Effect of Three Multisensory Stimulation Modalities on Needle-Related Procedural Pain, Fear, and Anxiety Among Children: Randomized Controlled Trial
Abstract
Aim: This research aimed to measure the effect of three multisensory stimulation modalities (virtual reality, thermomechanical stimulation, and kaleidoscope) on needle-related procedural pain, anxiety, and fear among children.
Background: Effective distraction strategies for pediatric pain management require multisensory stimulation, including visual, auditory, and kinesthetic modalities. These modalities can compete with unpleasant stimuli and promote a positive emotional response. Additionally, thermomechanical stimulation and kaleidoscopes can decrease needle-induced pain, fear, and anxiety in hospitalized children.
Materials and Methods: This randomized controlled trial (RCT) involved 160 children aged 6–12 years, conducted from January 2024 to June 2024 at the inpatient pediatric medical department of Tanta Main University Hospital. Participants were randomly classified into four equal groups (n = 40): a control group receiving no intervention, virtual reality group, Buzzy Bee group, and kaleidoscope group. Data was collected using information from Wong–Baker Faces Pain Rating Scale (WBFPS), Children’s Fear Scale (CFS), and Children’s Anxiety Meter (CAM). The research was approved by the Ethical Committee of Faculty of Nursing, Tanta University.
Results: The virtual reality, Buzzy Bee, and kaleidoscope groups showed significantly lower mean scores in WBS, CFS, and CAM scales compared to the control group. The virtual reality group demonstrated the most significant reduction, with mean pain scores of 1.88 ± 0.463 for children in the virtual reality group compared to 2.05 ± 0.504 for the Buzzy Bee group and 2.55 ± 0.876 for the kaleidoscope group. There was a highly significant (p ≤ 0.001) mean difference in respiratory and oxygen saturation among the control and the intervention groups.
Conclusion: All three distraction methods (virtual reality, Buzzy Bee, and kaleidoscope) effectively reduced procedure-related pain, fear, and anxiety. However, virtual reality was found to be better, outperforming the other methods in terms of pain reduction.
Trial Registration: Pan African ClinicalTrials.gov identifier: PACTR202405799797673
1. Introduction
Pediatric patients often experience pain during hospitalization, primarily because of various nursing and medical procedures involving needle-related procedures such as blood sampling and cannulation. This can cause significant anxiety, fear, and stress for both the children and their parents [1]. Needle phobia, or the extreme fear of needles, can develop as a result of unmanaged pain experienced during invasive procedures [2]. This phobia can significantly affect the children’s lives, leading to avoidance of necessary medical care [3].
Monitoring heart rate, respiratory rate, and oxygen saturation (SpO2) is crucial for pediatric pain assessment. Pain often activates the sympathetic nervous system, leading to tachycardia. Studies have shown that children with chronic pain exhibit a dominant sympathetic response and reduced heart rate variability, indicating decreased parasympathetic activity [4]. Additionally, pain can alter breathing patterns. A systematic review reported that pain influences respiration by increasing frequency, volume, and flow [5]. Severe pain can also lead to decreased oxygen saturation levels. It may cause hypoventilation and muscle tension, and exacerbate underlying respiratory conditions, ultimately resulting in a drop of SpO2 [6].
Anxiety can amplify the experience of pain, leading patients to avoid the situations that caused these sensations. Unmanaged fear, anxiety, and pain can increase the probability of adverse physiological, psychological, and emotional outcomes, such as post-traumatic stress disorders, altered pain perception, chronic pain development, and increased sensitivity to pain. Additionally, it may also lead to reluctance to seek health care in the future [7, 8].
Effective children’s pain management during medical treatment is crucial. A comprehensive, combining pharmacological and nonpharmacological pain-relieving modalities, is often recommended. Many of the nonpharmacological methods can divert children’s attention away from needle-related painful procedures [9]. Distraction techniques, which are common nonpharmacological methods, can effectively manage procedural pain and reduce fear [10]. They work by diverting the child’s attention during painful procedures through various sensory inputs, like olfactory, visual, tactile, auditory, or motor inputs, redirecting their focus from the stressful stimulus to a more pleasant one [11].
Distraction techniques, such as distraction cards, blowing bubbles and applying cold vibration, can effectively reduce pain perception and raise the pain threshold in children [12]. Audiovisual distraction, which engages both the visual and auditory senses, can induce a positive emotional response and promote a sense of relaxation. Virtual reality (VR) technology, in particular, offers multisensory stimulation, that can alter a child’s perception of reality [13, 14]. VR experiences can vary in their level of immersion. Immersive VR provides a complete panoramic view, while nonimmersive VR limits the view based on the device’s movement. The choice of VR experience relies on the child’s preferences and the specific medical procedure [15].
