Infected liver cysts resulting from ascending cholangitis and cancer of the ampulla of Vater: A case report
Abstract
Infected liver cysts may have a unique etiology and require further workup. Generally, large cyst is easy to be symptomatic. In contrast, smaller cyst with infection in our case is associated with ampullar cancer of Vater without typical manifestations of jaundice, body weight loss, and pancreatitis. We presented the case of a 61-year-old man with infected liver cysts, which is confirmed by abdominal computer tomography and liver cysts drainage with bacterial culture. Endoscopic retrograde cholangiopancreatography revealed a swollen papilla of Vater and a dilated common bile duct. Biopsy confirmed adenocarcinoma of the ampulla of Vater. Further surgical pathology revealed communication of bile duct with liver cysts and no evidence of tumor invasion to pancreatic duct and common bile duct. The infected liver cysts may result from ascending cholangitis which is secondary to ampullar cancer. The patient underwent the Whipple procedure, unroofing of the right-side liver cyst, and partial hepatectomy without complications. There is no recurrence of infected liver cyst and cancer till now after follow-up for 3 years. Infected liver cysts are rarely associated with ampullar cancer. Early diagnosis and successful resection of early stage ampullary neoplasm ensure favorable outcomes.
1 INTRODUCTION
Most liver cysts are incidentally discovered and typically asymptomatic. Liver cysts may be symptomatic when they become infected after trauma or therapeutic procedures, communicate with the biliary tract, or develop in immunocompromised hosts, such as patients with diabetes mellitus.1 Cholangitis resulting from cancer of the ampulla of Vater is common. However, infected liver cysts resulting from ascending cholangitis, which is secondary to ampullary cancer, have not been reported. This report presents the case of a 61-year-old man with an infected liver cyst, ascending cholangitis, and cancer of the ampulla of Vater, which was detected in duodenoscopy.
2 CASE REPORT
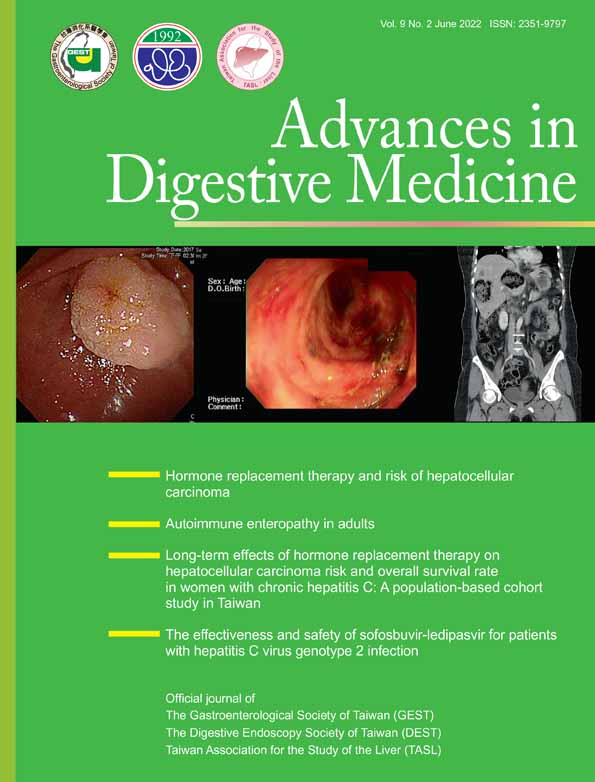
A 61-year-old man was admitted to Ditmanson Medical Foundation Chiayi Christian Hospital with fever and severe epigastralgia for the last 4 days. He had no history of surgery or trauma, and he denied having major systemic diseases such as diabetes mellitus, heart disease, or pulmonary disorders. No history of jaundice or weight loss was noted. During physical examination, the patient's body temperature was 38.2°C. The conjunctivae was not pale, and the sclera was not icteric. Only epigastric tenderness was noted. Murphy's sign was negative, and the liver and spleen were impalpable. A laboratory examination indicated normal levels of total bilirubin (0.82 mg/dL, normal: 0.2-1.2 mg/dL), aspartate transaminase (20 U/L, normal: 8-38 U/L), alanine transaminase (17 U/L, normal: 4-44 U/L), alkaline phosphatase (282 U/L, normal: 104-338 U/L), and lipase (15.8 U/L, normal: 13-60 U/L). A hemogram indicated leukocytosis (22 050/cumm) and a normal hemoglobin level. The differential count was normal. The patient's C-reactive protein level was elevated (22.948, normal: 0-0.3 mg/dL), and his serum carbohydrate antigen (CA 19-9) level was within the normal range (15.38, normal: 0-37 U/mL). A blood culture revealed no growth. Abdominal computed tomography (CT) revealed multiple cysts of various sizes in both lobes of the liver. The largest cyst, found in the right lobe of the liver, reached 15 cm in diameter. Multiple small cysts with peripheral enhancement were noted in the left lobe with a dirty fat plane at the periphery (Figure 1). Percutaneous drainage was performed on the liver cysts in both hepatic lobes. The cyst content in the right lobe was clear with no bacterial growth after culturing. Drainage from the cysts in the left lobe was turbid, and Klebsiella pneumoniae was cultured from its content. Fever subsided after drainage and administration of antibiotics. Esophagogastroscopy (EGD) revealed a gastric ulcer and a prominent ampulla of Vater. Biopsy from the ampulla of Vater revealed villous adenoma with low-grade dysplasia. Side-viewing duodenoscopy for endoscopic retrograde cholangiopancreatography (ERCP) revealed a swollen ampulla of Vater with normal passage of bile (Figure 2). Mild dilatation of the common bile duct was observed through cholangiography (Figure 3). Repeat biopsy of the ampulla of Vater indicated adenocarcinoma.


