Hodgkin′s Disease with Atypical Clinical Presentation, Associated with Ataxia-Telangiectasia
Abstract
The authors report a 4-year-old male with Hodgkin′s disease with atypical clinical presentation, laboratory data and imaging studies as well as an increased radiosensitivity. These were the first symptoms which raised the suspicion of ataxia-telangiectasia. The lymphoma presented as a solid tumor mass in the right upper posterior mediastinum without peripheral lymphadenopathy. The alpha-fetoprotein was significantly increased and the diagnosis of a germ-cell tumor or neuroblastoma was suspected. After partial resection of the tumor the histology indicated Hodgkin′s disease - mixed cellularity. The boy received chemotherapy according to DAL HD-95 protocol without any unusual toxicity. Low-dose radiation therapy of the upper and middle mediastinum was followed by early radiation-induced esophagitis and appearance of a large pericardial effusion one year later. Ataxia and bulbar and skin telangiectasias at the radiation site appeared in the next years. He suffered recurrent pulmonary infections and succumbed to severe pneumonia with respiratory failure and pulmonary hypertension five years after the diagnosis of malignant lymphoma without evidence of recurrence of Hodgkin′s disease.
1. Case Report
The child was a 4-year-old male of Roma origin, born after second normal pregnancy without family history of immune deficiency. He had a past history of cerebral palsy, diagnosed at the age of 20 months because of a delay in motor and intellectual development. His present complaints were productive cough and fever for one month. After admission to the regional hospital physical and X-ray signs of right pulmonary infiltrate were found, and he received antibiotic treatment with Clindamycin, Amikacin, Imipenem, and Cefepime without any improvement. He was referred for further diagnostic evaluation to the Department of Pediatrics, Medical University-Plovdiv. Physical examination on admission showed mask-like, sad, and relaxed face with progeroid features, growth retardation, reduced subcutaneous fat, generalized muscle hypotonia and atrophy, bronchial breathing in the right parascapular region, tracheal stridor, and enlarged liver 3 cm below the costal margin and lack of peripheral lymphadenopathy. Mental retardation was mild (IQ: 60%) with predominantly affected expressive speech and fine motor skills. Computer tomography (CT) scan showed tumor mass in the right upper posterior mediastinum (Figure 1). It deviated the trachea and was well demarked from the pulmonary parenchyma. No destruction of the adjacent bones was evident.

Laboratory data showed leukocytosis, thrombocytosis; elevated erythrocyte sedimentation rate, serum fibrinogen and C-reactive protein 221 mg/L. The diagnostic workup for the mediastinal tumor revealed significant increase of alpha-fetoprotein (AFP) 238.98 ng/mL (reference range 0–5 ng/mL), moderate elevation of vanylmandelic acid 80.9 μmol/l, anergic tuberculin test, and negative blood and sputum cultures and serology for ecchinococcus.
Germ-cell tumor or neuroblastoma was suspected and the boy was referred to the Pediatric Surgery Department for thoracotomy and biopsy. The tumor was partially resected. The histological examination revealed HD—mixed cellularity subtype. The biopsy specimen was reviewed by two independent pathologists, who confirmed the diagnosis. The abdominal ultrasound and CT examination did not reveal enlarged lymph nodes or focal changes in the liver and spleen. The clinical stage was considered IIB, and the boy underwent chemotherapy according to DAL HD-95 protocol: 2 OEPA (Oncovin, Etoposide, Prednisolone, and Adriamycin) and 2 COPP (Cyclophosphamide, Oncovin, Prednisolone, and Procarbazine) blocks. The chemotherapy was well tolerated without unusual toxicity. Irradiation of the upper and middle mediastinum followed, but it was stopped at a total dose of 13.5 Gy because of intermittent retrosternal pain and hematemesis. Radiation-induced esophagitis was diagnosed. It was treated successfully with parenteral nutrition and protectors of the mucosa for 10 days. At that time HD was in complete remission, indicated by the imaging studies and laboratory tests for biological activity.
One year later a large pericardial effusion with clinical signs of cardiac failure was detected (Figure 2).
