Analyzing Autonomy in Critical Care Nursing: Unveiling the Distinctive Aspects
Abstract
Background: Autonomy embodies self-governance, self-directed freedom, moral independence, and an individual’s discretion in task performance. The current literature suggests that autonomy among nurses is becoming more common in nursing practice. Professional autonomy, integral to nursing, signifies nurses’ capacity to transcend conventional care standards. Nurses play the most significant role in patient care outcomes among healthcare professionals. Autonomy fosters critical thinking, facilitating interpretation, reasoning, analysis, and evaluation. This encourages problem-solving and innovation in patient care.
Purpose: This concept analysis explores and describes the concept of autonomy among critical care nurses and provides a conceptual definition to enhance understanding of autonomy within this context.
Methods: Using search engines, we extensively explored existing knowledge on autonomy in critical care nursing. We then applied Walker and Avant’s eight-step method to analyze autonomy in this nursing context.
Findings: The findings suggest that autonomy is integral to nursing professionalism. The analysis covers attributes, antecedents, and consequences linked with autonomy among critical care nurses. Model, borderline, and contrary cases are presented to illustrate the concept.
Conclusion: Nursing autonomy is a multifaceted concept. This analysis deepens the understanding of autonomy in critical care nursing, encompassing independent clinical decision-making, accountability, critical thinking, and a process-oriented approach. Various factors contribute to the effective application of autonomy in critical care nursing, including educational competence, comprehensive knowledge of critical care nursing practices, and educational qualifications like higher degrees in nursing.
1. Introduction
Autonomy is a state of self-governance, self-directed freedom, moral independence, or a level of discretion an individual possesses to perform their tasks [1]. The current literature suggests that autonomy among nurses is becoming more common in nursing practice. Professional autonomy has been defined as the ability of a nurse to go beyond the status quo regarding the care of their patients [2]. Traynor [3] discusses that professional autonomy is the primary descriptor in any professional organization. Skår [4] stipulates that autonomy is the power of professionals to make independent decisions and the freedom to practice based on formal professional knowledge, experience, and judgment. Nursing literature emphasizes the ideology of autonomy, which includes authority, independence, professional limitations, and a degree of freedom from unnecessary interference by other professions. However, the extent to which individual nurses understand and exercise autonomy varies based on their role, experience, and workplace policies.
Among healthcare professionals, nurses play the most significant role in patient care outcomes [5]. The year 2020 was celebrated as the Year of the Nurse and Nightingale. The COVID-19 pandemic placed nurses in the public eye more than ever [6]. The public image of nursing is often stereotyped as compassionate helpers, doctors’ assistants, and a “doing” profession [6, p. 180]. The nursing profession is complex and extends beyond the traditional perception of nurses as merely compassionate caregivers, encompassing clinical expertise, leadership, and critical decision-making. Contemporary nursing continues to reflect on the epistemology of care, challenging traditional views and embracing new modes of self-image where the nursing profession is defined and projected based on historical perspectives [7]. Autonomy is a key factor in professional organizations, and nurses must navigate autonomy-related challenges and limitations within the evolving healthcare landscape of the 21st century.
The COVID-19 pandemic has underscored the nursing profession’s challenges, particularly the need to establish and maintain a suitable work environment for nurses. According to Gottlieb et al. [8], job satisfaction has become a crucial predictor of nursing retention. Nurse autonomy has been strongly linked to job satisfaction. The research indicates that leadership styles significantly influence nurses’ perceived autonomy and their ability to make independent clinical decisions. Professional autonomy develops over time and is supported by patient-centered competence, organizational policies, and healthcare structures. It involves self-reliance in delivering optimal patient care, promoting patient health through independent decision-making, and collaborating with other healthcare professionals [5].
