New form of idiopathic osteolysis: Nodulosis, arthropathy and osteolysis (NAO) syndrome
Abstract
We describe 10 patients (6 females and 4 males) from 6 unrelated families with an autosomal recessive disease characterized by simultaneous presentation of nodulosis, arthropathy and osteolysis. They were followed up regularly at King Faisal Specialist Hospital and Research Center in Saudi Arabia for clinical evaluation, serial blood work-up, and evaluating radiological changes. Nodulosis and arthropathy were the clinical criteria for inclusion in this study, and the ten patients fulfilled these criteria. All patients had nodulosis and distal arthropathy. Eight patients (80%) presented with deformed hands and four (40%) with painful hands. All patients had parents who were first cousins and three families had more than one affected child, the finding suggesting autosomal recessive inheritance. Osteopenia and undertubulation of bones distally more than proximally, and upper limbs affected more often than lower limbs, were found in all patients. Osteolysis was seen in carpal and tarsal bones. Other common findings were sclerotic cranial sutures, brachycephaly, and broad medial clavicles. This novel phenotype should be considered in the differential diagnosis of chronic arthritis. Familial arthropathies are more often seen in communities where interfamilial marriage is common. Such a collection of patients is ideal for homozygosity mapping of the disease locus. Am. J. Med. Genet. 93:5–10, 2000. © 2000 Wiley-Liss, Inc.
INTRODUCTION
Idiopathic osteolysis is a rare skeletal disorder usually presenting in early childhood with progressive destruction mainly of the carpal and tarsal bones. Other bones may also be involved [Pai and Macpherson, 1988]. The first case of “disappearing-bone disease” was described by Jackson in 1838, since then several forms of osteolysis have been described under a variety of designations [Gorham and Stout, 1955; Gluck and Miller, 1972; Kohler et al., 1973; Macpherson et al., 1973; Petit and Fryns, 1986]. Torg et al. [1969] described three siblings from Columbia with simultaneous presentation of osteolysis, osteopenia, arthropathy and subcutaneous nodules. Subsequently, similar cases have been reported as Torg's osteolysis or Winchester syndrome [Winchester et al., 1969; Sozke et al., 1995; Eisenstein et al., 1998]. Because there are various forms of idiopathic osteolysis, the current classification proposed by the International Bone Dysplasia Society [Eisenstein et al., 1998] could be considered a useful classification tool (Table I). We describe the largest known collection of patients with multicentric osteolysis predominantly involving carpal, tarsal and interphalangeal bones where nodulosis is the main presenting finding in addition to arthropathy. This phenotype should be differentiated from other types of osteolysis and must not be confused with juvenile rheumatoid arthritis.
| Multicentric predominantly carpal and tarsal in the hand |
| Multicentric carpal-tarsal osteolysis with and without arthropathy |
| Multicentric predominantly carpal tarsal and interphalangeal |
| François syndrome |
| Winchester syndrome |
| Torg syndrome |
| White-Hemingway carpal tarsal phalangeal syndrome |
| Predominantly distal phalangeal |
| Hajdu-Cheney syndrome |
| Giacci familial neurogenic acroosteolysis |
| Mandibulo-acral syndrome |
| Predominantly involving diaphyses and metaphyses |
| Familial expansile osteolysis |
| Juvenile hyaline fibromatosis |
MATERIALS AND METHODS
Ten children with nodulosis, arthropathy and osteolysis from six unrelated families were followed prospectively at King Faisal Specialist Hospital and Research Centre (KFSH-RC), Riyadh, Saudi Arabia between 1992 to 1998. Clinical information was recorded for each patient, including age, onset of nodulosis and musculoskeletal manifestations. All patients had follow-up visits every 3–6 months. At each visit, interval history, physical examination included detailed musculoskeletal assessment, functional ability and assessment of the nodules (distribution, change in size and consistency). Ophthalmologic evaluation was done in all patients. Routine laboratory investigations performed included: complete blood count (CBC), renal and hepatic profile (RP and HP), erythrocyte sedimentation rate (ESR), rheumatoid factor (RF) and antinuclear antibody (ANA). Skeletal survey was done for all patients and magnetic resonance imaging (MRI) and biopsy of the nodules were performed for two and four patients, respectively (Table II). Metabolic screening (tandem mass spectrometry, gas chromatography and ceramidase level) was performed for 3 patients of Family 1 to rule out the possibility of metabolic disorders such as storage disease.
