Propofol sedation without endotracheal intubation is safe for endoscopic submucosal dissection in the esophagus and stomach
Abstract
Background
Endoscopic submucosal dissection (ESD) for early esophageal and stomach cancer is usually performed under general anesthesia. However, propofol sedation without endotracheal intubation has been suggested as a viable alternative.
Objective
The objective of this study was to evaluate the safety of propofol sedation without endotracheal intubation during ESD in the upper gastrointestinal tract.
Methods
We performed a retrospective cohort study of patients who underwent ESD for upper gastrointestinal tumors with propofol-remifentanil analgosedation in a tertiary referral center in the Netherlands between October 2013 and February 2018. Primary endpoints were the rates of intraprocedural endoscopy- and anesthesia-related complications. Secondary endpoints were the postprocedural complication rates within 30 days and endotracheal intubation conversion rates.
Results
Of 88 patients, intraprocedural ESD-related complications occurred in three patients (3.4%). Intraprocedural anesthesia-related complications occurred in two patients (2.3%), one of whom required conversion to endotracheal intubation. Postprocedural ESD-related complications occurred in 14 patients (15.9%), and minor postprocedural complications occurred in two patients (2.3%). Eighty-two (93.2%) patients were discharged within one day after ESD. No patient was readmitted for anesthesia-related complications.
Conclusion
Propofol-based sedation without endotracheal intubation is safe for ESD procedures in the esophagus and stomach with low anesthesia-related complication rates and short hospital stay.
Key summary
- Appropriate sedation and analgesia are required during endoscopic submucosal dissection (ESD) in the esophagus and stomach to limit complications.
- Most ESDs are performed under general anesthesia with endotracheal intubation for continuous airway protection.
- We performed ESD with propofol sedation without endotracheal intubation. Anesthesia-related complications were low (2.3%); only one patient required conversion to endotracheal intubation.
- A total of 93.2% of the patients were discharged within one day after ESD.
- Propofol sedation without endotracheal intubation is safe and feasible for ESD.
Introduction
Endoscopic submucosal dissection (ESD) is a widely used endoscopic resection method for early gastric and esophageal neoplasms that cannot be removed by endoscopic mucosal resection (EMR) or when submucosal invasion is suspected.1,2 ESD enables en bloc resection of the lesion and has a higher curative resection rate than EMR.3-5 However, ESD is difficult and time consuming and can result in pain and discomfort for the patient during the procedure.3,6 Minimal patient movement is preferred, as ESD involves complex and precise maneuvers.7 Therefore, appropriate sedation and analgesia are required to limit complications, such as bleeding or perforation.7-9
Several types of (analgo-) sedation have been used during ESD, ranging from conscious sedation using midazolam or propofol to general anesthesia.10-12 The advantages of propofol over midazolam as a sedative agent are clearly established: fewer movements of the patient during ESD and faster recovery after the procedure because of the short half-life of propofol.10,13-17 Propofol provides stable sedation, and as a result, patients do not experience any restlessness.8,10,13-15,18 Combining remifentanil with propofol as analgosedation improves intraoperative hemodynamic control during painful procedures compared with fentanyl, which is mostly used in combination with midazolam.19 Nowadays, most ESDs are performed under general anesthesia with endotracheal intubation.12,20-22 Aspiration in the course of long-lasting procedures or due to intraprocedural bleeding is a feared complication. The benefit of general anesthesia is continuous airway protection, which may lead to fewer respiratory problems and interruptions during the procedure and therefore fewer endoscopy- and anesthesia-related complications.7,12,23 The downsides of general anesthesia are prolonged postprocedural hospital stay, the need for an anesthesiologist, additional logistic challenges and higher procedural costs.7,12
Currently, there are no guideline recommendations regarding the preferred sedation method during ESD in the esophagus and stomach. We have used propofol-remifentanil analgosedation without endotracheal intubation for ESD in our center since October 2013. In general, in the Netherlands, propofol sedation can be performed by a sedation practitioner (SP) specialized in procedural sedation without the need for an anesthesiologist.24
We hypothesize that ESD can be safely performed with analgosedation using propofol and remifentanil without endotracheal intubation with low endoscopy- and anesthesia-related complication rates. The aim of this study was to report on endoscopy- and anesthesia-related complications of ESDs in the upper gastrointestinal tract to determine the safety of propofol sedation without endotracheal intubation.
Materials and methods
We retrospectively reviewed the medical records of all consecutive patients who were treated with ESD for upper gastrointestinal tumors using propofol-remifentanil analgosedation in a tertiary referral center between October 2013 and February 2018. The study was approved by the medical ethical review committee (MEC-2018-1060).
