Marshall-Smith syndrome: Follow-up report of a four and a half year old male
To the Editor:
I read with interest the report by Diab et al. [2003] entitled “Osseous fragility in Marshall–Smith syndrome” recently published in the journal. I share experience and follow-up of our previously reported patient with this rare syndrome [Summers et al., 1999]. Our patient was diagnosed with Marshall–Smith syndrome at 1-month of age due to advanced bone age, hypotonia, cranio-facial anomalies (prominent forehead, shallow orbits with ocular proptosis, micrognathia, flattened nasal bridge, anteverted nares and left choanal atresia, small ear canals) and failure to thrive. He weighed 3,025 g (5th centile), length was 58 cm (95th centile), and head circumference was 37 cm (50th centile). He required a tracheostomy during infancy due to choanal atresia and upper airway obstruction. A fundoplication was performed due to feeding difficulties and abnormal esophageal motility. Chromosome studies revealed a normal 46,XY karyotype. A skeletal survey at 1-month of age was significant for an estimated bone age of 3–4 years in the wrists, elbows and femoral epiphyses. A voiding cystogram showed a grade III vesicoureteral reflex on the left. An echocardiogram and electrocardiogram were normal. Normal blood chemistry and a normal hemogram were found.
At 4½ years of age, he weighed 17.7 kg (40th centile), height was 99 cm (5th centile), and head circumference was 53.6 cm (95th centile). He had a flattened occiput. He had broad appearing hands and feet with increased sweating bilaterally and limitation of range of motion of joints. His tracheostomy site was in place. He has had chronic ear infections since infancy with drainage and bilateral small external ear canals. His sclerae were blue (typically seen in patients with Marshall-Smith syndrome) and eyes were prominent. He wears glasses. His cardiovascular evaluation was normal while his neurological examination showed diminished tone overall and mildly hyper-reflexive extremities. He was not ambulatory and has delayed psychomotor development.
He has had three fundoplications and is fed by a gastrostomy tube. He had reconstructive facial surgery including upper orbital advancement at 15-months of age to correct the cranio-facial anomalies. Bone age at that time was 10 years. He later had a left diaphragmatic hernia repair. At 3½ years of age, his bone age was 11 years. X-ray studies also showed osteopenia, scoliosis and a callous formation in the mid-radius of the right arm with a fracture line. There was no report of trauma. Serum bone alkaline phosphatase levels were high (27 ng/ml; reference range: 1–24 ng/ml), and urinary N-telopeptide levels were also high (242 nm/mm creatinine; reference range: 10–65 nm/mm creatinine). Osteocalcin levels were normal as were general electrolytes. A skin biopsy was performed and fibroblast studies showed no biochemical or histological evidence of osteogenesis imperfecta. He has begun treatment with oral bisphosphonates. Since his last clinic visit, he has sustained a second non-traumatic fracture. This fracture occurred in his femur requiring surgery for stabilization and treatment. Figure 1 shows frontal views of our patient at 1½ years of age, 3½ years of age, and 4½ years of age.
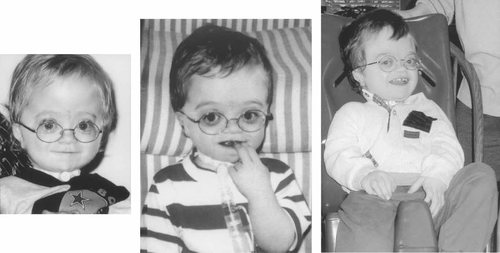
Frontal views of our patient with Marshall–Smith syndrome taken at 1½ years (left), 3½ years (middle), and 4½ years of age (right).
In summary, our patient with Marshall–Smith syndrome with non-traumatic fractures and blue sclerae further supports bone fragility in this rare syndrome. Healthcare providers should be aware that patients with this rare disorder may be at risk of increased bone fragility and fractures and should be treated accordingly.