Another effective method for managing pediatric procedural pain is thermomechanical stimulation, which can be achieved by using the Buzzy Bee device. This device is a Bee-shaped gadget that combines external skin cooling with vibration through cold wings. To achieve a mechanical effect, the Bee-shaped device is positioned a short distance away from the needle insertion site [16]. Buzzy Bee blocks the transmission of pain impulses in peripheral nerves by applying a cold effect, which reduces pain severity according to the gate control theory. Presynaptic inhibition in the dorsal horn is thought to impede the fast pain gate when Aβ mechanoreceptors are stimulated concurrently with vibration [17].
A kaleidoscope is another effective distraction technique for pain reduction. It is a toy that uses mirrors and colored objects to create intricate and ever-changing patterns. A kaleidoscope consists of various colored beads arranged between broken mirrors at specific angles. As the beads are turned at eye level, they move and reflect in the mirrors, creating various attractive designs. When a kaleidoscope is rotated, beads move and reflect in the mirrors, creating a mesmerizing, constantly changing pattern of colors and shapes that can effectively capture children’s attention, providing a distraction during the needle-related procedure [18, 19].
Some studies used the previous pain-distracting techniques. Moadad et al. compared the usefulness of Buzzy Bee in decreasing intravenous pain in children diagnosed with cancer. They found that the Buzzy Bee group reported lower pain and anxiety levels compared to the control group [20]. Similarly, Casman et al. evaluated the effectiveness of Buzzy Bee during venipuncture and concluded that it significantly reduced pain and anxiety levels in the study group compared to the control group [21]. Additionally, Faheim and Mahfoz compared the Buzzy Bee to distraction cards during venipuncture in healthy children, reporting higher parental satisfaction and lower pain scores in the Buzzy Bee group [22].
Aditya et al. investigated the effectiveness of three distraction techniques, a kaleidoscope, VR, and a fidget spinner, in reducing children’s anxiety levels during dental procedures. Anxiety was assessed using the Venham picture test (VPT), oxygen saturation (SpO2), and pulse rate. All three distraction techniques significantly reduced anxiety levels compared to the control group. The fidget spinner was most effective, followed by VR and kaleidoscope. The control group exhibited the highest anxiety levels and pulse rates. SpO2 levels did not differ significantly across groups. The study highlighted the importance of using simple, cost-effective, and noninvasive techniques to reduce anxiety in children. The authors also recommended further research with a larger sample size and additional assessment tools [23].
Similarly, Akarsu et al. investigated the effectiveness of VR and tablet-based carton distraction methods in reducing pain, fear, and anxiety in children aged 5–12 years undergoing various blood draws in the pediatric emergency unit. The findings highlight the potential effectiveness of tablet-based cartoons and VR as effective nonpharmacological methods for alleviating procedural distress in pediatric patients. However, the study also identifies a gap in the literature regarding the direct comparison between VR and other pain-distracting techniques, emphasizing the need for further research in this area [24].
Nurses play a crucial role in pediatric pain management by introducing children to pain distraction techniques such as Buzzy Bee, Kaleidoscopes, and VR. However, many nurses may lack sufficient knowledge, training, or access to resources necessary to implement these techniques effectively, which may limit their use in clinical practice. To ensure optimal outcomes, nurses must possess the required skills and knowledge to guide children in self-applying these techniques, which can significantly reduce pain and anxiety [25].
Despite the growing recognition of pain distraction techniques in pediatric care, there remains a gap in the literature regarding the effectiveness of various methods across different pediatric populations and healthcare settings [26]. Addressing this gap, this study aims to assess the effects of three multisensory stimulation modalities (VR, thermomechanical stimulation, and kaleidoscope) on needle-related procedure pain, fear, and anxiety in pediatric patients. By evaluating and comparing these interventions, this research seeks to identify the most effective strategies for managing pediatric needle-related pain.
1.1. Research Hypothesis
-
H1: Children receiving VR, Buzzy Bee, and kaleidoscope will experience lower needle-related procedure pain, fear, and anxiety compared to children in the control group.
-
H2: Children receiving VR, Buzzy Bee, and kaleidoscope will experience more stable physiological parameters (lower heart rate, respiration, and higher oxygen saturation) measured by pulse oximeter compared to children in the control group.
2. Methods
2.1. Design and Setting
This research was designed as a prospective, randomized controlled trial (RCT) conducted in the blood testing room of the inpatient pediatric medical ward of Tanta Main University Hospital, associated with the Egyptian Ministry of Higher Education. The study design followed the CONSORT 2010 statement [27] and included four groups.