| Family no. | Patient no. | Age (years) | Gender | Age at onset (years) | Presenting symptom | MRI (foot) | Biopsy (nodule) | Others |
|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 12 | M | 5 | Fracture of right arm and femur, nodules in soles, claw hands | |||
| 2 | 19 | F | 6 | Bilateral claw hand and foot deformity, nodules in soles | ||||
| 3 | 10 | M | 6 | Painful hands especially after mild trauma, claw hands, nodules in the soles | Fibrous tissue | |||
| 2 | 4 | 9 | F | 1 6/12 | Deformity of hands, nodules in soles | Fibrous tissue | Congenital heart disease, mental retardation, MTX, D-penicillamine | |
| 5 | 10 | F | 1 6/12 | Painful hands, nodules in soles | Fibrous tissue | Meningitis at 2 months, mental retardation, CT scan of brain: arachnoid cyst, MTX, D-penicillamine | ||
| 3 | 6 | 11 | F | 1 | Painful hand, nodules in hands and soles | Fibrous tissue | ||
| 7 | 5 | F | 8 1/2 | Nodules in soles, left clinodactyly | ||||
| 4 | 8 | 3 | M | 2 1/2 | Nodules in hands and soles | |||
| 5 | 9 | 7 | M | 1 | Deformed hands, nodulosis elbow, knee, shin, and soles | Fibrous tissue | MTX, D-penicillamine | |
| 6 | 10 | 12 | F | 9 1/2 | Painful nodules on soles, right clinodactyly | Fibrous tissue | Mental retardation |
- * MT, methotrexate; CT, computed tomography.
Three patients (Patients 4, 5, and 9) were commenced on oral methotrexate (mean dose 15 mg/m2/week) and D-penicillamine (15 mg/kg/day). This combination was started as a trial to control fibrous deposition leading to nodule formation and to minimize the progression of joint contracture.
RESULTS
All patients (100%) had nodulosis, 8 patients (80%) presented with deformed hands and 4 patients (40%) presented with painful hands. Mean age at onset of symptoms was 3.4 years (range, 1 to 9 1/2). The clinical manifestations of the patients are summarized in Table II. Parents of all patients were first degree relatives and reported no similar history in previous generations. Three families had more than one affected child. Eight patients had minor facial anomalies with frontal bossing and hypertelorism and 5 patients had brachycephaly (Fig. 1). Patient 1 was confined to a wheelchair at the first clinical visit secondary to frequent falls with multiple pathological fractures. All patients had nodules on plantar aspects of their feet; 2 patients (Patients 6 and 8) also had nodulosis on the second metacarpophalangeal joint (MCP), whereas Patient 9 had nodulosis over the elbows and knees. Each nodule measured approximately 0.5 × 0.5 cm. These nodules were mobile, non-tender and hard in consistence with smooth surface. The arthropathy started in hands and feet and subsequently progressed to involve more proximal joints. Eight patients had a decreased range of motion (ROM) of the interphalangeal joints (IP) and MCP with widening of the phalanges and metacarpal bones. Six patients had decreased ROM of the wrists. Five patients had similar restriction of the elbow joints. Three patients had knee joint involvement and one had limited ROM of the shoulder joints. None of the involved joints showed evidence of acute arthritis. At the most recent follow up, none of the patients had hip joint involvement. All patients had normal CBC, RP, HP and ESR, and negative RF and ANA. Metabolic screening was normal in the three patients from Family 1, however, only Patient 3 had minor anomalies. All the 10 patients (100%) had generalized osteopenia, and advanced osteolytic changes were present in 70% of patients (Fig. 2). Seven (77%) of 9 patients had sclerotic cranial sutures, 5 (62%) of 8 patients had brachycephaly, and broad medial clavicles were seen in 6 (66%) of 9 patients (Table III).
