Donor age determines outcome in acute leukemia patients over 40 undergoing haploidentical hematopoietic cell transplantation
Abstract
Haploidentical hematopoietic cell transplantation (haplo-HCT) is being increasingly used in acute leukemia patients as an alternative transplant modality when matched sibling or matched unrelated donors are unavailable. As several potential haploidentical relative donors are typically available for a given patient, optimizing donor selection to improve clinical outcome is crucial. The impact of donor age and kinship on the outcome of acute leukemia patients is not clearly established in this setting. Using the multinational registry of the acute leukemia working party of the European society for blood and marrow transplantation we retrospective analyzed the clinical outcome of 1270 acute myeloid leukemia and acute lymphoblastic leukemia patients who underwent haplo-HCT between 2005 and 2015. Patients over the age of 40 were significantly affected by increasing donor age resulting in higher non-relapse mortality (NRM) [Hazard ratio (HR)=1.86, confidence interval (CI) 95%, 1.18-2.94; P = .007], inferior leukemia-free survival (LFS) (HR = 1.59, CI 95%, 1.13-2.24; P = .007), and overall survival (OS) (HR = 1.74, CI 95%, 1.22-2.47; P = .002) when donors were over the age of 40. Additionally, kinship was found to be prognostically significant as patients transplanted from children donors over the age of 35 experienced an increased rate of NRM (HR = 1.82, CI 95%, 1.13-2.9; P = .01), inferior LFS (HR = 1.5, CI 95%, 1.05-2.13; P = .03), and OS (HR = 1.5, CI 95%, 1.04-2.15; P = .03). For patients younger than 40 years, donor age and kinship were mostly not clinically impactful. Our data establish donor age and kinship as significant determinants of outcome following haplo-HCT for acute leukemia patients.
1 INTRODUCTION
With the introduction of innovative immunosuppression strategies enabling stem cell engraftment across broad HLA disparity, thus mitigating the incidence of lethal graft versus host disease (GVHD) and transplantation associated mortality and toxicity,1, 2 the routine implementation of haploidentical hematopoietic cell transplantation (haplo-HCT) is gaining considerable traction in hematological malignancies.3-5 The use of haplo-HCT affords the distinct advantage of a readily available related donor pool allowing for avoidance of the potentially hazardous delay caused by the search for matched unrelated donors. Initially however, this potential gain of haplo-HCT was counterbalanced by an increased risk of immune related complications. Notwithstanding these early concerns, several studies now report comparable outcomes following haplo-HCT and transplant from HLA matched sibling and unrelated donors.6-8 Accordingly, capitalizing on the relative abundance of possible donors available for prospective haplo-HCT patients, potentially allows for refinement of donor selection with the aim of matching patients with the most compatible donor. Whereas donor-specific HLA antibodies,9 ABO compatibility,10 and donor-recipient kinship11 have been clearly shown to affect outcome in diverse clinical settings in haplo-HCT, the impact of donor age on the outcome of acute leukemia patients is not as clearly established. A previously published single center analysis of patients with various hematological malignancies indicated that patients with young male donors experienced better outcomes,12 yet it remains unclear whether these results are applicable to acute leukemia patients and furthermore whether optimization of donor selection is affected by the age of patients as well as that of donors.
Herein, we present the EBMT acute leukemia working party experience with 1270 patients who underwent related haplo-HCT for acute leukemia. Our data show a clear dichotomy between patients over the age of 40 who decidedly benefited from age and kinship matching as opposed to younger patients for whom matching of age and kinship did not impact significantly on clinical outcome.
2 METHODS
2.1 Study design and data collection
The current analysis was a retrospective multicenter analysis performed by the Acute Leukemia Working Party (ALWP) of the European Society for Blood and Marrow Transplantation (EBMT). Quality control measures of the multicenter registry include confirmation of the validity of the entered data by the reporting team, cross-checking with the national registries, and regular in-house and external data audits. Eligibility criteria for the current study included adult patients with acute leukemia (i.e. AML, ALL) over the age of 18 who underwent a first T-cell replete related haplo-HCT from 2005 through 2015. Per study protocol, patients younger than 40 were included in the analysis if their donors were either parent or sibling, whereas patients over the age of 40 were included if their donors were either sibling or children. The list of participating institutions is available in the Supporting Information appendix. The study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines and approved by the ALWP institutional review board. All patients provided written informed consent authorizing the use of their personal information for research purposes.