2.2. Participants
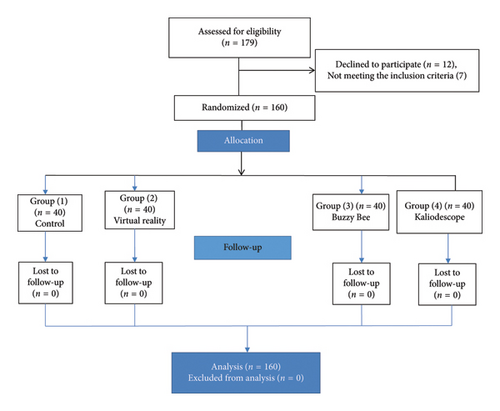
A power analysis using G∗Power was used to estimate the necessary sample size to identify a significant difference with an effect size of 0.40, a significance level of 0.05, and a power of 85%. The calculation indicated 40 children per group, for a total of 160 participants. Between January and June 2024, 179 children aged 6–12 were assessed for eligibility. Twelve children declined to participate, and seven children did not meet the study’s inclusion criteria.
To be included in the study, the child should undergo needle-related procedures such as blood draws, IV punctures, and IV cannulations, be able to use electronic devices, and be able to report pain. Additionally, children must be between 6 and 12 years old. This age range was chosen based on the cognitive stage of these children, which is the concrete operational stage that allows them to understand and follow instructions more effectively, and they are more capable of expressing their feelings and understanding the concept of pain, making them suitable participants for pain-related research. Also, younger children tend to experience higher levels of procedural anxiety than adolescents. Adolescents typically develop more advanced coping strategies, allowing them to manage anxiety more effectively during medical interventions.
Children were excluded if they had epilepsy, were unable to maintain a sitting or semi-upright position during the procedure (due to the VR device requiring a minimum head-tracking angle of 30°), or had mental disabilities that prevented the interaction with the researcher. Children with peripheral vascular disease, connective tissue disease, diabetic neuropathy, birth defects, central nervous system disease, visual and hearing impairment, and altered level of consciousness are excluded also from participation in the study.
- •
Group 1: Control group (no intervention)
- •
Group 2: VR (VR)
- •
Group 3: Buzzy Bee
- •
Group 4: Kaleidoscope
This randomization method helped to minimize bias and ensure that participants were evenly distributed across the groups (Figure 1 shows the flow diagram of sampling).
2.3. Ethical Consideration
The Ethical Committee of Faculty of Nursing, Tanta University (Number: 273.6.2023) approved the study. Prior to participation, children and their parents were informed about the study’s objective, intervention methods, and the right to withdraw from the study at any time without facing any consequences. Written informed consent was obtained from parents, and verbal consent was obtained from children, ensuring their understanding and voluntary participation in the research.
2.4. Instruments
Data was collected by the researchers using information from Wong–Baker Faces Pain Rating Scale (WBFPS), Children’s Fear Scale (CFS), Children’s Anxiety Meter (CAM) scale, and noninvasive pulse oximeter.
The information form, developed by the researchers after a comprehensive literature review, was reviewed by three pediatric nursing experts to establish content validity. The final form consisted of three sections: demographic information (child’s age and gender, mother’s age and education), child’s medical history (cause for admission, previous hospitalization, and venipunctures within the past 3 months), and physiological parameters (child’s heart rate, respiratory rate, and SpO2, measured noninvasively using a pulse oximeter as recommended by Le May et al. and Castarlenas et al. [28, 29].
Children’s perception of needle-related pain was assessed using the WBFPS. The scale is reliable and valid for determining procedure pain intensity in children between 3 and 18 years old [30] and has been used in several Egyptian studies [31, 32]. The freely accessible WBFPS consists of six cartoon faces depicting pain intensity, ranging from a neutral expression (no pain) to a crying face (severe pain). The children were asked to select the face that best represents their pain experience. The scale uses a numerical anchor, with 0 representing “no pain” and 10 representing “too severe pain”. In this study, the WBFPS demonstrated a Cronbach’s alpha coefficient of 0.89.
Procedural fear was assessed using the CFS. It is a self-report measure developed by McMurty et al. [33] and used to assess children’s fear levels during acute pain. The scale consists of five cartoon faces indicating varying levels of fear, with the left-most face marked as 0, with an expression said by the developers to show no fear, and the face on the far right marked as 4, demonstrating the most serious degree of fear. The scores ranged from 0 to 5. The scale has been used in Egypt previously [34]. The reliability was tested using Cronbach’s alpha test (r = 0.96).