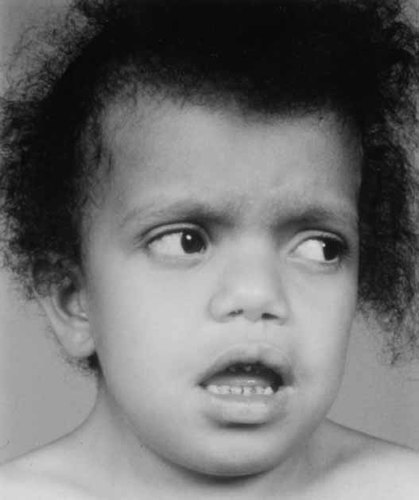
Four-year-old girl with NAO-syndrome. Photography of face demonstrates frontal bossing, hypertelorism and coarse facial features.

Radiograph of left hand of a girl with NAO syndrome at age 3 7/12 years (a) and at age 4 4/12 years (b), showing progress of arthropathy of wrists and hands.
| Osteopenia | 10/10 |
| Brachycephaly | 5/8 |
| Sclerotic calcarium sutures | 7/9 |
| Squared vertebrae | 5/9 |
| Broad medial clavicles | 6/9 |
| Undertubulation | 8/9 |
| Arthritis | 8/10 |
| Osteolysis | 7/10 |
| Contraction | 7/10 |
| Nodule | 2/3 |
| Progress of disease | 7/7 |
MRI of the nodules showed dense fibrous tissue (Fig. 3). Biopsy from the nodules showed fibrosis extending through the whole thickness of the reticular dermis into the subcutaneous tissue (Fig. 4). All treated patients showed encouraging results at their 3–6 month follow-up clinic visits. One patient was able to walk for the first time 6 months after initiating therapy. Both patients showed no further deterioration in both joint contracture or nodule formation. The combination therapy, however, did not stop the osteolysis. One patient had evidence of gastric irritation while he was on folic acid prophylaxis. Subsequently, the methotrexate dose was reduced to 10 mg/m2/week with good response. No patients showed elevated liver enzymes and D-penicillamine was well tolerated.

MRI of right foot of a nine-year-old girl with NAO syndrome. Sagittal proton density weighted imaged demonstrates a centimeter sized nodule in the plantar soft tissue of the foot (arrow).

Histology of subcutaneous nodule from a patient with NAO Syndrome, showing poorly demarcated fibrotic area composed of thick, dense collagen fibers with plump fibroblasts in between. No degenerative features (PAS staining).
DISCUSSION
We report on 10 children from 6 unrelated families whose clinical manifestations included nodulosis, arthropathy and osteolysis. Parental consanguinity, the absence of the disease in earlier generations, multiple affected sibs and the early onset of manifestations support the hereditary nature of this disease and suggest an autosomal recessive mode of inheritance.
Torg et al. [1969] described a possible autosomal recessive idiopathic multicentric osteolysis in 3 siblings. This was based on the absence of the disorder in earlier generations, consanguinity of parents and involvement in 3 of 6 siblings. Subcutaneous nodules were described but not regarded a major presenting feature of the disease. Two other reports suggested that Torg syndrome might occur in different ethnic groups and could be associated with other organ involvement [Winchester et al., 1969; Sozke et al., 1995]. Eisenstein et al. [1998] recently reported an additional case of Torg syndrome where the nodules, contrary to our findings, were not major presenting manifestations, but rather occurred years later. Cases with multicentric osteolysis may have been reported as cases of Winchester syndrome or Winchester-like syndrome [Winchester et al., 1969; Hollister et al., 1974; Cohen et al., 1975; Dunger et al., 1987]. The overlap between different osteolysis syndromes may be due to the similarities between clinical characteristics and the disease stage at the time of diagnosis. Our patients share many findings with those reported by other authors but are unique in that nodulosis is a primary finding followed by arthropathy and osteolysis [Torg et al., 1969; Winchester et al., 1969; Hollister et al., 1974; Sozke et al., 1995].
