Chinese expert consensus on the application of comprehensive geriatric assessment for the elderly
Abstract
Comprehensive geriatric assessment is the major approach in screening geriatric syndrome. The aim of this expert consensus is to supply standard operating procedures for clinical practice of comprehensive geriatric assessment in China.
1 INTRODUCTION
Comprehensive geriatric assessment (CGA) refers to the use of a multidisciplinary approach in assessing the physical condition, functional status, mental health, and social environment of the elderly, followed by treatment plans developed to maintain and improve their health and functional status and maximize their quality of life. CGA is one of the core elements in modern geriatric medicine and is an effective approach in screening geriatric syndrome. Generally, most of the geriatricians in China lack knowledge on comprehensive evaluation for elderly patients, and there is no available standard operating procedure for clinical practice. This consensus is prepared in accordance with international guidelines and is adjusted to the Chinese context in order to provide guidance in implementing CGA.
2 OVERVIEW OF CGA
Comprehensive geriatric assessment is applicable to people aged more than 60 years who experience activity insufficiency, functional impairment, recent deterioration, multiple medication prescriptions, geriatric syndrome, medical comorbidities, mental problems, and lack of social support. For those with end-stage illness, severe illness, severe dementia, and complete disability, as well as for some elderly people in good health, CGA can be conducted partially. It is recommended that CGA is performed by full-time staffs qualified with the skills in conducting CGA or by geriatric multidisciplinary-team members, such as geriatricians, clinical dietitians, rehabilitation therapists, clinical pharmacists, nurse specialists, and psychiatrists. CGA may have different focuses when performed by assessors in different health professions and according to the situation of the patient. Therefore, the time required to complete the assessment and the purposes of the CGA may also differ. It is recommended that general hospitals and geriatric hospitals should develop systematic CGA programs to assess the general conditions, comorbidities, use of multiple medications, physical function, mental and psychological status, cognitive function, nutritional status, and social support for the elderly patients. The comprehensive version of the CGA software is recommended to be used in a hospital setting. In a community setting, the simplified version of the CGA software is recommended. Some validated short forms are adopted in the simplified version. In expert opinions, the purpose of the CGA is to facilitate the diagnostic process of geriatric syndrome, and is regarded as an efficient observation indicator in treating elderly patients.
3 CONTENT OF CGA
3.1 General information
Information on the patient's name, gender, age, marital status, height, weight, alcohol and tobacco use, education status, occupation, and hobby is collected.
3.2 Function status
Assessments of function status are to assess patients’ ability to perform activities of daily living, balance and gait problems, and risk for fall.
3.2.1 Activities of daily living
An elderly patient's functional status can be assessed by basic activities of daily living (BADL) and instrumental activities of daily living (IADL). BADL refers to self-care activities and the ability to perform functional activities, which can be assessed by direct observations or interviews. The Barthel Index is the most widely used, most studied, and most reliable instrument in evaluating BADL in clinical practice.1 The Modified Barthel Index (MBI) is developed in accordance with Chinese context and has been widely used in the field of rehabilitation medicine.2 Be aware of the following points when using the MBI: (i) The assessment should be performed at an appropriate time in a safe environment and started with simple tests; (ii) Basically, assess the patient by direct observation. In other aspects, ask patients or their family members questions when needed; (iii) Assess the patient's actual ability and record it accordingly. Patients are categorized as self-care as long as they are able to perform the activities without others’ help, even with assistive devices; and (iv) The assessment results reflect the patient's situation within the past 24 hours. In a community setting, the Lawton Scale for IADLs is used to assess IADL.3 The following points should be paid attention to when using the scale: (i) Before the assessment, the purpose of the test should be fully discussed with the patient; (ii) According to the scale, questions are asked one by one or determined according to the observations of family members and nursing staffs; (iii) If the item fails to be assessed, record it elsewhere; and (iv) The assessment results are evaluated based on performance in the past month.
3.2.2 Gait and balance
One of the most commonly used gait and balance assessment tools in outpatient setting is the Timed Up and Go test (TUG).4 But when compared to the Tinetti assessment tool, the latter is more widely used internationally with higher reliability and validity, and can better assess the patient's balance function.5, 6 Before the test, the following items should be prepared: (i) The test should be performed in a clean and bright environment; (ii) The walking surface for the test should be nonslip and smooth; (iii) Prepare a solid armless chair, an evaluation table, pens, gait bands, and a timer for the test; (iv) Ask the patient to wear light clothes before the test; and (v) Inform the patient about the entire process of the test and provide support when necessary. During the test, always stand by the patient and be prepared to help stabilize the patient to prevent a fall. Help the patient to sit in the chair if the patient falls. Use gait belts when needed, and try to complete the test without assistive devices as much as possible.