Children’s anxiety level was assessed using the CAM scale developed by Kleiber et al., to evaluate anxiety in children before a medical procedure [35]. The CAM scale is a visual analog scale resembling a vertical mercury thermometer with a bulb at the bottom and horizontal lines at intervals going up to the top. The grades ranged from 0 to 10, with higher grades indicating greater levels of anxiety [36]. Children were asked to show their anxiety level by pointing to the corresponding mark on the thermometer. The value of Cronbach’s alpha coefficient was 0.881.
2.4.1. Noninvasive Pulse Oximeter
The noninvasive pulse oximeter with 99% accuracy was used to measure the heart rates and oxygen saturation levels of children. These values were recorded 1 min before, during, and after the procedure in all the study groups (Figure 2).

2.5. Data Collection Procedures
- •
Data collection occurred during the morning shift (8 a.m.–2 p.m.).
- •
Mothers in all groups were present during the needle-related procedures.
- •
The researcher explained the study to mothers and children.
- •
All Procedures are conducted in a specialized room for needle-related procedures.
- •
A single highly experienced nurse (with at least 3 years of experience in pediatric needle-related procedures) performed all procedures using the child’s nondominant hand.
- •
Mother completed an information form.
- •
The researcher completed the WBFPS, CFS, and CAM.
- •
5 min before the procedure, the researcher recorded the child’s physiological parameters (heart rates, oxygen saturation levels, and respiration).
- •
Children in the three intervention groups were given a 3-min acclimation period to familiarize themselves with the distraction aid before the needle-related procedure.
After the first 30 min of the study, each group followed a specific protocol.



2.5.1. Control Group
- •
Before blood collection, children in the control group underwent the needle-related procedure following the standard unit routine practice. This included a detailed explanation of the procedure and the use of comforting words and positive verbal reinforcements for 3 min before the procedure began.
- •
When the needle enters the vein, from minute 4 to minute 8, the nurse performs the procedure, and the researcher records the children’s physiological parameters at minute 6.
2.5.2. VR Group
- •
Before blood collection, children were seated and fitted with VR goggles (immersive 3D experience, manufactured in China) and a tracking system (intersperse 1S300 6-6-degree of freedom inertia Cube with a USB-Serial converter, required for the Inertia Cube). The headset featured a wide field of view, a high-resolution display, and an adjustable head strap for comfort, ensuring an engaging and distraction-based intervention. This setup allowed children to interact with the virtual environment by moving their head and neck.
- •
The children watched an animated comedy short film called “Big Buck Bunny” which was freely downloaded from YouTube and created by the Blender Institute. The video provided a visual simulation, aiming to give the children a sense of being in a forest with its creatures, including fruits, butterflies, trees, water, rodents, and various traps. Figure 3 illustrates a scene from the film. This video was selected to provide effective distraction by creating a deeply engaging experience, utilizing nonviolent and simplified natural scenes without movement during the invasive procedure [37].
- •
When the needle enters the vein, from minute 4 to minute 8, the nurse performs the needle-related procedure, and the researcher records the children’s physiological parameters during the procedure at minute 6. At minute 8, the VR video was stopped, the goggles were removed, and the equipment was disinfected.
2.5.3. Thermomechanical Stimulation (Buzzy Bee) Group
- •
Before blood collection, the Buzzy Bee (Figure 4) wings were frozen for 10 min before the procedure. Before application, the device was disinfected with 70% alcohol and placed on the child’s arm at the injection site. The vibration feature was activated before applying the device to the child’s arm. The Buzzy Bee was attached to the injection site for 1 min.
- •
When the needle enters the vein, the researcher moves the Buzzy Bee 3 cm above the injection site while maintaining vibration for an additional 3 min during the procedure. The researcher recorded the child’s physiological parameters during the procedure at minute 5.
2.5.4. Kaleidoscope Group
- •
Before blood collection, the kaleidoscope (Figure 5) was provided 3 min before the needle-related procedure, allowing the child to engage with changing shapes.
- •
When the needle enters the vein, the child held the kaleidoscope with his free hand, looked through the eyepiece with one eye to make sure proper positioning. The researcher instructed the child to focus on the center of the image to see the pattern, while the mothers were asked to slowly rotate the kaleidoscope. The needle-related procedure took place from minute 4 to minute 8. The researcher recorded the child’s physiological parameters during the procedure at minute 6.
- •
At minute 10, the researcher recorded physiological parameters, including heart rate, oxygen saturation (SpO2), and respiration rate.
- •
Pain, fear, and anxiety levels were then assessed using the WBFPS, CFS, and CAM.