2.2 Statistical analysis
The main endpoints of the study were non-relapse mortality (NRM), defined as death without previous relapse; relapse incidence (RI), defined on the basis of morphological evidence of leukemia in bone marrow or other extramedullary organs; leukemia-free survival (LFS), defined as the time from transplantation to first event (either relapse or death in complete remission); refined GVHD-free/relapse-free survival (GRFS), defined as survival without the following events: grade 3–4 acute GVHD, severe cGVHD, disease relapse, or death from any cause after Haplo-SCT13; and overall survival. Cumulative incidence curves were used for RI and NRM in a competing risks setting, since death and relapse are competing. Probabilities of OS, LFS, and GRFS were calculated using the Kaplan–Meier estimate. The probabilities of NRM, RI, acute and chronic GVHD were calculated using the cumulative incidence estimator to accommodate for competing risks.14 Univariate analyses were done using the Gray's test for cumulative incidence functions and the log rank test for OS, GRFS, and LFS. A Cox proportional hazards model was used for multivariate regression. Variables included in multivariate models were either significantly or unbalanced between the donor age groups, or known to have an impact on outcome studied. Results were expressed as the hazard ratio (HR) with the 95% confidence interval (95% CI). Proportional hazards assumptions were checked systematically for all proposed models using the Grambsch-Therneau residual-based test.
Initially we included both donor age and kinship as continuous variables in the Cox regression model. As the assumption of log-linearity (linearity between HR in each quintiles of donor age and outcome) was not verified, we categorized donor age using a cutoff of 40 years as planned in the protocol. Since donor age was related to kinship in the two cohorts of patients (over or under the age of 40), we also investigated the association between donor age and outcome in 4 groups of patients: 1. patients less than 40 years of age transplanted from a parent; 2. patients under the age of 40 transplanted from a sibling; 3. patients over 40 years of age transplanted from a child; 4. patients more than 40 years of age transplanted from a sibling. In each group, we then determined the optimal threshold of donor age (i.e. best predictor of clinical outcome) using methodology previously described by Hothorn and Zeileis.15
All tests were two-sided with the type I error rate fixed at 0.05. Statistical analyses were performed with SPSS 22.0 (SPSS Inc, Chicago, IL, USA) and R 3.2.3 (R Development Core Team, Vienna, Austria) software packages.
3 RESULTS
3.1 Patient characteristics
In all, 1270 patients underwent haploidentical HCT between 2005 and 2015, of whom 700 were transplanted at age 40 or over and 570 were transplanted at an age less than 40. Median follow-up for patients in this analysis was 27 months (range 0.6–119 months). Patient, disease and transplant characteristics are summarized in Table 1.
