Cutaneous involvement by post-polycythemia vera myelofibrosis
Conflict of interest: Nothing to report
A 69-year-old man presented with multiple skin lesions scattered across his thorax and abdomen that had appeared 3 months earlier. He had a 20-year history of polycythemia vera with homozygosity for JAK2 V617F and was treated with hydroxyurea and aspirin since diagnosis. Skin lesions were macular to papulo-nodular, reddish to purple, up to 3 cm in diameter (Image 1A), and hard on palpation. The patient denied they were itchy or painful. Apart from that, physical examination was notable only for mild hepatosplenomegaly. Blood cell count showed leukocytosis (WBC 14.3 × 109/L) with hemoglobin concentration and platelet count within normal limits. Peripheral blood smear was characterized by red cell anisopoikilocytosis with dacryocytosis, and leukoerythroblastic picture with 2% micromegakaryocytes and 1% blasts. Ultrasonografy showed that spleen major diameter was 13.5 cm.
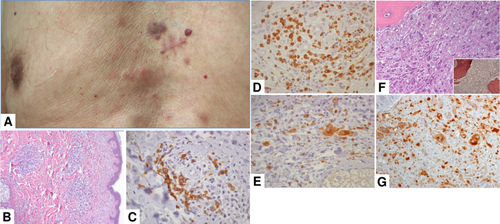
A punch biopsy of a thoracic skin nodule demonstrated a dermal perivascular and periadnexal infiltrate with mild interstitial fibrosis (Image 1B, HE, 20×) composed by glycophorin C+ erythroblasts (Image 1C, 60×) immature MPO+ granulopoietic elements (Image 1D, 40×), and dysmorphic LAT+ megakaryocytes (Image 1E, 60×), without CD34+ or CD117+ blasts. A diagnosis of post-polycythemia vera myelofibrosis was established on the concurrent bone marrow biopsy (Image 1F,G) 1 and the trilineage hemopoiesis observed on the cutaneous biopsy was consistent with a neoplastic skin involvement by the disease.
Cutaneous involvement has been reported in a few patients with myelofibrosis 2-4 and was associated with progressive disease and very poor prognosis 3. Our patient was asymptomatic and, apart from development of the skin lesions, had no signs of progressive disease, and we, therefore, did not modify his treatment. After a 15 months follow-up, his clinical and hematological picture is stable and the skin lesions show no modifications in size or number. This suggests that cutaneous involvement by myelofibrosis should not be always regarded as a manifestation of the terminal phase of the disease.
The observation in adult patients of extramedullary trilineage hemopoiesis, even in absence of blasts, should always rise the suspect of a neoplastic proliferation, which is usually expression of a underlying myeloid proliferation, especially chronic myeloproliferative diseases 5: thus, as in our case, it is important to integrate the extramedullary findings with clinical picture and results of bone marrow biopsy.