- •
All equipment was cleaned using disposable wipes and alcohol swabs and allowed to air dry for at least 20 min between participants to ensure proper disinfection.
VR goggle: VR box 2.0 3d VR glasses with lens adjustment and focus control (Figure 3).
2.6. Data Analysis
The data was analyzed using the Statistical Package for Social Sciences (SPSS) program version 28. Descriptive statistics, including mean, standard deviation, frequency, and percentage distribution, were calculated to summarize the data. Due to the nonnormal distribution of the WBFPS, CFS, and CAM scores, the Kruskal–Wallis H test was used to determine the difference between the four groups. The Mann–Whitney U test with Bonferroni correction was used for pairwise comparisons to identify the specific groups contributing to observed differences [38].
3. Results
3.1. Participants’ Demographic Characteristics
The mean age of the children in the control, VR, Buzzy Bee, and kaleidoscope groups was 8.03 ± 1.46, 7.91 ± 1.44, 8.02 ± 1.454, and 8.10 ± 1.34, respectively. Gender distribution was relatively balanced, with approximately half of the children in each group being male (control = 60%; VR = 52.5%, Buzzy Bee group = 57.5%, and kaleidoscope group = 50%). Regarding geographic location, 55%, 52.5%, 55%, and 57.5% of participants in the control group, VR group, Buzzy Bee group, and kaleidoscope group, respectively, came from urban areas. In terms of education, 65%, 57.5%, 60%, and 52.5% of children in these groups, respectively, were from 1st- to 3rd-grade schools.
The mean age of mothers in the control, VR, Buzzy Bee group, and kaleidoscope group was 30.62 ± 5.75, 30.42 ± 5.66, 31.21 ± 5.70, and 30.47 ± 5.556, respectively. Additionally, 40%, 52.5%, 42.5%, and 55.5% of mothers held a secondary school certificate in the control, VR, Buzzy Bee group, and kaleidoscope group, respectively. A summary of the sample characteristics is shown in Table 1.
| Characteristics | Control group (n = 40) | VR group (n = 40) | Buzzy Bee group (n = 40) | Kaleidoscope group (n = 40) | t-value | p value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |||||||
| Children’s age (mean ± SD) | 8.04 ± 1.46 | 7.91 ± 1.44 | 8.02 ± 1.45 | 8.10 ± 1.34 | 0.283∗ | 0.963 | ||||
| Mother age (mean ± SD) | 30.62 ± 5.75 | 30.42 ± 5.66 | 31.21 ± 5.70 | 30.47 ± 5.55 | 0.713∗ | 0.870 | ||||
| Children’s gender | ||||||||||
| Boy | 24 | 60.0 | 21 | 52.5 | 23 | 57.5 | 20 | 50.0 | 1.004∗∗ | 0.800 |
| Girl | 16 | 40.0 | 19 | 47.5 | 17 | 42.5 | 20 | 50.0 | ||
| Residence | ||||||||||
| Urban | 22 | 55.0 | 21 | 52.5 | 22 | 55.0 | 23 | 57.5 | 0.201∗∗ | 0.977 |
| Rural | 18 | 45.0 | 19 | 47.5 | 18 | 45.0 | 17 | 42.5 | ||
| Children’s education | ||||||||||
| 1st–3rd grade | 26 | 65.0 | 23 | 57.5 | 24 | 60.0 | 21 | 52.5 | 1.426∗∗ | 0.699 |
| 4th–5th grade | 14 | 35.0 | 17 | 42.5 | 16 | 40.0 | 19 | 47.5 | ||
| Mothers’ education | ||||||||||
| Read and write | 16 | 40.0 | 21 | 52.5 | 17 | 42.5 | 22 | 55.5 | 2.996∗∗ | 0.392 |
| Secondary school | 17 | 42.0 | 15 | 37.5 | 17 | 42.5 | 14 | 35.0 | ||
| Bachelor’s degree | 7 | 17.5 | 4 | 10.0 | 6 | 15.0 | 4 | 10.0 | ||
- Abbreviation: SD = standard deviation.
- ∗Z; Kruskal–Wallis Test.
- ∗∗Pearson chi-square.