Intensive Care Units (ICUs) for critically ill patients, where nursing autonomy is not just an abstract but a crucial factor influencing patient outcomes. In this high-stress, fast-paced environment, critical care nurse autonomy fosters advanced clinical reasoning, increased professional accountability, and informed decision-making [9]. However, the concept of autonomy within critical care nursing remains ambiguous in the current literature. Oshodi et al. [10] conducted a descriptive phenomenological study exploring nurses’ experiences and perceptions of autonomy. Their findings reveal that nurses associate autonomy more closely with their specific clinical roles than with broader professional responsibilities. Exploring the concept of autonomy among critical care nurses is vital to understanding its impact on the advancement of patient care, critical thinking in nursing, accountability, job satisfaction, empowerment, and professional growth. How is autonomy conceptualized and operationalized among critical care nurses, and what are its defining attributes in this context? This paper aims to analyze and highlight the distinctive aspects of autonomy among critical care nurses, offering a conceptual definition to enhance the understanding of autonomy within this specific nursing context. Professionalism and professional behavior are crucial in today’s medical sciences. To meet an evolving healthcare system, nursing must continually adapt and advance in epistemology and axiology.
2. Methods
2.1. Concept Analysis Method
The systematic methodology of concept analysis serves to define and clarify abstract or ambiguous concepts. This analysis breaks down each concept into its fundamental components to reveal its internal structure. By eliminating ambiguity, concept analysis facilitates a precise understanding and enables the creation of operational definitions that validate the concept. Walker and Avant’s approach to concept analysis consists of eight steps: (1) selecting a concept, (2) defining the purpose of the analysis, (3) examining all variations of the concept’s usage, (4) identifying the key attributes, (5) creating a model case, (6) identifying borderline, related, and opposing cases, (7) analyzing antecedents and consequences, and (8) establishing empirical referents [11]. Researchers can use this method to investigate the antecedents, attributes, and consequences of autonomy in critical care settings [12].
2.2. Search Method
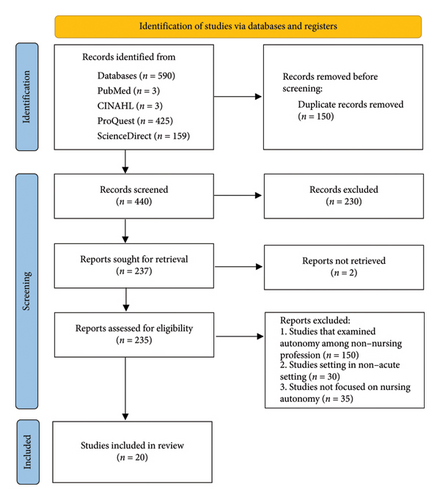
A comprehensive systematic search was conducted across four major databases: CINAHL, ScienceDirect, PubMed, and ProQuest. Advanced search techniques were employed using MeSH terms (Table A1), with assistance from a school librarian to refine the strategy. Following the PRISMA guidelines (Figure A1), articles were screened for eligibility based on predefined inclusion criteria. These included empirical studies (qualitative, quantitative, or mixed-methods) on autonomy in critical care nursing, conceptual papers and reviews discussing autonomy in nursing or critical care, English-language publications, studies from 2014 onward for contemporary relevance, and peer-reviewed journal articles, conference proceedings, and dissertations. Studies examining autonomy among other healthcare professionals (e.g., physicians and physical therapists) or in non–acute care settings, as well as research not focused on nursing practice autonomy, were excluded.
A total of 590 studies were identified through the selected databases. After removing 150 duplicates, 440 studies remained. An initial screening of titles and abstracts reduced this number to 237, which advanced to the second screening stage for a more detailed examination of their characteristics. Ultimately, 20 studies met the inclusion criteria for this analysis. Several articles were excluded due to their focus on autonomy among other healthcare professionals, their setting in non–acute care, or their lack of relevance to nursing practice autonomy. To appraise the included studies, the Johns Hopkins Evidence-Based Practice tool was used to evaluate methodological rigor and risk of bias. The included articles were ranked at Level III, ensuring that only high-quality studies were included in the final review.