| Variable, n (%) | Patient age < 40 (n = 570) | Patient age > 40 (n = 700) | P |
|---|---|---|---|
| Follow up duration in m, median (range) | 30 (0.62–119.3 ) | 24 (0.89–102.16 ) | <.001 |
| Patient age in y, median (range) | 27 (18–40) | 55 (40–77) | <.001 |
| Donor age in y, median (range) | 43 (13–72) | 36 (13–71) | <.001 |
| Gender | 0.16 | ||
| Male | 348 (61.1) | 401 (57) | |
| Female | 221 (38.8) | 299 (42.7) | |
| Year of transplant, median (range) | 2012(2005–2015) | 2013(2005–2015) | <.001 |
| AML | 400 (70.1) | 619 (88.4) | <.001 |
| ALL | 170 (29.8) | 81 (11.5) | |
| Disease status at transplant | <0.001 | ||
| CR1 | 325 (57) | 324 (46.2) | |
| CR2/3 | 125 (21.9) | 124 (17.7) | |
| Active disease | 120 (21) | 252 (36) | |
| ELN AML cytogenetic risk category | <0.001 | ||
| Favorable | 39 (11.9) | 27 (5.6) | |
| Intermediate | 236 (72.1) | 322 (67.6) | |
| Adverse | 52 (15.9) | 127 (26.6) | |
| Missing | 73 | 143 | |
| ALL Philadelphia chromosome status | 0.001 | ||
| Negative | 68 (51.5) | 17 (26.1) | |
| Positive | 64 (48.4) | 48 (73.8) | |
| Missing | 37 | 16 | |
| Donor-patient kinship | <0.001 | ||
| Parent | 298 (52.2) | 0 | |
| Child | 0 | 440 (62.8) | |
| Sibling | 272 (47.7) | 260 (37.1) | |
| Donor-recipient gender matching | .031 | ||
| Male-Male | 184 (32.3) | 248 (35.4) | |
| Female-Male | 164 (28.8) | 153 (21.8) | |
| Male-Female | 118 (20.7) | 171 (24.4) | |
| Female-Female | 103 (18.1) | 128 (18.2) | |
| CMV Donor-recipient matching | <0.001 | ||
| CMV D-/R- | 62 (11.1) | 97 (14.1) | |
| CMV D+/R- | 34 (6.1) | 27 (3.9) | |
| CMV D-/R+ | 49 (8.8) | 164 (23.9) | |
| CMV D+/R+ | 409 (73.8) | 397 (57.9) | |
| Missing | 16 | 15 | |
| T-cell depletion in-vivo | <.001 | ||
| Yes | 321 (56.4) | 247 (35.4) | |
| No | 248 (43.5) | 449 (64.5) | |
| Missing | 1 | 4 | |
| Use of PTCy | <.001 | ||
| Yes | 240 (42.4) | 425 (61) | |
| No | 325 (57.5) | 271 (38.9) | |
| Missing | 5 | 4 | |
| Stem cell source | <0.001 | ||
| Bone marrow derived graft | 171 (30) | 290 (41.4) | |
| Peripheral blood graft | 203 (35.6) | 360 (51.4) | |
| Bone marrow and peripheral blood | 196 (34.3) | 50 (7.1) | |
| Engraftment | 0.015 | ||
| Succesful engraftment | 495 (94.2) | 556 (90.4) | |
| Engraftment failure | 30 (5.7) | 59 (9.5) | |
| Missing | 45 | 85 | |
| Conditioning regimen | <0.001 | ||
| Myeloablative | 426 (74.7) | 287 (41) | |
| Reduced intensity | 144 (25.2) | 413 (59) | |
- AML, acute myeloid leukemia; ALL, acute lymphoblastic leukemia; CMV, cytomegalovirus; ELN, European LeukemiaNet; PTCy, post-transplant cyclophosphamide.
3.2 Transplant outcomes
At 2 years of follow-up for the entire cohort, LFS and RI rates were 43.6% (95% CI: 40.7–46.5) and 28.9% (95% CI: 26.3–31.5), respectively. The 2 year incidence of grade II-IV acute GVHD and chronic GVHD were 30.7% (95% CI: 28.1–33.3) and 31.2% (95% CI: 28.5–33.9), respectively. The rate of NRM was 27.3% (95% CI: 24.8–29.8) while the 2 year OS was 48.8% (95% CI: 45.8–51.7). The 2 year rate of GRFS was 34.9% (95% CI: 32.1–37.7). Leukemia relapse, infection, and GVHD were the main etiologies for patient death both in patients under and over the age of 40 (Supporting Information Table S1).
3.3 Impact of donor age on patient outcome in patients over the age of 40
To determine the differential impact of donor age on patient outcome, we proceeded with a separate analysis for patients over and under the age of 40. As shown in Supporting Information Table S2 which summarizes the baseline characteristics of patients over the age of 40, patients with younger donors tended to be older (57 vs. 53; P = .032) whereas donors younger than 40 years of age were for the most part children of the patients (91% vs. 19%; P < .001) as opposed to older donors who were mostly siblings (80% vs. 8%; P < .001). Next, a univariate analysis comparing the clinical outcomes of patients in this age group was carried out to determine whether outcome differed among patients with donors over and under the age of 40, and according to donor kinship, namely sibling donor versus child donor. As shown in Supplementary Table S3, patients with younger donors experienced improved LFS and OS rates compared to their counterparts with older donors (41% vs. 32%; P = .03, and 45% vs. 35%; P = .01, respectively). In this age group of patients over 40, kinship did not impact on patient outcome in a statistically significant manner, thus patients had comparable outcomes whether they were transplanted from their sibling or child.