3.2. Participant’s Medical History
Table 2 presents the medical history of the 160 children participating in the study, categorized into four groups: Control, VR, Buzzy Bee, and kaleidoscope. The most common reason for hospitalization was chest problems affecting 45% of the children in the control group, 30% of the VR group, 30% of the Buzzy Bee group, and 35% of the kaleidoscope group. Additionally, approximately 37%, 40%, 45%, and 35% of the children in the control, VR, Buzzy Bee, and kaleidoscope groups, respectively, had less than three venipunctures in the last 3 months.
| Group | Control group (n = 40) | VR group (n = 40) | Buzzy Bee group (n = 40) | Kaleidoscope group (n = 40) | t | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |||
| The reason for admission | ||||||||||
| Chest problem | 18 | 45.0 | 12 | 30.0 | 12 | 30.0 | 14 | 35.0 | 3.089 | 0.378 |
| Renal problem | 10 | 25.0 | 13 | 32.5 | 13 | 32.5 | 11 | 27.5 | ||
| Hepatic problem | 6 | 15.0 | 5 | 12.5 | 5 | 12.5 | 6 | 15.0 | ||
| Endocrine problem | 4 | 10.0 | 5 | 12.5 | 5 | 12.5 | 5 | 12.5 | ||
| Metabolic problem | 2 | 5.0 | 5 | 12.5 | 4 | 10.0 | ||||
| Number of venipuncture for last 3 months | ||||||||||
| No | 9 | 22.5 | 8 | 20.0 | 6 | 15.0 | 6 | 15.0 | 3.126 | 0.373 |
| Less than 3 | 15 | 37.5 | 16 | 40.0 | 18 | 45.0 | 14 | 35.0 | ||
| 3–5 | 8 | 20.0 | 8 | 20.0 | 6 | 15.0 | 8 | 20.0 | ||
| More than 5 | 8 | 20.0 | 8 | 20.0 | 10 | 25.0 | 12 | 30.0 | ||
- Note: Pearson Chi-square.
- Abbreviation: SD = standard deviation.
- ∗∗p ≤ 0.001 highly significant.
3.3. Comparison of Pain, Fear, and Anxiety Scores Across the Four Groups
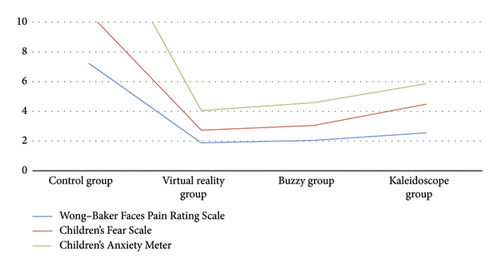
Table 3 presents the mean scores for the WBFPS, CFS, and CAM across the four groups (n = 160). A statistically significant difference was found between the four groups in terms of pain scores (p ≤ 0.001). The mean pain scores of children in the control group, as measured by WBS and CFS, were higher compared to those in the VR, Buzzy Bee, and kaleidoscope groups. Among the intervention groups, children in the kaleidoscope group reported higher mean pain scores than those in the VR and Buzzy Bee groups (p ≤ 0.001).
| Variables | Control group (n = 40) | VR group (n = 40) | Buzzy Bee group (n = 40) | Kaleidoscope group (n = 40) | Z:P | Post-hop test |
|---|---|---|---|---|---|---|
| M ± SD | M ± SD | M ± SD | M ± SD | |||
| Wong–Baker Faces Pain Rating Scale | 7.23 ± 1.230 | 1.88 ± 0.463 | 2.05 ± 0.504 | 2.55 ± 0.876 | 114.836; < 0.001 | a > d > c, b |
| Children’s Fear Scale | 3.38 ± 0.667 | 0.85 ± 0.5.33 | 1.00 ± 0.679 | 1.93 ± 0.829 | 105.001; < 0.001 | a > d > c, b |
| Children’s Anxiety Meter (CAM) | 7.15 ± 1.075 | 1.23 ± 0.832 | 1.53 ± 0.640 | 1.38 ± 0.807 | 97.448; < 0.001 | a > c > d > b |
- Note: Z; Kruskal–Wallis test.
Regarding children’s fear, measured by the CFS, the results indicate that there were statistically significant differences in CFS scores among the four groups (p ≤ 0.001) indicating that the intervention groups (VR, Buzzy Bee, and kaleidoscope) were more effective in reducing children’s fear compared to the control group. Children in the control group reported significantly higher levels of fear than those in the intervention groups. Among the intervention groups, the VR group consistently reported the lowest levels of fear, followed by the Buzzy Bee and kaleidoscope groups (see Table 3).
Figure 6 visually represents the mean scores of WBFPS, demonstrating a significant decrease in pain levels for the VR group (1.88 ± 0.463) followed by Buzzy Bee group (2.05 ± 0.504) and kaleidoscope group (2.55 ± 0.876). The control group exhibited significantly higher pain levels (7.23 ± 1.230). Similarly, the mean scores of the CAM scale in the control group were higher than those in the VR, Buzzy Bee, and kaleidoscope groups (p ≤ 0.001). The mean scores of the CAM scale among children in the Buzzy Bee group were higher than those in the VR and kaleidoscope groups (p ≤ 0.001).