3.2.3 Morse Fall Scale7, 8
The Morse Fall Scale is designed to assess the fall risk of hospitalized elderly patients specifically. When using the scale, ask patients about their history of falls. Ask a family member or caregiver if patients are unwilling to answer or present with cognitive dysfunction and mental disorders. When asking about the present illness and past history, review patients' medical records to further understand the trajectory of the disease and current treatment. The use of assistive devices can be assessed by both observing and questioning.
3.3 Nutritional status
There are multiple indicators defining a patient's nutritional status. It is now recommended to apply systematic nutritional assessment in clinical practice. Nutritional Risk Screening 2002 (NRS 2002)9 and Mini Nutritional Assessment (MNA) are both commonly used assessment tools. A full MNA is a method that specifically assesses the nutritional status of the elderly and has been widely used abroad. Originally, the MNA is comprised of 18 questions, but for clinical use, the recommended version is the mini nutritional assessment short form (MNA-SF). It has a good correlation with MNA, with good sensitivity and specificity, and the index is easy to measure as a primary screening tool for malnutrition among the elderly. In 2013, the Chinese expert consensus on parenteral nutrition support for the elderly recommended using MNA-SF as the nutritional screening tool,10 and NRS 2002 in inpatient settings. When using MNA-SF, it should be noted that the body mass index (BMI) is preferred, but the calf circumference can be measured instead if the BMI value fails to be obtained. If further assessment is needed, the full MNA should be performed.11
3.4 Cognition and mood status
The assessment for cognitive function, delirium, anxiety, depression, and other related assessments are included. Cognitive disorders in the elderly include mild cognitive impairment (MCI) and dementia. The most widely used cognitive function screening scale domestically and internationally is the Mini-Mental State Examination (MMSE)12 and the “Mini-Cog” test.13, 14 Note that: (i) The test should be performed in a quiet, well-ventilated, comfortable, and bright environment; (ii) It is suggested that only the assessor and the patient is present in the room. If the assessment is performed bedside, avoid interference from others, including family members; (iii) Treat the patient politely and speak in a gentle tone to mitigate any uncooperative emotions; (iv) Perform the tests in strict accordance with the assessment manuals, avoid overinstruction, and provide assistance when allowed. The language spoken by the assessor should be fully understood by the participants; (v) The entire assessment process can be timed without limitation; (vi) Patients with speaking disorders, a lack of emotional cooperation, severe visual or hearing impairment, or who are immobilized are not suitable for this test. To assess elderly patients’ delirium, the American Psychiatric Association recommends the use of the Confusion Assessment Method (CAM),15 which is a simple, effective assessment tool with high sensitivity and specificity for diagnosing delirium. The elderly are often clinically associated with chronic pain, in combination with various chronic medical conditions (such as diabetes, cardiovascular disease, gastrointestinal disease), and presented with various unexplained somatic symptoms or a recent major stressful experience. Depression is a common complication in these patients. Depression scales play a very important role in screening or assessing the severity of depressive symptoms in the elderly. In outpatient and community setting, the Geriatric Depression Scale-4 (GDS-4) is used as a primary depression-screening tool for the elderly.16 Refer the patient to psychiatrist when further treatments or assessments are needed. The Geriatric Depression Scale-15 (GDS-15) is a self-rating screener for depression designed specifically for the elderly17 and can be used in a community setting. The Zung Self-Rating Anxiety Scale (SAS) can be used to evaluate anxiety symptoms in adults.18 Currently, there is no self-rating anxiety scale for the elderly. When performing the tests, both oral and written responses are acceptable. Patients with severe dementia or aphasia are not eligible for this scale.
3.5 Frailty
At present, there is no agreed standard for frailty assessment.19-21 Multiple tools are used in evaluating frailty, such as phenotype of frailty proposed by Fried et al,22 the frailty index proposed by Rockwood et al,23 the FRAIL Scale,24 and Clinical Frailty Scale.25 All assessment tools are not applicable to patients who rely on assistive devices, who cannot walk more than 4 meters, and who have a high risk for fall, with severe heart failure, cachexia, or disability. Currently, it is recommended to use the diagnosis criteria proposed by Fried, but there is no uniform standard for evaluating physical activity in this assessment. The Short Physical Performance Battery (SPPB) and Minnesota Leisure Time Physical Activity Questionnaire can be used to evaluate physical activity.26 The Rockwood Frailty Index was developed based on CGA by counting the number of deficits accumulated. Typically, 30-70 items are counted. Clinically, it is too complex to use. The FRAIL Scale is widely reported as a simple primary screener, and is recommended to be used in an outpatient setting.