Anesthesia management
Analgosedation was administered before and during ESD by an SP specialized in procedural sedation (L.L.). The SP is a registered anesthesia nurse having followed an additional theoretical and practical, specialist-supervised training. The SP is responsible for the sedation of the patient and is trained to manage potential medical complications of sedation such as airway and cardiovascular changes. The SP is competent in advanced life-support skills and airway management and understands the pharmacology of the drugs used. The SP is supervised by an anesthesiologist, who is not present in the endoscopy room but on call if necessary. Patients were continuously sedated with intravenous injection of 1%–2% propofol emulsion at a dose of 1–7 mg/kg/hour to achieve a Ramsay Sedation Scale (RSS) score ≥4 (Table 1). Analgesia was obtained with intravenous injection of remifentanil, starting at a dose of 2–9 µg/kg/minute. Additional medications that could be administered during the procedure were glycopyrronium (reduction of mucus secretion), scopolamine butyl (reduction of spasms of the gastrointestinal tract), esketamine (anesthetic), granisetron (anti-emetic), dexamethasone (antiemetic and analgesic) and piritramide (analgesic). Supplemental oxygen was administered via nasal cannula with CO2 monitoring. Heart activity (including five- or six-lead electrocardiography), respiratory rate and RSS were continuously monitored. Blood pressure was monitored every five minutes. Ephedrine or low-dose norepinephrine was administered in case of low blood pressure and atropine in case of bradycardia. Oxygen flow was increased if desaturation occurred until saturation level >95% was achieved.
| 1 | Patient is anxious and agitated or restless, or both. |
| 2 | Patient is cooperative, oriented, and tranquil. |
| 3 | Patient responds to command only. |
| 4 | A brisk response to a light glabella tap or loud auditory stimulus. |
| 5 | A sluggish response to a light glabella tap or loud auditory stimulus. |
| 6 | No response to a light glabella tap or a loud auditory stimulus. |
Sedation parameters were collected from the anesthesiology patient data management system, including anesthesia duration, medications used, and complications. Anesthesia duration was defined as the time between the start of propofol sedation until patient's awakening (RSS of 2).
ESD
All ESDs were performed by a single endoscopist (A.K.), an interventional endoscopist specializing in ESDs. ESD involved marking of the lesion, circumferential mucosal incision and submucosal dissection with simultaneous hemostasis. After circumferential marking of the lesion, a saline solution containing epinephrine (0.01 mg/ml) and indigo carmine was injected into the submucosal layer underneath the lesion to elevate the lesion from the muscular layer. A circumferential incision was made in the mucosa using a HybridKnife® (ERBE Elektromedizin GmbH, Tuebingen, Germany) and the submucosal layer was dissected until the lesion was completely resected. All specimens were reviewed by an expert gastrointestinal pathologist and classified according to the Vienna classification of gastrointestinal neoplasia.25
Data extraction
Patient characteristics such as age, gender, use of anti-coagulation, American Society of Anesthesiologists classification and clinical follow-up were collected from patient medical charts. Endoscopy characteristics such as location of the lesion, Paris classification, lesion size, accomplishment of en bloc resection (defined as a macroscopic complete resection of the lesion in a single specimen), intraprocedural ESD-related complications, and duration of the procedure (defined as the time between the introduction and removal of the endoscope) were collected from endoscopy reports.
Complications
Intraprocedural anesthesia-related complications were defined as oxygen desaturation (SpO2 < 90%), hypotension (systolic blood pressure <80 mmHg), bradycardia (heart rate <50 bpm), apnea or coughing during the procedure that caused an interruption of the procedure or conversion to endotracheal intubation. Intraprocedural ESD-related complications were defined as adverse events (e.g. bleeding or perforation) that caused a change of procedure management, such as discontinuation of ESD. Postprocedural complications comprised all adverse events that resulted in prolonged hospital stay, hospital readmission or additional medical interventions within 30 days.
Statistical analysis
Categorical data are presented as frequencies and percentages. Continuous data are presented as mean (range) and median (interquartile range (IQR)) for normally distributed and skewed data, respectively. Analysis was carried out using IBM SPSS version 24.
Results
A total of 97 ESDs were performed in 96 patients between October 2013 and February 2018 (Figure 1). Three patients received general anesthesia during ESD. In two patients, the procedure was combined with other surgical procedures. In the other patient, the lesion was located near the upper esophageal sphincter, necessitating endotracheal intubation. In three patients midazolam was used as a sedative because procedural time and anticipated technical challenges in relation to small lesion size were estimated to be minimal. Anesthesia reports were missing in three patients. These nine patients were excluded from further analysis. A total of 88 ESDs in 87 patients were included in the final analysis.