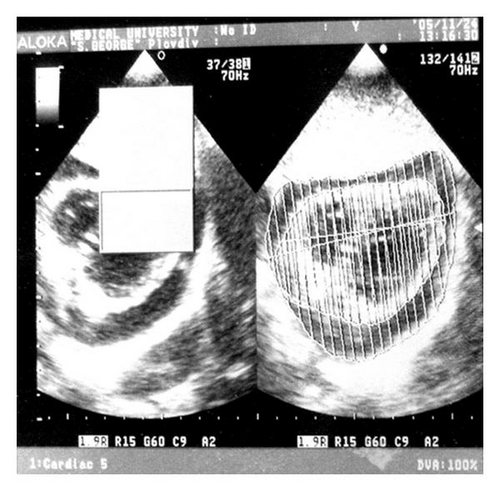
The diagnostic echocardiography-guided pericardiocentesis yielded 120 mL of yellowish clear fluid with exudative characteristic: total protein level of 53 g/l, lactic acid dehydrogenase: 411 UI/l, and WBC: 400 × 106/l with a predominance of lymphocytes from the cytologic study. The cultures of the pericardial fluid excluded nonspecific and mycobacterial infection. Until obtaining the final results of the culture for mycobacteria, the child received empiric tuberculostatic therapy for one month, during which there was a slight increase in the amount of the pericardial effusion. After several therapeutic pericardial punctures he was finally referred for pericardiotomy. Despite the late onset we concluded that the pericarditis was most probably radiation induced. The patient received long-term systemic steroid treatment at a dose of 2 mg per kg body weight, which resulted in gradual resolution of the pericardial effusion.
At the age of six static and locomotor ataxia was noted. The neurological examination showed cerebellar gait ataxia, positive Romberg sign, dysmetria, and intention tremor, oculomotor apraxia, and normal muscle strength but diminished deep tendon reflexes of the lower extremities. Telangiectasias in the temporal and nasal parts of the bulbar conjunctiva and skin telangiectasias at the radiation site appeared at the same age. A-T was suggested. The CT scan and magnetic resonance imaging (MRI) of the brain and spinal cord were normal. The laboratory data revealed low levels of immunoglobulin (Ig) A and G, normal level of Ig M, and high and progressively increasing AFP 1240 ng/mL.
In the following three years the boy suffered monthly recurrent pneumonias and had permanently increased bronchial reactivity. He experienced two episodes of hemoptysis, requiring tracheobronchoscopy, which showed severe inflammation and purulent secretions. The lung CT scan was consistent with chronic fibrotic pulmonary changes without evidence of HD recurrence. The patient received several courses of systemic steroid treatment, maintenance with inhaled corticosteroids, and intermittent broad-spectrum antibiotics for the exacerbations of the chronic pneumonia. The follow-up echocardiographic examinations showed progressive pulmonary hypertension. He also experienced a very severe form of varicella. The child succumbed to severe pneumonia with respiratory failure and pulmonary hypertension five years after the diagnosis of the malignant lymphoma. Autopsy was refused by the parents.
2. Discussion
Ataxia telangiectasia is a primary immunodeficiency with autosomal recessive inheritance and worldwide prevalence between 1 : 100 000 and 1 : 300 000 people. The disease is clinically heterogeneous but most patients tend to be wheelchair bound by their teens. Fatal outcome occurs in the fourth or fifth decade of life [1]. The major causes of mortality are pulmonary infections or malignancies [2].
Despite the increased frequency of lymphoid malignancies in A-T patients (up to 100-fold) there are only few reported cases of HD in A-T patients. Sandoval and Swift analyze 11 cases of HD among 412 A-T patients with additional 14 cases described in literature [3]. The reported case contributes with the unusual clinical presentation of HD in a child with a previously undiagnosed immunodeficiency, good response to standard-dose chemotherapy, and late onset of severe radiation-induced pericarditis.
The clinical presentation and imaging studies of HD in this case display some peculiarities. The boy presented with a bulky soft-tissue mass due to lymphonodal coalescence in the posterior mediastinum. It is quite infrequent for HD to be limited only to the mediastinum without any peripheral lymphadenopathy at the time of the diagnosis. This is especially true for the mixed cellularity subtype of the disease diagnosed in our patient. Mixed cellularity was pointed out as the prevailing histological subtype of HD in A-T patients in contrast with the general pediatric population [3, 4]. Involvement of the posterior medistinal or paracardiac lymph node groups is found very rarely in HD [5]. Moreover, most mediastinal tumors are asymptomatic and discovered incidentally by staging X-ray or CT examinations. In our case fever and productive cough were the initial symptoms leading to the misdiagnosis of pneumonia. The recurrent infections and subsequent interstitial progressive pulmonary changes in A-T often mask and delay the diagnosis of a mediastinal HD [6, 7]. In addition, the primary location of the tumor mass in the posterior mediastinum and the elevated AFP and vanylmandelic acid raised the suspicion of a solid tumor. The lack of enlarged peripheral lymph nodes suitable for biopsy was the indication for thoracotomy and partial resection.