3.6 Sarcopenia
The Asian Working Group for Sarcopenia recommends screening sarcopenia by evaluating muscle strength (measured by grip strength) and muscle function (measured by daily walking speed).27 Dual-energy X-ray absorptiometry (DXA) or bioelectrical impedance analysis (BIA) is used to measure muscle mass. Sarcopenia is diagnosed when the appendicular skeletal muscle (ASM) is ≤ 7 kg/m2 in men and ≤ 5.7 kg/m in women with the BIA method or ≤ 7 kg/m2 in men and ≤ 5.4 kg/m2 in women with the DXA method, plus reduced gait speed (<0.8 m/s) or reduced grip strength (male <26 kg, female <18 kg).
3.7 Pain
Pain assessment for older adults requires a detailed history review of the pain and physical examination, determining the following: pain location, intensity, aggravation, mitigating factors, whether it affects mood and sleep, and whether the pain site has paresthesia, hyperalgesia, declined sensory sensation, numbness, and so on. Pain assessment tools for the elderly include Visual Analogue Scale (VAS) and Numerical Rating Scale (NRS). VAS is an effective method to evaluate acute and chronic pain in elderly patients,28 but it requires the patient to have normal vision and motor function. NRS is especially suitable for elderly people who need to assess the level and changes in pain intensity,29 which is also an effective and reliable tool for evaluating acute or chronic pain. However, it is not suitable for elderly patients with poor linear perception or poor understanding of description. When using the NRS, it is best to assess the patient every several hours intermittently. Too frequent assessments may cause anxiety and noncooperation in patients, and loss of self-control and increased anxiety may increase the intensity of pain and affect the results.
3.8 Comorbidity
Comorbidity refers to the presence of two or more chronic diseases in the elderly. It is recommended to use the Cumulative Illness Rating Scale-Geriatric (CIRS-G) for evaluating comorbidity in elderly patients.30
3.9 Multiple medication use
There is currently no consensus on the diagnostic criteria for multiple medication use. Currently, the most widely used clinical standard is to regard “5 or more medications” as multiple medications. It is recommended to use the Beers criteria for inappropriate medication use in elderly people31 and the list of inappropriate medication use in the elderly Chinese32 to assess the potential risk for inappropriate medication use.
3.10 Sleep disorder
Sleep disorder in the elderly patients is mainly evaluated by clinical assessment and scale assessment. In clinical assessment, the form of insomnia, pattern of rest and sleep, sleep-related symptoms and effects on daytime functions, medication history and possible substance dependence, physical examination, and mental status are assessed. Generally for the scale assessment, the Pittsburgh Sleep Quality Index Scale (PSIQ) is recommended,33 and the Ascent Insomnia Scale (AIS) is recommended to use in an outpatient setting.34
3.11 Visual impairment
Snellen's visual acuity table35 is generally used. Requiring the patient to read the headline of a newspaper can also be used as a simple primary screening test. Ask the patient about the history of visual impairment and glasses. Visual assessment in CGA is to screen for visual impairment, and whether the impairment would increase the risk for falls and other geriatric syndromes. Refer the patient to a specialist when further treatment or diagnosis is needed.
3.12 Hearing impairment
Before the examination, please exclude the condition of earwax blockage or otitis media. The hearing test uses a simple method: the assessor stands about 15 cm behind the patient and whispers a few words. If the subject cannot repeat more than half of the words, it may indicate a hearing problem. Ask the patient about the history of hearing impairments and the usage of hearing aids. Refer the patient to a specialist when further treatment or diagnosis is needed.
3.13 Dental health
Check the patient's condition of tooth loss, dentures, and missing teeth. Evaluate the comfort of dentures wearing and assess its impact on eating. Assessment is focused on whether the dental problems affect eating, mood, or nutritional intake. If it is necessary to clarify the status of oral diseases, experts recommend further dental treatment. Refer the patient to a specialist when further treatment or diagnosis is needed.
3.14 Urinary incontinence
It is recommended to use the Incontinence Questionnaire Short Form (ICI-Q-SF) for evaluating the incidence of urinary incontinence and the degree of its influence on the patient.36
3.15 Pressure injury
Pressure injury risk assessments mainly are scale assessment and skin assessment. Domestic and international guidelines for preventing pressure injury recommend the use of the Braden Scale as a primary tool in identifying the risk factors of pressure injury.37 It is the most widely used assessment tool in the world and can be used for elderly patients. Furthermore, assess the skin for localized warmth, swelling, and pain, and test the skin with the blanching test to see whether the skin area turns white when pressed by a finger and returns to red when the finger is removed. Impairment or damage is presented if the skin area stays white.