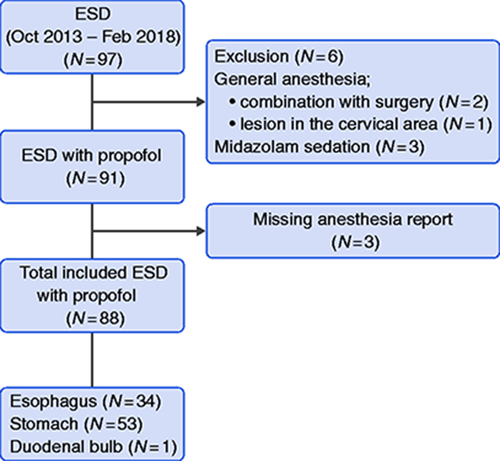
Flowchart of study inclusion.
ESD: endoscopic submucosal dissection.
ESD was performed in the esophagus (34/88; 38.6%), stomach (53/88; 60.2%) and duodenal bulb (1/88; 1.1%) (Figure 1). Baseline characteristics are outlined in Table 2. Median endoscopic procedure time was 100 minutes (IQR: 65–139) and median anesthesia sedation time was 125 minutes (IQR 97–166). Median dose given during the procedure was 403 mg (IQR 272–691) for propofol and 552 µg (IQR 351–552) for remifentanil.
| N (%) | Median (IQR) | |
|---|---|---|
| Age | 70 (60–76) | |
| Sex | ||
| Male | 51 (58.6) | |
| Female | 36 (41.4) | |
| BMI (kg/m3) | 26.3 (22.9–28.7) | |
| ASA score | ||
| I | 10 (11.5) | |
| II | 45 (51.7) | |
| II | 32 (36.8) | |
| Anticoagulant therapy | ||
| Yes | 34 (39.1) | |
| No | 53 (60.9 | |
| Type of anticoagulant therapy | ||
| Antiplatelet drugs | 16 (47.1) | |
| Vitamin K antagonist | 17 (50.0) | |
| Othera | 1 (2.9) |
- ASA: American Society of Anesthesiologists; BMI: body mass index; IQR: interquartile range.
- a Dabigatran.
Tumor characteristics
Tumor characteristics are outlined in Table 3. In seven patients (8.0%), the procedure was discontinued and no histology was obtained (muscular invasion: 5, bleeding: 2). The pathology report was missing for one patient, leaving 80 reports available for analysis. En bloc resection rate was 91% and piecemeal resection was performed in one patient (1.1%). Early cancer was found in 75/80 lesions (94%).
| N (%) | Median (IQR) | |
|---|---|---|
| Histology | ||
| Adenocarcinoma | 42 (52.5) | |
| Squamous cell carcinoma | 18 (22.5) | |
| Neuroendocrine tumor | 1 (1.3) | |
| Gastrointestinal stromal cell tumor | 8 (10.0) | |
| High-grade dysplasia | 6 (7.50) | |
| Low-grade dysplasia | 1 (1.3) | |
| No malignancy | 4 (5.0) | |
| R0 resection | ||
| Yes | 56 (70.0) | |
| No | 17 (21.3) | |
| Unknown | 7 (8.7) | |
| Tumor size, diameter (mm) | 30 (20–40) |
- IQR: interquartile range.
ESD-related complications
The complication rate was calculated for 88 ESD procedures (Table 4). Intraprocedural complications were reported in three procedures (3.4%; all bleeding). In one patient, ESD was converted to EMR and the bleeding was successfully treated with coagulation. In the other two patients, ESD was discontinued and no histology was obtained. One patient received surgical resection, the other patient received chemoradiotherapy as surgical resection was deemed not feasible because of extensive comorbidity. A postprocedural ESD-related complication occurred in 14 patients (15.9%). Six patients developed retrosternal pain for which three patients were given analgesic medication during prolonged hospitalization. One patient was hospitalized one extra day without requiring additional analgesics. A re-endoscopy was performed in two of six patients. In one patient, re-endoscopy after 24 days showed a normal healing ulcer that was treated with sucralfate. The other patient showed candidiasis on re-endoscopy after seven days that was treated with fluconazole. In both patients, no explanation for retrosternal pain was found. Five patients suffered from delayed bleeding. Re-endoscopy was performed in three of these five patients: two without any intervention and one with clip placement for a bleeding ulcer. In two patients, delayed bleeding resulted in prolonged hospitalization without requiring additional intervention. Three patients with delayed bleeding were on anticoagulation therapy, which was discontinued before the procedure. Bleeding occurred after anticoagulation therapy was restarted. Additional postprocedural ESD-related complications were dysphagia (two patients, reendoscopy with esophageal dilation) and gastric pain (one patient, prolonged hospitalization without intervention).