Hodgkin’s disease associated with elevated AFP in a child with delayed motor skills and growth should be regarded as the first presenting symptom of A-T. We suspected homozygous ATM mutation two years later after the appearance of other symptoms from the clinical phenotype of A-T (OMIM 208900): increased radiosensitivity, progressive cerebellar ataxia, oculomotor apraxia, and bulbar and skin telangiectasias [8]. A-T was proven by the hypogammaglobulinemia and progressive elevation of AFP—5 to 6 fold above the value at the diagnosis. Age-related increase of AFP in A-T is reported also by other authors [9]. Elevated AFP occurs in about 95% of the A-T patients. Thus, AFP appears to be a reliable diagnostic tool when other causes for its elevation are excluded, keeping in mind that another laboratory evidence like increased chromosomal breakage after radiation exposure of cell cultures or sequencing of the ATM gene is expensive and not routinely available [10, 11].
The basic neuropathology in A-T is degeneration of the Purkinje and granular cells in the cerebellum [12]. It explains the core symptoms of the disease—progressive cerebellar ataxia and oculomotor apraxia, observed in our case. Peripheral neuropathy is another finding in A-T patients explaining the positive Romberg sign and the hyporeflexia of the lower extremities. Choreoathetosis and dystonia become more prominent with increasing age, but they were not observed in our young patient. Mental retardation is not very typical for A-T, but it is observed in about 30% of the A-T cases. Despite the patient’s grossly abnormal neurological status at the time of the CT and MRI examinations, no imaging abnormalities were detected. Commonly, brain MRI in A-T patients may show a nonspecific cerebellar atrophy progressing with age. Therefore the imaging studies may be normal at an earlier age.
The boy had good response without excessive toxicity to standard-dose chemotherapy and sustained remission of the malignant disease. In the general pediatric population HD has a very favorable prognosis with combined multimodality treatment approach, and objectives of contemporary clinical trials are to limit late adverse therapy-related effects [13]. However, the outcome of A-T patients with HD remains poor. The problem of the appropriate chemotherapy regimen is still debated and controversial because of the small series of A-T patients with HD [3, 14]. Our case report supports the opinion that standard chemotherapy regimens are well tolerated [3, 11]. On the other hand, the patient experienced severe radiation-induced complications: esophagitis and pericarditis at a very low total dose of irradiation. Distinctive features of the pericarditis were the long latent period (more than a year) and exudative characteristic, requiring a pericardiotomy and surgical drainage. Usually pericarditis is an early complication of the mediastinal irradiation [15]. The late-onset pericarditis in the general population is mostly constrictive and associated with higher doses of mediastinal irradiation 35–40 Gy [16, 17]. Localization of the skin telangiectasias on the radiation site, as in this case, or on the sun exposed areas, is another marker of radiosensitivity. Thus, the increased radiosensitivity was a cornerstone for suspecting A-T on clinical grounds.
Respiratory infections are the major cause of morbidity and mortality of A-T patients. Steroids may play a role in controlling the chronic pulmonary inflammation and fibrosis. In our case despite the long-term steroid treatment the progressive lung disease led to lethal outcome at the age of nine. The patient did not receive Bleomycin, which could possibly contribute to the progression of the chronic lung disease in A-T [10, 18]. The several episodes of hemoptysis were caused more probably by a severe chronic inflammation rather than by telangiectasias of the respiratory tract. The latter were not proven by the tracheobronchoscopy.
In conclusion, association of incoordination symptoms like ataxia, fine motor delay, and so forth in children with malignant lymphoma should always raise the suspicion of A-T. The timely diagnosis is important to avoid therapeutic irradiation associated with increased radiosensitivity. Chemotherapy is well tolerated by A-T patients with HD at standard doses and schedules.