Winchester et al. [1969] described a type of osteolysis with peripheral corneal opacities, severe joint contracture and “coarse” facial appearance in two daughters of first cousin parents. This osteolysis syndrome is different from that in our series of patients, because none of our patients had ophthalmologic abnormalities. Another difference between the present series and other forms of osteolysis is minor facial anomalies. Frontal bossing and hypertelorism were observed in 8 of our patients and brachycephaly observed in 5 patients. None of our patients had a “gargoyle-like face” that was described in Winchester syndrome. Corneal opacity, gingival hypertrophy and a large tongue were not found in the present series. Idiopathic osteolysis was described in association with nephropathy and hypertension [Macpherson et al., 1973]. All our patients, however, had normal blood pressure with normal renal function. Gorham and Stout [1955] reported 24 patients with monocentric and massive osteolysis, and vascular abnormality in the form of hemangiomatosis. This was not found in our cohort. One (Patient 4) of our patients had a double outlet right ventricle. This is most likely a coincidental finding because an affected sibling (Patient 5) had no cardiac involvement. Petit and Fryns [1986] reported an autosomal recessive distal osteolysis with mental retardation and characteristic facial appearance, such as maxillary hypoplasia, exophthalmos, and broad nasal tip. None of their patients had nodulosis, however, and osteolysis was visible on X-ray examination only after age 7 years. The manifestations of the present disease considerably overlap with those of other forms of idiopathic multicentric osteolysis. The similarities and differences among these disorders are summarized in Table IV.
| Torg syndrome | Winchester syndrome | Juvenile hyaline fibromatosis | Farbr lipo-granulomatosis | NAO syndrome | |
|---|---|---|---|---|---|
| Clinical | |||||
| coarse face | unremarkable | + | − | − | + |
| corneal opacity | + | − | + | − | |
| subcutaneous nodule | moderate | − | multiple tumor-like lesions | moderate | prominent |
| arthropathy | prominent small/large joint | moderate | contracture small/large joint | mild–moderate | prominent small joint |
| gum hypertrophy | + | prominent | − | − | |
| age of onset | school age | infancy | infancy | early infancy | preschool age |
| main feature | deformities of phalanx/hand | coarse feature | generalized stiffness of all joints | nodule, hoarseness, respiratory insufficiency | nodulosis |
| Radiologic | |||||
| carpal/tarsal involvement | + | + | + | + | + |
| osteopenia | mild | severe | severe | mild | severe |
| osteolysis | moderate | severe | mild/moderate | mild | severe |
| broad medial clavicles | prominent | ||||
| squared vertebra | prominent |
- * +, present; −, absent.
Patient 5 was treated for neonatal meningitis, that was complicated by severe brain damage and mental retardation. Three patients (Patients 4, 5, and 10) were mentally subnormal. This association has to be studied further because there are insufficient data to suggest that mental retardation is associated with this clinical presentation. This possibility can not however be ruled out because two patients (Patients 4 and 10) had no known cause for subnormal mentality. All other patients in our series had normal intelligence and showed a good school performance.
Radiological findings were helpful in reaching the diagnosis in our series. Laboratory studies were not helpful in making the diagnosis. The inflammatory markers were not high and this might reflect the late referral of these cases, because patients with osteolysis could have high acute phase reactants and high cytokines at earlier stages of the disease [Eisenstein et al., 1998]. This might partly explain the response to methotrexate and D-penicillamine. The exact cause of osteolysis is not known, but Cohen et al. [1975] suggested abnormal fibroblast function. This mechanism may play a role in the nodular regression and improved joint ROM, and should be studied.
In summary, overlap between different types of osteolysis is well recognized. We here describe a large cohort of patients with “nodulosis, arthropathy and osteolysis” that share findings with the osteolysis described by Torg et al. [1969]. Our group of patients, however, presented initially with nodulosis and have unique radiological findings that probably represent a new form of idiopathic osteolysis. We would like to call this unique association of Nodulosis, Arthropathy and Osteolysis, NAO syndrome. These clinical signs should be recognized and not to be confused with other chronic arthritis, particularly in populations where consanguinity is common. Genetic localization of this novel disorder and other forms of osteolysis by linkage analysis may reveal the basis of heterogeneity observed in these disorders.