3.4. Comparison of Physiological Parameters (Heart Rate, Respiratory Rate, and Oxygen Saturation) Across the Four Groups During Needle-Related Procedure
Table 4 presents the mean scores for heart rate, respiratory rate, and oxygen saturation (SpO2) across the four groups during the needle-related procedure. The control group had the highest mean heart rate during the procedure (108.98 ± 4.376), followed by the kaleidoscope group (109.53 ± 3.776), the Buzzy Bee group (109.33 ± 4.215), and the VR group (109.28 ± 4.095). Similarly, the control group exhibited the highest mean respiratory rate during the procedure (32.73 ± 2.025), followed by the kaleidoscope group (31.75 ± 2.519). The VR and Buzzy Bee groups had comparable respiratory rates (30.68 ± 1.953). Oxygen saturation levels were slightly lower during the procedure compared to baseline in all groups. The control group had the lowest mean oxygen saturation (95.80 ± 1.067), while the kaleidoscope group had the highest (96.98 ± 1.250). Overall, the procedure had a notable impact on heart rate and respiratory rate, with the control group experiencing the most significant elevations. There were statistical significant differences among the three groups regarding mean scores of heart rate after procedure, p = 0.006, mean score of respiratory rate during and after procedure, p ≤ 0.001 & p = 0.005, respectively, and also regarding O2 saturation during and after procedure p ≤ 0.001 & p = 0.020, respectively.
| Physiological parameter | Control group (1) (n = 40) | VR (2) group (n = 40) | Buzzy Bee group (n = 40) | Kaleidoscope group (n = 40) | Total of four groups | p value |
|---|---|---|---|---|---|---|
| M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | ||
| Heart rate | ||||||
| Before | 108.98 ± 4.376 | 109.28 ± 4.095 | 109.33 ± 4.215 | 109.53 ± 3.776 | 109.28 ± 4.117 | 0.947 |
| During | 114.85 ± 3.793 | 109.13 ± 16.499 | 109.13 ± 16.499 | 111.53 ± 3.404 | 111.16 ± 12.060 | 0.108 |
| After | 113.10 ± 3.986 | 110.73 ± 3.672 | 110.73 ± 3.672 | 110.55 ± 3.515 | 111.28 ± 3.830 | 0.006∗ |
| Respiratory rate | ||||||
| Before | 27.43 ± 1.534 | 27.50 ± 1.519 | 27.40 ± 1.566 | 27.75 ± 1.446 | 27.52 ± 1.509 | 0.987 |
| During | 32.73 ± 2.025 | 30.68 ± 1.953 | 30.68 ± 1.953 | 31.75 ± 2.519 | 31.46 ± 2.273 | 0.001∗ |
| After | 31.10 ± 1.751 | 30.00 ± 1.519 | 30.00 ± 1.519 | 30.83 ± 1.999 | 30.48 ± 1.763 | 0.005∗ |
| SpO2 | ||||||
| Before | 96.80 ± 1.067 | 97.05 ± 1.154 | 96.93 ± 1.047 | 97.10 ± 0.928 | 96.97 ± 1.049 | 0.778 |
| During | 95.80 ± 1.067 | 96.35 ± 1.252 | 96.40 ± 1.277 | 96.98 ± 1.250 | 96.38 ± 1.273 | 0.001∗ |
| After | 96.33 ± 1.269 | 96.70 ± 1.324 | 96.75 ± 1.335 | 97.25 ± 1.316 | 96.76 ± 1.340 | 0.020∗ |
- Note: One-way ANOVA.
- Abbreviation: SD = standard deviation.
- ∗∗p ≤ 0.001 highly significant, ∗p ≤ 0.05.
4. Discussion
Nonpharmacological interventions are crucial in controlling pain, anxiety, and fear experienced by children undergoing needle-related procedures. VR, Buzzy Bee, and kaleidoscopes are examples of nonpharmacological measures that are safer and have fewer or no side effects than pharmacological measures. Aditya et al. (2021) emphasize the importance of effective distraction techniques that require multiple senses, active involvement, and pediatric patient participation [23].
Among the intervention groups, the VR group demonstrated the most significant reduction in pain, fear, and anxiety as measured by the WBFPS, CFS, and CAM scale. This result can be attributed to the immersive, multisensory nature of the VR technology, which can modify users’ perceptual experiences and promote relaxation. Supporting this finding, Özkan and Polat and Wong et al. concluded that the pain and anxiety scores were markedly lower for the VR group compared to the control group, and these results further emphasize the effectiveness of VR in providing both audiovisual and sense-perception distraction [39, 40].
