Fitting the task to a person with disabilities: A case of return-to-work support for a patient due to left-sided poststroke hemiplegia using tailor-made jigs-and-tools
Abstract
Background
A 45-year-old Japanese male pharmacist developed a stroke in December 2018; hence, he had left-sided hemiplegia due to the after-effects of cerebral stroke. This paper reports the return-to-work (RTW) and after RTW support for poststroke patients from a combined ergonomic and rehabilitation perspective.
Methods
From April 2019 to July 2020, we visited hospitals and workplaces multiple times, making various preparations for workplace accommodation and exchanging information as follows: allowing staggered working hours; securing the flow routes in the back room; equipping a cane holder on his working desk; and adjusting the position of the work tablet. In August 2020, after RTW, we conducted a brief evaluation of residual motor function and an on-site task analysis, and we subsequently made a support tool.
Results
In July 2020, his RTW was eventually realized. Moreover, as a result of introducing the tailor-made support tool, the duration of certain tasks that he had been claiming to be difficult was reduced when compared to that before support-tool use, and the average task duration before and after support-tool use was 32.8 s and 10 s, respectively (reduced by approximately 69.5%).
Conclusion
To augment our efforts, hospital staff, support staff in his workplace, and his employer collaborated to make various workplace accommodations for the smooth realization of RTW before and after RTW. In the present case, the ergonomic and rehabilitation approach after RTW might have contributed to ease of task, work efficiency, and the potential for future job retention.
1 INTRODUCTION
According to the World Health Organization (WHO), with the aging of the global population, the occurrence of cardiovascular disease (heart disease and stroke) has become an important health problem.1 In particular, if a working-age person suffers a stroke, the poststroke effects may reduce work performance.2 Recently in Japan, Saeki et al reported that the proportion of stroke survivors who have had a successful return-to-work (RTW) experience has remained static at 45% for the past 20 years.3 According to previous studies, important factors associated with RTW and stroke are gender, age, enterprise size, education level, stroke severity, and comorbidity.2, 4, 5 In addition, the potentiality of RTW after hospital discharge was reported to be influenced by impairments and occupation.6 In particular, poststroke survivors have residual impairments in the upper and lower limbs (hemiparesis), which are important factors related to RTW.6, 7 Consequently, hemiparesis affects work ability and productivity after RTW; hence, it is important to make an effort in workplace accommodation—fitting the task to the person with disabilities—within each workplace.8
The WHO recommends assessing the capacity to work of persons with disabilities and thereby setting up disability management programs to support RTW.1 Published in February 2016, the Japanese Guideline for Assisting Treatment-Work Balance clearly states that the occupational health support centers nationwide owned by the Japan Organization of Occupational Health and Safety (JOHAS) will RTW support and advise for companies and workers.8 Therefore, in order to provide RTW support from various aspects, occupational health support centers nationwide have not only occupational health physicians, public health nurses, and ergonomists but also other specialists (eg, nurse, lawyer, labor and social security attorney, medical social worker, and physical therapist) were assigned in recent years. Moreover, the Japanese guidelines also recommend creating an RTW support plan that includes workplace accommodation for persons with disabilities.8 Additionally, it was indicated that in specific cases of persons with disabilities, environmental factors hindered optimal performance; thus, it is important to increase RTW rates through workplace accommodation.1 According to previous studies, the importance of workplace accommodation for persons with disabilities through the use of ergonomic principles is emphasized.9, 10 Moreover, previous studies have shown that evaluation from an ergonomic and rehabilitation perspective is important for workplace design for persons with disabilities.11 Therefore, in order to increase the RTW rate, it seems necessary to accumulate useful case reports on workplace accommodation from ergonomic and rehabilitation perspectives.
In this paper, we report on RTW support for a poststroke patient. The Fukuoka Occupational Health Support Center (FOHSC), which is one of centers owned by the JOHAS, provides RTW support and advise free of charge to companies and workers who have requested. The role and aim of FOHSC in the present case study was to gather opinions from patients, hospital staff, employers, and support staff in the workplace regarding the adjustments necessary for establishing optimal working environments for patients and workplace staff. Hence, we visited hospitals and workplaces, making various preparations and exchanging information. In particular, we considered it important to publish detailed information from an ergonomic and rehabilitation perspective in this case study.