| N (%) | |
|---|---|
| Anesthesia-related complications | |
| Intraprocedural | |
| Coughing | 1 (1.1) |
| Hypotension + desaturation | 1 (1.1) |
| Total | 2 (2.2) |
| ESD-related complications | |
| Intraprocedural | |
| Bleeding | 3 (3.4) |
| Postprocedural | |
| Retrosternal pain | 6 (6.8) |
| Delayed bleeding | 5 (5.7) |
| Stomach pain | 1 (1.1) |
| Dysphagia | 2 (2.3) |
| Total | 14 (15.9) |
| Other postprocedural complications | |
| Nausea | 1 (1.1) |
| Atrial fibrillation | 1 (1.1) |
| Total | 2 (2.2) |
- ESD: endoscopic submucosal dissection.
Anesthesia-related complications
An intraprocedural anesthesia-related complication occurred in two patients (2.3%). One patient coughed, causing a deep laceration in the muscular layer, which was treated with clip placement. The other patient suffered from hypotension and desaturation after a procedure of more than five hours. The anesthesia technique was converted to general anesthesia with endotracheal intubation, and the endoscopic procedure was completed successfully. No postprocedural anesthesia-related complication was observed.
Two postprocedural complications were not clearly anesthesia or ESD related. One patient experienced nausea directly after the procedure, which could be caused by intragastric blood or by sedation with propofol. Nausea disappeared shortly after antiemetic therapy was given. One patient showed atrial fibrillation several hours after the procedure. No clear connection could be established between atrial fibrillation and propofol sedation; the patient was known to have paroxysmal atrial fibrillation. Both patients were discharged the day after the procedure.
Hospital stay
Overall, the mean hospital stay after ESD was 0.9 days (±2.6). Almost half of the patients were discharged the same day as the procedure (43 patients, 48.9%). Thirty-nine patients (44.3%) were discharged the following day: 23 for logistic reasons and 16 for medical reasons. In six patients, hospital stay exceeded two days. No patient was readmitted for anesthesia-related complications.
Discussion
In this retrospective, observational cohort study, we found that ESD for gastrointestinal tumors in the esophagus and stomach could be safely performed with propofol-remifentanil analgosedation without endotracheal intubation. There was no mortality as a result of complications. Conversion to endotracheal intubation took place in one patient only. Coughing was observed in another patient, which brings the intraprocedural anesthesia-related complication rate to 2.3%. Two other minor postprocedural complications were observed that were not obviously anesthesia or ESD related, without additional consequences for the patient. No postprocedural anesthesia-related complications were observed. The intraprocedural ESD-related complication rate was 3.4% and the postprocedural ESD-related complication rate was 15.9%. A total of 93.2% of the patients were discharged the same day or the day after the procedure.
Endoscopy-related complication rates in gastric ESDs range from 1.2% to 5.2% for perforation and 0% to 15.6% for delayed bleeding.26 In ESDs performed in the esophagus, perforation ranges from 0% to 6.9% and delayed bleeding ranges from 0% to 5.2%.27 Although no perforations occurred in our study, the overall postprocedural ESD-related complication rate was still 15.9%, which seems high compared with other studies. However, in our series pain was also considered a complication if this resulted in a longer hospital stay, even one day after the procedure. When taking only perforation and delayed bleeding into consideration, in line with what is reported in most studies, the ESD-related complication rate is 9.1% (8/88). This includes only bleeding in the stomach, which corresponds with the reported range of 0% to 15.6% in the literature.26 Studies in which sedation method was taken into account reported low ESD-related complication rates during ESD when general anesthesia was used. Song et al.12 reported a lower perforation rate in esophageal ESDs in patients receiving general anesthesia compared with those who received propofol sedation (1.2% vs 14.0%). This reported perforation rate of 14.0% when using propofol sedation seems exceedingly high. No perforations were reported in our study. Another study, using general anesthesia, reported no ESD-related complications during esophageal ESD and low complication rates in gastric ESD (bleeding: 1.6% and perforation: 1.7%).7
To judge the safety of ESD in relation to the sedation method used, it would be appropriate to focus on anesthesia-related complications. Several studies reported fewer anesthesia-related complications in patients receiving general anesthesia during ESD. In a study by Yurtlu et al.,23 cough was observed more frequently during ESD in patients receiving propofol compared with general anesthesia (50% vs 5.4%). Likewise, desaturation occurred more often in the propofol sedation group (18.5% vs 2.7%).23 In contrast, we observed cough in only one patient (1.1%). This was likewise for desaturation (1.1%). Other studies in which general anesthesia were used during ESD in the esophagus and stomach reported no hypotension, desaturation or aspiration.7,28 We encountered no hypotension or aspiration either.