We then carried out a multivariate analysis (Table 2) which revealed that patients older than 40 experienced increased NRM (HR = 1.86, CI 95%, 1.18-2.94; P = .007) as well as inferior LFS (HR = 1.59, CI 95%, 1.13-2.24; P = .007), OS (HR = 1.74, CI 95%, 1.22-2.47; P = .002), and GRFS (HR = 1.6, CI 95%, 1.16-2.22; P = .004) rates when donor age was more than 40 years of age.
| RI | NRM | LFS | OS | GRFS | Grade II-IV aGVHD | cGVHD | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | CI | P | HR | CI | P | HR | CI | P | HR | CI | P | HR | CI | P | HR | CI | P | HR | CI | P | |
| Donor Age > 40y | 1.30 | 0.779-2.165 | .32 | 1.87 | 1.182-2.945 | .007 | 1.59 | 1.134-2.24 | .007 | 1.74 | 1.223-2.475 | .002 | 1.61 | 1.162-2.227 | .004 | 1.40 | 0.823-2.376 | .22 | 1.39 | 0.778-2.469 | .27 |
| Patient age (per 10y) | 0.80 | 0.621-1.021 | .07 | 1.08 | 0.851-1.369 | .529 | 0.93 | 0.782-1.103 | .40 | 0.95 | 0.798-1.129 | .56 | 0.85 | 0.722-1 | .05 | 0.79 | 0.619-1.008 | .06 | 0.89 | 0.682-1.173 | .42 |
| ALL vs. AML | 1.32 | 0.811-2.137 | .27 | 1.32 | 0.833-2.094 | .237 | 1.29 | 0.925-1.808 | .13 | 1.26 | 0.893-1.77 | .19 | 1.22 | 0.884-1.672 | .23 | 0.94 | 0.566-1.567 | .82 | 1.04 | 0.608-1.785 | .88 |
| KPS > 80% | 0.82 | 0.517-1.303 | .40 | 0.64 | 0.411-1.006 | .053 | 0.74 | 0.539-1.027 | .07 | 0.68 | 0.488-0.939 | .02 | 0.64 | 0.471-0.881 | .006 | 0.78 | 0.477-1.269 | .31 | 0.44 | 0.252-0.781 | .00 |
| Sibling vs. children | 0.82 | 0.448-1.489 | .51 | 0.64 | 0.367-1.097 | .10 | 0.71 | 0.473-1.065 | .10 | 0.69 | 0.453-1.04 | .08 | 0.65 | 0.44-0.95 | .026 | 0.73 | 0.4-1.344 | .32 | 0.75 | 0.389-1.456 | .40 |
| RIC vs. MAC | 1.38 | 0.971-1.968 | .07 | 1.09 | 0.785-1.522 | .60 | 1.22 | 0.957-1.556 | .11 | 1.19 | 0.928-1.526 | .17 | 1.25 | 0.99-1.577 | .06 | 1.08 | 0.767-1.526 | .65 | 1.00 | 0.679-1.461 | .98 |
| PB vs. BM stem cell source | 0.82 | 0.559-1.19 | .29 | 1.27 | 0.894-1.798 | .18 | 1.04 | 0.798-1.348 | .79 | 1.01 | 0.775-1.31 | .96 | 1.16 | 0.906-1.481 | .24 | 1.77 | 1.267-2.467 | <.0001 | 1.45 | 0.935-2.239 | .10 |
| Female patient vs. male | 1.37 | 1.004-1.871 | .047 | 1.01 | 0.748-1.367 | .94 | 1.18 | 0.949-1.462 | .14 | 1.08 | 0.866-1.353 | .49 | 1.04 | 0.843-1.277 | .73 | 0.93 | 0.678-1.283 | .67 | 1.31 | 0.921-1.863 | .13 |
| Female donor vs. male | 0.73 | 0.532-1.006 | .055 | 0.97 | 0.714-1.309 | .83 | 0.84 | 0.677-1.05 | .13 | 0.86 | 0.684-1.076 | .18 | 0.89 | 0.718-1.093 | .26 | 1.16 | 0.849-1.59 | .35 | 1.06 | 0.744-1.501 | .76 |
- RIC, reduced intensity conditioning; MAC, myeloablative conditioning; PB, peripheral blood; BM, bone marrow.