2 CASE PRESENTATION
The present case was one of 423 consultations received by FOHSC in 2019. A 45-year-old Japanese male worker, who was employed as a pharmacist at a pharmacy, developed a stroke in December 2018. Subsequently, he was diagnosed with left-sided spastic hemiplegia. Although he lived alone, he returned to his hometown and was transferred to a hospital near his parents' house in January 2019. He was eager to return to work, and thus, his manager in the pharmacy requested RTW support from FOHSC in April 2019. Hence, we began collaborating with hospital staff (eg, physicians, nurses, physical therapists, occupational therapists, and medical social workers) and support staff in his workplace to support his RTW. Furthermore, we occasionally visited the pharmacy because it was important to understand the interaction between the patient's functions and the workplace's environment and work system so as to fit the task and environment to his condition. When it comes to occupational medicine in Japan, any company with over 50 employees is required to hire an occupational physician under the Japanese Industrial Safety and Health Law. The pharmacy was small-sized enterprise with a few employees, so it did not have a contract with any occupational health physician or public health nurse.
On March 6, 2020, we visited the workplace for the first time to conduct a preliminary workplace evaluation at the time he was making RTW plans. We assessed the working desk he planned to use for the task and the routes he was likely to take within the back room. We recommended the employer to implement the following to protect him from trips and falls and avoid reducing productivity: allow staggered working hours, ensure secure flow routes in the back room (eg, relocate the trash), equip his working desk with a cane holder, and place the work tablet on the right side of his working desk. Workplace preparation was conducted concurrently with the patient's discharge preparation. On July 8, 2020, his RTW was realized.
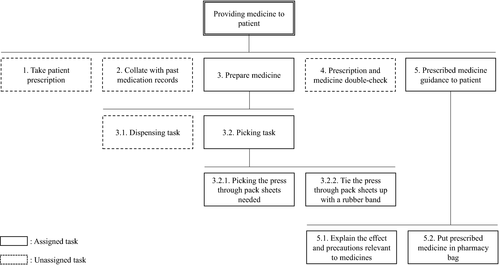
Evaluation of motor function, including anthropometry, is important to work environment design for persons with disabilities.1, 9, 12 Therefore, on August 25, 2020, we made a second visit to his workplace for a brief evaluation of residual motor function, on-site task analysis using the work sampling and time-and-motion methods,10, 12 and interviews. The results of the brief evaluation of motor function involved the following variables: (a) active range of motion (AROM) of upper limbs, (b) Brunnstrom Stage13 of upper limbs, (c) grip strength measurement, and (d) check-up gait patterns. The AROM of his left upper limb was 140° of shoulder joint flexion and almost normal for left elbow joint flexion and extension, left forearm supination and pronation, and left wrist joint flexion and extension. Brunnstrom Stage is a motor function test that evaluates the recovery stage of hemiplegia.13 It is categorized according to Stage I-VI. There is no voluntary movement in Stage I. In Stage VI, various coordinated movement is possible. His left hand was capable of both cylindrical and spherical grasps. Furthermore, all his left fingers could be actively extended. These finger movements are the criteria for Brunnstrom Stage V. Therefore, his left hand seemed to correspond to Brunnstrom Stage V. However, when he moved his right hand and/or finger, a certain associated movement of his left hand and fingers occurred. Furthermore, we checked the grasping power of his hands, which had powers of 29.5 kg and 8.5 kg for the right and left hands, respectively. Although his gait pattern was affected by the leg circumduction due to extensor hypertonia in the lower limb, his gait performance was self-sufficient with a short leg brace and T-cane. The results of the hierarchical task analysis are shown in Figure 1. The main tasks assigned to him were “prepare medicine” and “prescribed medicine guidance to patient.” Although he had to work with both hands in the “Put prescribed medicine in pharmacy bag” task, he was able to press down the pharmacy bag with his left hand and put the medicine in the pharmacy bag with his right hand. However, he complained in an interview that “tie the press through pack sheets (PTPs) up with a rubber band” work was difficult. Thus, we performed a micromotion analysis to identify the problem associated with “tie the PTPs up with a rubber band” (Table 1). The “tie the PTPs up with a rubber band” task consisted of six elements and required a fair amount of seconds for the following motions: “hold the PTPs, tie the PTPs up with a rubber band” and “tie the PTPs up with a rubber band” for the right and left hands, respectively. In this micromotion, his left hand was not holding a rubber band. Due to the impairments in dexterity of the left hand after stroke, he could barely hook a rubber band on his finger. However, we applied his left hand to “Grasp” for convenience in this micromotion. Furthermore, in this micromotion, he made two and three mistakes on the third and fourth time, respectively. In addition, he broke PTPs in the fourth task. As the number of tasks increased, the dexterity of the left hand gradually decreased. Moreover, commercially available fingers and/or hand splints did not seem to match his task. Based on the results of this analysis, we proposed to him and his employer that we make tailor-made jigs-and-tools to support his task. Additionally, from the perspective of rehabilitation, it was recommended to actively use the left hand for other assigned tasks that do not require dexterity.