Akarsu et al. aligned with the present findings, reporting a decrease in pain, fear, and anxiety perception among children using VR during blood draws [24]. Zhao et al. and Tüfenk and Büyük similarly supported the effectiveness of VR in reducing fear associated with medical procedures and preventing severe pain sensitivity, anxiety, and medical avoidance in both adults and children [41, 42]. A recent systematic review by Tas et al. demonstrates the efficacy of VR as a tool for reducing pain and anxiety in children undergoing various medical procedures [43].
The Buzzy Bee device, which combines cold and vibration to provide thermo-mechanical stimulation, was also found to significantly reduce procedural pain and anxiety. This supports the previous research by Moadad et al., Casman, et al., and Fahiem and Mahfoz, who reported reduced pain and anxiety in children undergoing venipuncture or intravenous procedures when the Buzzy Bee was used [20–22].
In an RCT, Erdogan and Aytekin (2021) reported that children who used the Buzzy Bee had the lowest mean pain score, according to child, parent, and researcher ratings [45]. Merino-Lobato et al. further confirmed the Buzzy Bee efficacy as an analgesic and anxiolytic [46]. Semerci et al. found that children who received Buzzy Bee distraction had lower average pain, current anxiety, and fear scores compared to those without distraction [47]. Bilgen Sivri et al. and Sahiner et al. recommended that nurses use the Buzzy Bee method to reduce venipuncture pain and fear in children [48, 49].
Our results showed that kaleidoscope is another effective method that helps to reduce pain, fear, and anxiety among children. Previous research has supported the use of kaleidoscopes as a distraction aid during medical procedures [50, 51]. The kaleidoscope affordability and ability to create captivating visual displays make it a valuable tool for distracting children from pain [50, 51]. Canbulat et al. and Kunjumon observed a reduction in pain levels among children using kaleidoscope compared to the control group [52, 53]. Similarly, Karakaya and Gözen’s found that kaleidoscope distraction was effective in reducing venipuncture pain [54]. However, Aditya et al. noted that kaleidoscope may be less effective than VR due to its limited field of view and the potential for discomfort with use [23].
Pulse rate, respiratory rate, and SpO2 are important physiological measures for children’s pain assessment. In the current study, statistically significant differences were observed between the intervention group and the control group. The control group had the highest mean heart rate during the procedure, followed by the kaleidoscope group, the Buzzy Bee group, and the VR group. Aditya et al. observed a similar pattern, with the highest mean pulse rate in the control group, closely followed by the kaleidoscope group, although the results were nonsignificant. There were statistically significant differences in SpO2 levels among all the groups. The control group had the lowest mean oxygen saturation, while the kaleidoscope group had the highest. This result contrasts with the findings reported by Aditya et al., who found no statistically significant difference in SpO2 levels among VR, kaleidoscope, and control groups [23].
5. Conclusion
According to the results of this study, VR, Buzzy Bee, and kaleidoscope were demonstrated to successfully decrease procedure-related pain in children. These nonpharmacological interventions offer effective and safe alternative pain relief methods, with no reported side effects.
6. Limitations
This study has several limitations that should be considered when interpreting the findings. One limitation is that the sample was not stratified by gender, which may have influenced the results, as gender differences can affect pain perception and anxiety levels. Additionally, the study was conducted in a single hospital, which may limit the generalizability of the findings to other settings or populations. Another limitation was the lack of blood pressure measurement, which could have provided an additional objective indicator of anxiety levels alongside pulse rate and self-reported measures. Lastly, due to the nature of the interventions, blinding of participants, research assistants, nurses, and the statistician was not feasible. Further studies are recommended to use gender-stratified samples, include multiple hospital settings, incorporate more physiological measures, and explore methods to reduce bias from a lack of blinding.
7. Implications
The results of this research study have important implications for nursing practice in the realm of pediatric pain management. By demonstrating the effectiveness of nonpharmacological interventions like VR, Buzzy Bee, and kaleidoscopes, the study expands the range of options available to nurses, reducing reliance on potentially harmful medications and enhancing patient experience. These interventions can improve patient satisfaction and trust in healthcare providers while promoting evidence-based decision-making among nurses. By offering a variety of pain management options, nurses can better accommodate individual patient preferences and needs, leading to more personalized and effective care. Ultimately, the study contributes to advancing pediatric pain management and improving the quality of care given to young patients.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
No funding was received for this manuscript.
Acknowledgments
We would like to express our gratitude to the children, parents, and healthcare professionals who participated in this study.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.