The published literature to date indicates that, compared with propofol sedation, the risk-benefit balance is in favor of general anesthesia. It is difficult, however, to discern to what extent the training and experience of the SP plays a decisive role in this equation. In our setting, propofol sedation is managed by an SP, a member of the anesthesiology department who is supervised by the anesthesiologist. Under these conditions, the results of propofol sedation were excellent and only one case required conversion to general anesthesia with endotracheal intubation. Moreover, our anesthesia-related complication rates are lower compared with other studies in which hemodynamic events and respiratory events during propofol sedation were reported to be 37.3% and 14.1%, respectively.29
Another reported advantage of general anesthesia is a shorter procedure time due to fewer interruptions during ESD.28 In that particular study, however, the time between insertion and withdrawal of the endoscope was considered the ESD procedure time without including the time the patient was in the operation room.28 Therefore, the total procedure time including preparation for general anesthesia might be much longer. The median ESD procedure time in the study by Rong et al.,28 in which general anesthesia was used, was 42.5 minutes compared with 100 minutes in our study. This is a huge difference. Rong and colleagues, however, excluded lesions >20 mm in contrast to a median lesion size of 30 mm in our study, which explains this difference. In the same study less body movement and more comfort for the patient were reported as other advantages of general anesthesia.28 In our anesthesia reports, interruptions and body movements were not reported, which precludes further quantitative analysis in our series. According to the SP (L.L.) and the endoscopist (A.K.) who performed all the procedures, no procedure was interrupted because of patient movements. In this retrospective study we could not report on patient satisfaction after the procedure.
This study demonstrates the feasibility and safety of propofol sedation for ESD. This was accomplished with limited hospital admission time with 48.9% of the patients being discharged the day of the procedure and another 44.3% being discharged the day after the procedure. In contrast, other studies in which general anesthesia was used for ESD reported a mean hospital stay of more than four days.7,12,23
Compared with propofol sedation, general anesthesia requires additional facilities, more expertise, and an anesthesiologist.28 Furthermore, most patients cannot be discharged the same day when undergoing the procedure under general anesthesia, which results in a longer hospital stay.7,12,23 Therefore, general anesthesia in all likelihood results in higher costs, although formal cost-effectiveness studies are needed to quantify potential savings in a specific local setting.28
The main strength of this study is that all ESDs were performed by the same endoscopist (A.K.) and by the same sedation practitioner (L.L.), both with extensive experience in this procedure. This limits confounding factors such as experience and technical skills. However, we are aware that such a dedicated team is quite unique in the clinical routine. In particular, an SP is not very common since an anesthesiologist is required in most countries when propofol sedation is used.30 A second strength is that we included all consecutive ESDs in the upper digestive tract between October 2013 and February 2018 performed with propofol sedation regardless of location or size of the lesion.
Some limitations need to be discussed. This is a retrospective, observational, single-center study, which potentially limits the generalizability of our results. There was no comparator group in our study, which could be seen as a limitation. A randomized, controlled trail in which propofol sedation (performed by an SP) is compared with general anesthesia (performed by an anesthesiologist) during ESD is needed to definitively prove the safety of propofol sedation performed by an SP. Owing to the retrospective nature of this study, we did not know the exact number of interruptions during ESD caused by restlessness of the patient. Patient satisfaction could also not be assessed.
Conclusion
In conclusion, in this retrospective, observational, proof-of-concept cohort study, propofol-remifentanil analgosedation without endotracheal intubation proved to be a feasible and safe sedation method for ESD in the esophagus and stomach. Patients could be discharged shortly after the procedure without readmission for anesthesia-related complications. In line with these observations and logistical and financial ramifications, propofol-remifentanil analgosedation without endotracheal intubation for ESD should be considered over general anesthesia when a sedation practitioner is available.
Declaration of conflicting interests
None declared.
Ethics approval
This study was approved by the ethical review board of Erasmus Medical Center, on March 6, 2018 (MEC-2018-1060). The study protocol conforms to the ethical guidelines of 1975 Declaration of Helsinki.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Informed consent
Informed consent was not required, as this was a retrospective study.