| No | Left hand description | Therblig | Measured time (sec) | Therblig | Right hand | ||||
|---|---|---|---|---|---|---|---|---|---|
| First | Second | Third | Fourth | Fifth | |||||
| 1 | — | — | 1 | 1 | 1 | 1 | 1 | G | Grasp a rubber band |
| 2 | — | — | 1 | 1 | 1 | 1 | 1 | TE | Reach for PTPs |
| 3 | — | — | 2 | 2 | 1 | 2 | 3 | G | Grasp PTPs |
| 4 | Grasp a rubber band | G | 1 | 1 | 2 | 1 | 1 | H | Hold the PTPs |
| 5 | Tie the PTPs up with a rubber band | U | 8 | 6 | 45 | 59 | 15 | H, U | Hold the PTPs, Tie the PTPs up with a rubber band |
| 6 | — | — | 1 | 1 | 1 | 1 | 1 | TL, RL | Put in the designated box |
- Abbreviations: G, grasp; H, hold; No, number; PTPs, press through pack sheets; RL, release Load; sec, seconds; TE, transport empty; TL, transport loaded; U, use.
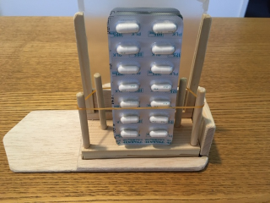
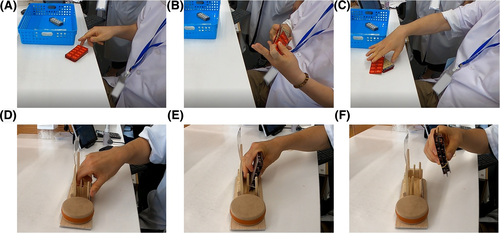
On our third visit to the workplace on September 4, 2020, we gave him jigs-and-tools (Figure 2). This support tool is a device for wrapping a rubber band around four pillars. The PTPs in the expanded rubber band were set, and the rubber band and PTPs were subsequently removed together. With this support tool and operation, it was envisioned that he could perform the traditional task of “tie the PTPs up with a rubber band” with the right hand only (Figure 3). It was made based on the size of his right hand, size of the PTPs to be handled, and operability with only the right hand in mind. Although we made support tools, the cost was very low. Furthermore, we performed micromotion analysis again to compare the differences between before and after support tool use. As shown in Table 2, after using the support tool, the micromotion consisted of six elements. Therefore, there was the same number of motion elements than before support tool use. However, the average number of seconds for five-time measurements showed a decreasing trend compared to that before support tool use, and the number of seconds before and after support tool use was 32.8 s and 10 s, respectively (reduced by approximately 69.5%). According to the patient himself, the usability of the support tools was beneficial.
| No | Left hand description | Therblig | Measured time (sec) | Therblig | Right hand | ||||
|---|---|---|---|---|---|---|---|---|---|
| First | Second | Third | Fourth | Fifth | |||||
| 1 | — | — | 1 | 1 | 1 | 1 | 1 | G | Grasp a rubber band |
| 2 | — | — | 4 | 4 | 5 | 6 | 4 | U | Wrap a rubber band around a tool |
| 3 | — | — | 1 | 1 | 1 | 1 | 1 | TE | Reach for PTPs |
| 4 | — | — | 2 | 1 | 1 | 1 | 1 | G, TL | Grasp PTPs and put them on the tool |
| 5 | — | — | 2 | 1 | 1 | 1 | 1 | G | Grasp the PTPs and rubber band |
| 6 | — | — | 1 | 1 | 1 | 1 | 1 | TL, RL | Put in the designated box |
- Abbreviations: G, grasp; No, number; PTPs, press through pack sheets; RL, release load; sec, seconds; TE, transport empty; TL, transport loaded; U, use.
