The case of a 26-year-old male with subacute progressive visual loss
interACTN Case #38: Available: https://interactn.org/2023/11/29/case-38-case-of-a-26-year-old-man-with-subacute-progressive-visual-loss/
Summary of Case
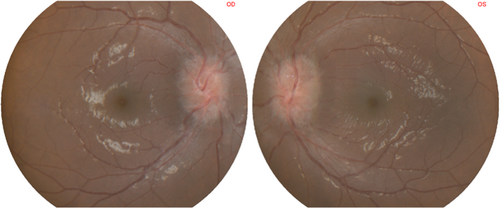
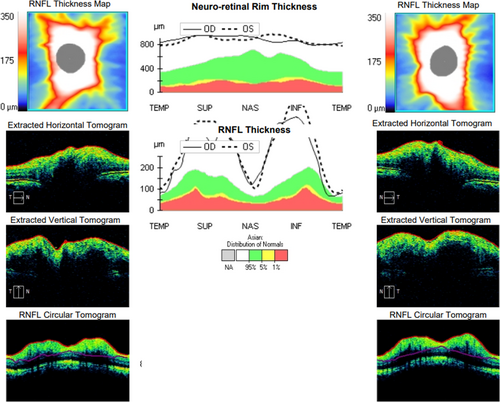
A 26-year-old male with HIV was referred from an infectious disease specialist due to an abnormal finding on fundoscopy. For 3 months, the patient has noticed a maculopapular rash on his palms and soles. He has found penile ulcers and has noticed weight loss of over 10 kg over the past 2 months. A month before his hospital visit, he started to have blurry vision and could not view things as clearly as before. He described the landscape as “foggy.” He denies any loss of color vision, headache, or diplopia. He could still maintain his activities of daily living. Two weeks later, his visual symptoms worsened as he experienced more acuity loss along with desaturation of red colors. No pain on eye movement was evident. On fundoscopic examination, he was found to have bilateral 360-degree optic disc edema with profound elevated and blurring margins of both eyes with no hemorrhage or exudate visualized (Fig. 1). Optical coherence tomography (OCT) shows generalized increase retinal nerve fiber layer thickness and retinal rim thickness of both eyes which was beyond the 95th percentile of the standardized Asian population (Fig. 2). Cerebrospinal fluid analysis shows mild pleocytosis and elevated protein. Serum treponema pallidum hemagglutination assay (TPHA) was positive. Therefore, syphilitic optic neuropathy was suspected. The patient was given aqueous penicillin G 18 mU/day intravenously for 14 days followed by intramuscular injection of benzathine penicillin G 2.4 mU weekly for 3 weeks consecutively.1 After the course was completed, antiretroviral therapy was initiated. After 2 months of treatment, his optic disc edema was much improved without new symptoms.
Diagnosis
Syphilitic optic neuropathy in person with HIV.
Take-Home Points
- Bilateral optic disc edema with profoundly elevated and blurred margins of both eyes could result from increased intracranial pressure, which is called “papilledema,” but also should raise suspicion for other possible causes such as infectious/inflammatory, demyelinating, toxic-metabolic/nutritional, and hypertensive emergency in the appropriate cases.
- Systemic condition and past medical history could help to narrow down the possible etiologies of blurred vision with bilateral optic disc edema.
- Syphilitic optic neuropathy is a rare manifestation of late syphilis. The hallmark of this condition is optic disc edema without association of hemorrhage or exudate in patients who do not have evidence of increased intracranial pressure.2-4
- The proper diagnosis and prompt treatment of syphilitic optic neuropathy leads to better vision outcomes.