3.4 Focused assessment of optimal donor subsets for patients over the age of 40
To better characterize the specific patient subsets which would benefit from specific donor pools, we made use of methodology previously described by Hothorn and Zeileis,15 allowing us to determine that the optimal discriminating age cutoff for prognostication was 35 years and 41 years for children donors and sibling donors, respectively. As shown in Supplementary Figure S1 and Table S4, patients transplanted from their children had inferior NRM, LFS, OS, and GRFS rates when the donors' age was over 35. In the multivariate analysis presented in Table 3, transplantation from children donors over the age of 35 was associated with an increased risk of NRM (HR = 1.82, CI 95%, 1.13-2.9; P = .01), inferior LFS (HR = 1.5, CI 95%, 1.05-2.13; P = .03), and inferior OS (HR = 1.5, CI 95%, 1.04-2.15; P = .03). Subsequently, we performed univariate and multivariate analyses for patients transplanted from sibling donors with age 41 as the cutoff. While a univariate analysis indicated that using a sibling donor over the age of 41 was associated with inferior NRM, LFS, and OS rates, the multivariate analysis summarized in Supporting Information Table S5, did not confirm the statistical significance of these associations.
| RI | NRM | LFS | OS | GRFS | Grade II-IV aGVHD | cGVHD | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | CI | P | HR | CI | P | HR | CI | P | HR | CI | P | HR | CI | P | HR | CI | P | HR | CI | P | |
| Donor Age > 35y | 1.15 | 0.683-1.941 | .60 | 1.82 | 1.137-2.907 | .01 | 1.50 | 1.051-2.139 | .03 | 1.50 | 1.049-2.151 | .03 | 1.38 | 0.978-1.934 | .067 | 1.04 | 0.623-1.748 | .87 | 1.03 | 0.584-1.808 | .92 |
| Patient age (per 10y) | 0.82 | 0.587-1.146 | .25 | 0.91 | 0.66-1.257 | .57 | 0.86 | 0.676-1.095 | .22 | 0.95 | 0.742-1.205 | .65 | 0.81 | 0.644-1.016 | .068 | 0.97 | 0.692-1.372 | .88 | 1.18 | 0.82-1.69 | .38 |
| ALL vs. AML | 1.44 | 0.733-2.816 | .29 | 1.22 | 0.621-2.39 | .57 | 1.31 | 0.808-2.135 | .27 | 1.36 | 0.835-2.227 | .22 | 1.19 | 0.743-1.907 | .47 | 0.92 | 0.432-1.95 | .82 | 0.91 | 0.4-2.06 | .82 |
| KPS > 80% | 1.15 | 0.636-2.077 | .65 | 1.26 | 0.759-2.098 | .37 | 1.21 | 0.813-1.801 | .35 | 1.27 | 0.851-1.904 | .24 | 1.23 | 0.845-1.789 | .28 | 1.13 | 0.651-1.962 | .66 | 1.29 | 0.747-2.24 | .36 |
| Active disease vs. CR1 | 0.72 | 0.399-1.287 | .26 | 0.53 | 0.302-0.919 | .02 | 0.65 | 0.432-0.988 | .04 | 0.60 | 0.39-0.908 | .02 | 0.48 | 0.321-0.72 | .0004 | 0.53 | 0.293-0.971 | .04 | 0.50 | 0.255-0.984 | .045 |
| RIC vs MAC | 1.16 | 0.739-1.811 | .52 | 1.55 | 1.003-2.399 | .049 | 1.41 | 1.016-1.951 | .04 | 1.40 | 1.003-1.94 | .048 | 1.60 | 1.171-2.192 | .0032 | 1.13 | 0.726-1.772 | .58 | 1.17 | 0.74-1.851 | .50 |