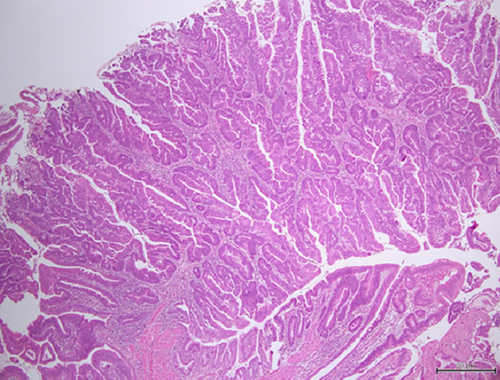
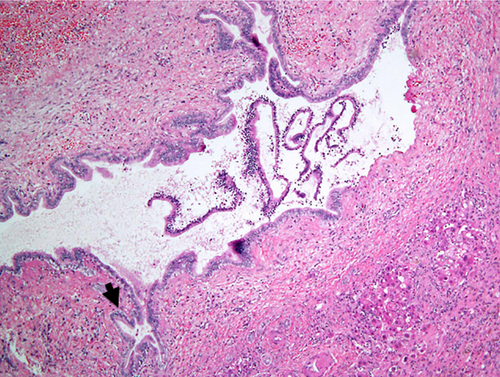
The patient underwent the Whipple procedure, unroofing of the right liver cyst, and partial hepatectomy of the left lobe. The surgical specimen revealed a small tumor 1 cm in diameter in the ampulla of Vater. The common bile duct was dilated. The cyst in the left lobe communicated with intrahepatic ducts and had turbid content. No stones or stenosis were discovered in the common bile duct or gall bladder. Pathology confirmed adenocarcinoma in the tubulovillous adenoma of the ampulla of Vater (Figure 4). The cancer was limited to the lamina propria and submucosa. No lymph node metastasis was detected. Final surgical pathology staging was stage: ΙA (T1aN0M0). The cyst was lined with a single layer of columnar epithelium and communicated with a bile duct (Figure 5). The patient recovered well after operation.
3 DISCUSSION
Liver cysts may cause complications such as hemorrhage,1 infection,2 rupture into the peritoneal cavity3 or bile ducts,4 and compression of the biliary tract.5 Liver cysts in symptomatic patients are larger than those in asymptomatic patients.6 In contrast, smaller cysts over the left lobe infected with K. pneumoniae raised suspicions of an underlying etiology in the biliary tract. ERCP revealed a swollen ampulla of Vater with mild dilatation of the common bile duct. The ampullary tumor caused ascending cholangitis, resulting in infection in the liver cysts of the left lobe.
Acute cholangitis has long been diagnosed on the basis of Charcot's triad previously, but it is low sensitivity (26%) in despite of high specificity. According to Tokyo guidelines 2018 for diagnosis criteria of acute cholangitis, our case showed fever, leukocytosis and high CRP associated with biliary dilatation but lacked of jaundice and abnormal liver function. So, acute cholangitis was highly “suspected.”
Most patients with ampullary cancer present symptoms of obstructive jaundice, pancreatitis, weight loss, and abdominal pain.7 However, early diagnosis of ampullary cancer in our patient was difficult because of the small tumor size, anicteric course, and normal biliary and pancreatic enzyme levels. Moreover, CT revealed no evidence of the double duct sign in our patient, except for mild dilatation of the common bile duct without changes in the main pancreatic duct. Reconstruction CT with simultaneous air inflation into the duodenal lumen and magnetic resonance cholangiopancreatography may be helpful for diagnosis.8 EGD revealed a suspicious ampullary tumor, which was confirmed to be adenocarcinoma through duodenoscopy with biopsy during ERCP.9 The rationale of ampullary cancer, ascending cholangitis, and resultant liver cyst infection was finally confirmed during surgery.
The preferred procedure for symptomatic simple cysts is laparoscopic wide unroofing. However, the Whipple procedure was performed in this case because ampullary cancer was present. The pathogenesis of liver cyst infection due to ampullary cancer is based on sphincter of Oddi dysfunction and repeated cholangitis, even in cases without evidence of bile duct obstruction. Liver cyst with infection could occur through biliary tract or blood stream. The most likely source is from biliary system. Connection between liver cysts and biliary system might occur if some reasons such as cholangitis induce increase of the pressure of the intrahepatic duct.10
ERCP and further surgery verified the dilatation of the common bile duct, ascending cholangitis, and communication of bile ducts with infected liver cysts. A favorable prognosis was anticipated for our patient because of the absence of jaundice at the time of diagnosis, limited tumor invasion into the submucosa layer, and no lymph node involvement.11
In conclusion, infected liver cysts associated with ampullary cancer are rare. However, infection of microorganisms to hepatic cyst showed the relatively high proportion of a biliary route of infection (42%). Duodenoscope and even ERCP are indicated after excluding other underlying etiology of infected liver cyst.12 The unusual infection in the liver cysts and ascending cholangitis with dilatation of the biliary tree without stones raised suspicion of ampullary lesions. Early diagnosis and successful resection of early stage ampullary neoplasm ensure favorable outcomes.
ACKNOWLEDGMENTS
This manuscript was edited by Wallace Academic Editing.
CONFLICT OF INTEREST
The authors declare no conflict of interest.