3 DISCUSSION AND CONCLUSION
In the present case, a male pharmacist had left-sided hemiplegia due to poststroke sequelae, and shortly after RTW, he complained of difficulty in certain tasks. It was difficult to work on “wrap a rubber band twice over multiple PTPs” because his left hand could not grasp the PTPs due to the associated movement. Additionally, a commercially available brace did not seem to match his task. Therefore, we developed a support tool to fill the gap between him and the difficult task. As a result, the number of seconds required for the task was reduced.
According to a previous study, more supportive social and work environments and professional jobs had a higher probability of RTW.7 Similarly, this case of RTW was realized in a situation where good conditions (eg, occupation, job requirements, personal work motivation, and the employer's effort) were met without a glitch, in line with the Japanese guidelines.8 For example, he was allowed staggered working hours. Moreover, he was able to walk alone using a T-cane and short leg brace; however, it was difficult to maintain a standing position for a long time. For that reason, the work assigned to him involved tasks that could be done while sitting. Furthermore, support staff in the workplace secured the flow routes in the back room to prevent trips and falls. A T-cane holder was attached to his work desk, and the tools on his desk were arranged such that they would be easy to use, despite motor impairment of the left upper limb. However, he complained of difficulty in certain tasks shortly after RTW. As a result of the evaluation of residual motor function and the on-site task analysis, there was clearly a mismatch between the motor function required for the task with his residual motor function. As a result of micromotion analysis, we identify the problem associated with “tie the PTPs up with a rubber band.” Because the dexterity of left hand after a stroke was impaired, he could barely hook a rubber band on his finger. Therefore, we considered the process to carry out the work of “tie the PTPs up with a rubber band” with only one hand. Normally, we recognize that the task of “tie the PTPs up with a rubber band” is the work of tying up “PTPs” with “rubber bands.” However, we considered how to put “PTPs” in “rubber bands.” Additionally, we made a support tool consisting of struts to fix the rubber bands. The support tool eliminated the mismatch between him and his task.
It has been reported that if workplace environments include tasks that do not accommodate persons with disabilities, it may make a person less productive and eligible for a lower market wage.1 It has also been suggested that a mismatch between a task and its implementer becomes psychologically stressful.12 In addition, a person with disabilities may leave their job as a result of mental health and psychosocial problems and be offered a lower wage.1, 8 In order to prevent the above, it is important to fit the task to a person with disabilities; hence, evaluation of residual motor function and task analysis are essential. It is likely that this will contribute to the retention of jobs for persons with disabilities through continued workplace accommodation, even after RTW. For this reason, workplace accommodation using the ergonomic and rehabilitation approach14 is important not only in contributing to RTW after disease but also in improving after RTW job retention for people with disabilities. Furthermore, in the present case, the patient was grateful to all staff who supported his RTW. In addition, he began to voluntarily improve his diet to prevent stroke recurrence. The sincere support of those around him might have prompted behavior change.
In conclusion, it seems that the use of support tools reduces task mistakes and task duration. Hence, it might have had a positive effect on physical and mental health. Consequently, in the present case, the ergonomic and rehabilitation approach might have contributed to the potential for future job retention. Additionally, task analysis is essential to fit the task to people with disabilities. Micromotion analysis may be useful, especially if the worker has motor impairment due to sequelae caused by diseases. This is because motor impairment affects micromotion and also affects tasks that consist of micromotion components. Furthermore, in order to retain a person with disabilities, it is considered necessary to select the preferred method for “fitting the task to a person with disabilities” after motor impairment and work environment evaluation (eg, compensate with compensatory movement, increase the number of motions, use a brace and/or make tailor-made jigs-and-tools, etc). In other words, ergonomics and rehabilitation are essential perspectives for workplace accommodation for persons with disabilities after RTW.9, 14
4 APPROVAL OF THE RESEARCH PROTOCOL
The ethical committee of the Association for Preventive Medicine of Japan (Approval Number: 2020006) approved this study.
5 INFORMED CONSENT
Written informed consent was obtained from the patient and employer for publication of this case report.
6 REGISTRY AND REGISTRATION NO. OF THE STUDY/TRAIL
N/A.
7 ANIMAL STUDIES
N/A.
ACKNOWLEDGMENT
We are grateful to the patient, fellow employees of the company he works for, and his employer for their participation. We would also like to thank Editage for English language editing.
CONFLICTS OF INTEREST
Authors declare no conflicts of interest for this article.
AUTHORS’ CONTRIBUTIONS
NT, FI, RM, and SO contributed to study design. NT and FI collected the data. NT and JA analyzed the data and drafted the manuscript. All the authors contributed to the writing of the manuscript, critical revision, and agreed with the final version.