| PB vs. BM stem cell source | 0.84 | 0.519-1.358 | .48 | 1.24 | 0.799-1.908 | .34 | 1.09 | 0.751-1.566 | .66 | 1.06 | 0.743-1.51 | .75 | 1.09 | 0.766-1.552 | .63 | 1.39 | 0.924-2.084 | .11 | 1.49 | 0.969-2.297 | .069 |
| Female patient vs. male | 1.44 | 0.972-2.143 | .07 | 1.13 | 0.774-1.65 | .53 | 1.29 | 0.977-1.711 | .07 | 1.25 | 0.935-1.661 | .13 | 1.14 | 0.869-1.495 | .34 | 1.09 | 0.717-1.656 | .69 | 2.00 | 1.275-3.134 | .003 |
| Female donor vs. male | 0.75 | 0.497-1.124 | .16 | 1.12 | 0.766-1.64 | .56 | 0.89 | 0.668-1.178 | .41 | 0.92 | 0.687-1.232 | .58 | 0.95 | 0.724-1.253 | .73 | 1.11 | 0.738-1.671 | .62 | 0.82 | 0.528-1.263 | .36 |
- RIC, reduced intensity conditioning; MAC, myeloablative conditioning; PB, peripheral blood; BM, bone marrow.
3.5 Impact of donor age on patient outcome in younger patients under the age of 40
The baseline characteristics of the subgroup of patients under the age of 40 are summarized in Supporting Information Table S6. Patients with younger donors tended to be older (29 years vs. 25 years; P < .0001) whereas patients with younger donors were more likely to have male donors as opposed to older donors who tended to be females (P = .001). Next, a univariate analysis was performed to evaluate the impact of donor age and donor kinship on clinical outcome. As shown in Supporting Information Table S7, the risk for grade II-IV acute GVHD was markedly increased in patients whose donors were over the age of 40 compared to patients with younger donors (38% vs. 28%; P = .014). The only clinical outcome affected by kinship was the incidence of grade II-IV acute GVHD which was significantly higher in patients with parent donors compared to patients transplanted from their siblings (38% vs. 28%; P = .017). The multivariate analysis shown in Supporting Information Table S8 revealed that in patients under the age of 40, having a donor over the age of 55 was independently associated with a decreased risk for extensive chronic GVHD (HR = 0.17, CI 95%, 0.02-0.95; P = .045) concomitant with a trend for an increased risk of relapse (HR = 1.85, CI 95%, 0.97-3.49; P = .058).
3.6 Focused assessment of optimal donor subsets for patients younger than 40
In line with the subgroup analysis performed above, we wanted to determine specifically in younger patients whether donor age affected prognosis with respect to kinship. In this patient age group it was determined that for parent donors, the optimal cutoff age was 51, and as summarized in Supporting Information Table S9, a multivariate analysis indicated that when donor age was more than 51 years of age, there was a trend towards increased RI (HR = 1.82, CI 95%, 0.97-3.38; P = .06) and LFS (HR = 1.6, CI 95%, 0.98-2.58; P = .057) rates. The equivalent analysis in sibling donors did not reveal any significant associations with donor age for this group of patients (data not shown). Figure 1 outlines LFS and OS of patients according to patient and donor age.