3.16 Social support
Currently, the most widely used assessment tool for social support in the Chinese population is the Social Support Rating Scale,38 which is suitable for conscious and cognizant elderly patients. The scale has a total of 10 entries in 3 dimensions, including objective support (actual support received by the patient), subjective support (emotional support), and accessibility of support which reflects the individual's active use of social supports, including their way of talking and asking for help, and participation in the activity. Higher scores indicate better social support.
3.17 Living environment
The home environment assessment is only for low-risk elderly patients receiving home care. It lays emphasis on the prevention. At present, self-developed questionnaires are used in domestic studies.39 The home-based environmental assessments in Taiwan can also be used.40 In the home-based or institution-based long-term care circumstances, selected items can be used for living environment assessment.
4 RECOMMENDATIONS ON THE MANAGEMENT OF THE GERIATRIC SYNDROME
For elderly patients who meet the indications for CGA, the expert panel recommends to perform routine and followup CGAs using informatics systems and tools. Assessment tools are chosen accordingly based on different environments, assessors in different fields, different purposes for the assessment, and different settings. For example, the full version CGA software is used in hospital settings to evaluate inpatient elderly people in general and geriatric hospitals. The brief version software is suitable for elderly people in outpatient settings. The self-rating version is suitable for elderly people who receive home-based or institution-based mid- and long-term care.
Based on the results of the CGA, the expert panel recommends following strategies on the management of geriatric syndrome:
- For elderly patients with good physical activity, good nutritional status, normal cognitive functioning, without anxiety or depression, and absence of sarcopenia and frailty, management on the chronic diseases in a traditional way is suggested.
- For elderly patients with high risk for fall, malnutrition, urinary incontinence, frailty, sarcopenia, presented with anxiety or depression, significant function decreases in physical activity and cognition, multidisciplinary team-led management is suggested. The members of the multidisciplinary team should include a geriatrist, nutritionist, mental health physician, nurse, therapist, and physician in related specialists, etc. CGA is used as the basic means to symmetrically evaluate the diseases and functional status of the elderly patients from time to time and facilitate the development of a comprehensive and individualized treatment plan through hospitalization and discharge. The process of the multidisciplinary team-led management is shown in Figure 1.
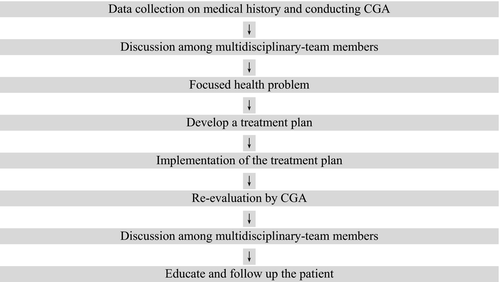 Figure 1Route chart of multidisciplinary team
Figure 1Route chart of multidisciplinary team - When the deterioration of the geriatric syndrome is induced by the onset of a certain acute situation, further specific treatment on the acute disease is preferred.
- When a patient's symptoms worsens and function deteriorates during multidisciplinary team-led management, consider deteriorations in systemic diseases and refer the patients for further treatments on the acute events.
- Use appropriate assessment tools to fit the circumstances. In a brief CGA, some simplified questionnaires are used in consideration of time for data collection. For example, ask patients whether they can walk quickly, dress up themselves, go shopping, bathe, and do housework without difficulty to preliminarily determine their abilities in performing daily activities. Ask patients whether their body weight has declined, and calculate the BMI to preliminarily detect any nutritional problems. Use the FRAIL Scale to assess frailty. Simply ask patients whether there are any problems in passing urine and in bowel movements. Perform measurements on walking pace, grip strength, and calf circumference to preliminarily screen for sarcopenia. Instruct patients to remember 3 words and ask them to repeat these words 1 minute to screen for cognitive problems.
- The expert panel suggests performing CGA on inpatient elderly routinely at admission, during the stay, at discharge, and in follow-ups. In a community setting, preliminarily screen the elderly for geriatric syndrome by CGA routinely. In the mid- and long-term institutional and home-based care, CGA also plays an important part in facilitating integrated management.
CGA is an important technique in geriatric medicine and is just starting to develop in recent years in China. There is limited guidance for clinical practice, and this consensus would promote the implementation and development of standardized CGA.