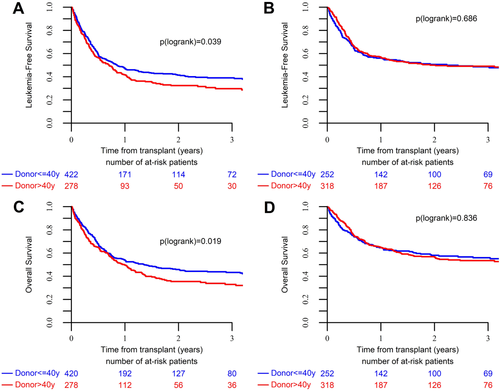
Transplantation outcomes of acute leukemia patients stratified per patient and donor age. (A) Leukemia free survival in patients over the age of 40. (B) Leukemia free survival in patients under the age of 40. (C) Overall survival in patients over the age of 40. (D) Overall survival in patients under the age of 40. [Color figure can be viewed at wileyonlinelibrary.com]
4 DISCUSSION
As haplo-HCT is transitioning into the mainstream of the stem cell transplantation field, choosing the best available donor is becoming a major priority. Our data suggest age 40 as a prognostically meaningful threshold with significant practical implications for patients, wherein patients over the age of 40 may benefit from a younger donor especially when the donor is their child. Conversely, we show that for patients under the age of 40, donor age for the most part is not as clinically significant.
Recently published donor selection algorithms for haplo-HCT16-18 have designated a myriad of clinical,11, 12 serological,9, 10, 19 and immunological20 parameters constituting the backbone for optimal donor selection in this setting. Whereas most of these have not been rigorously validated for haplo-HCT, a particular emphasis has been placed on donor age as this parameter is readily available and potentially modifiable when considering a specific donor from a potential donor pool consisting of several siblings and children. The theme of donor age has been extensively investigated in hematopoietic cell transplantation in the past three decades with data generally confirming that patients receiving grafts from younger donors experience superior survival21-25 concomitant to a decreased incidence of acute and chronic GVHD.26, 27
Our analysis shows that in patients over the age of 40, having an older donor, namely over the age of 40, is tightly associated with increased NRM and inferior LFS translating into inferior OS. Moreover, in this age group we established kinship to be a major determinant of patient outcome as increasing donor age did not affect outcome when patients were transplanted from their siblings whereas those patients receiving grafts from their children did experience worse outcome when their donor was over the age of 35. Our findings are generally in line with those of Wang and colleagues12 with several noteworthy exceptions. In contrast to their results we did not find male gender to be significantly associated with superior clinical outcome, nor did we observe children donors to be superior to sibling donors in terms of GVHD. These differences may be accounted for by considering several factors: our analysis was restricted to a uniform cohort of acute leukemia patients whereas theirs consisted of a mixed cohort which comprised a substantial segment of patients with diseases other than acute leukemia. Additionally, post-transplantation cyclophosphamide was widely used for patients in our analysis while the Chinese analysis uniformly used ATG for T-cell depletion.
Interestingly, we found that for younger patients, donor age and kinship were not as clinically impactful. The only clear association in this age group pertained to a decreased rate of extensive chronic GVHD when donors were over the age of 55, an observation which diverges from previously published data in matched unrelated donors.21, 26 The reasons for this observation are not completely clear but we note that as part of the aging process there is an increase in the number of peripheral blood CD4+CD25+ regulatory T cells, as shown previously in healthy volunteers,28 which may attenuate immune responsiveness and result in decreased GHVD.
We believe that the implications of our findings are of importance for future donor selection algorithms in haplo-HCT and will guide clinicians in making a rationale determination of the optimal donor for a specific patient. Furthermore, our findings underscore the unique immunological milieu of haplo-HCT where considerations need to be made regarding donor-recipient rapports between patients, their children, siblings, and parents.
As with any multicenter registry analysis, our results should be interpreted cautiously owing to inherent biases in data collection and variations in clinical practice among participating institutions. Additionally, we note that the group of patients over the age of 40 who were transplanted from younger donors (under the age of 41) consisted of only 47 patients and thus the lack of statistical significance (P = .06) with regard to OS and LFS may have resulted from the lack of sufficient statistical power.
In aggregate, the key findings of this analysis uncover an additional facet of the complexities involved in providing the best outcome for acute leukemia patients undergoing haplo-HCT, and will hopefully further inform the maturing field of haploidentical transplantation.
ACKNOWLEDGMENTS
We thank all the European Group for Blood and Marrow Transplantation (EBMT) centers and national registries for contributing patients to the study and data managers for their excellent work.