3. Results
3.1. Identify All Uses of the Concept
The third step in Walker and Avant’s concept analysis involves identifying all the ways the chosen concept is used (Table A2). Within nursing theory, autonomy has become widely recognized through extensive study and practical application. In the literature, the terms independent decision-making and autonomy are often used interchangeably. Pursio et al. [2] define critical care nursing autonomy as the ability to make independent clinical decisions based on professional judgment while applying personal competence to patient care. In critical care setting, autonomy requires nurses to make patient-centered decisions without external directives, organize unit operations, and solve problems independently using their own value systems. Additionally, nurses must preserve their professional skills and maintain accountability for their actions.
Similarly, Ito et al. [14] describe ICU nurses’ autonomy as a trait that develops through clinical decision-making abilities and general professional independence, both of which are grounded in personal competence. Autonomy necessitates self-reliance and decision-making based on expertise while collaborating with team members to achieve optimal patient care outcomes. It is present when nurses can make decisions based on clinical judgment and knowledge that align with professional and ethical standards. According to AllahBakhshian et al. [15], the concept of autonomy enables nurses to trust their professional judgment to make independent clinical decisions without undue reliance on physicians.
Autonomy in critical care nursing primarily manifests through active involvement in decision-making processes and the ability to exercise personal influence over patient care decisions. The autonomy nurses experience is reflected in their ability to be heard and respected for their professional input in clinical environments where physicians and other healthcare team members value their contributions. The critical nature of ICU nursing necessitates autonomy, as nurses must make rapid decisions for complex patient care situations [16].
Deci and Ryan [18] define autonomy as a foundational element of self-determination theory (SDT), which analyzes health behavior by focusing on autonomy, competence, and relatedness. Their theoretical framework explores how the social environment functions as either a support system or an obstacle to individual autonomy. The SDT highlights how decision-making autonomy strengthens motivation and job satisfaction among critical care nurses, ultimately enhancing their well-being and fostering a positive work environment.
3.2. Determining and Defining Attributes
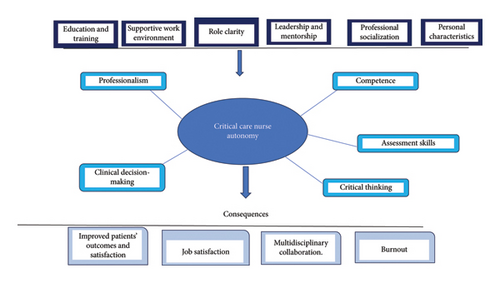
Several attributes associated with critical care nursing autonomy have been identified in the literature. These attributes include professionalism, competence, clinical decision-making, assessment skills, and critical thinking (Figure A2). These attributes are essential in fostering an environment where nurses can act independently and confidently. Understanding these characteristics helps in defining the scope of nursing autonomy within critical care settings. The recognition and development of these attributes can lead to improved patient outcomes and enhanced job satisfaction for nurses.
3.2.1. Professionalism
The American Association of Colleges of Nursing (AACN) [19] defines professionalism in nursing as the process of shaping a nursing identity that upholds values such as integrity, autonomy, altruism, inclusivity, compassion, courage, humility, advocacy, caring, humanity, and social justice. It is an ongoing journey of socialization, where nurses contribute to the profession by mentoring and fostering the growth of others. Ghadirian et al. [20] defined professionalism in nursing as a set of values crucial for enhancing the quality of patient care and refining the methods, standards, and judgments that guide nursing practice. Through advancements in education, work autonomy, and clinical experiences, the core values of the nursing profession can be further strengthened. The three essential quality categories of professionalism: cognition, attitude, and psychomotor. Cognition refers to continuously studying professional conduct and applying knowledge in the work environment. Critical care nurses who engage in career advancement develop vital skills to prioritize and make effective decisions in patient care. Attitude encompasses the behaviors and beliefs guiding nurses’ practice and career growth. Nurses’ behaviors should align with the standards of practice, and adaptability and negotiation skills are crucial in navigating professional challenges. Lastly, the psychomotor aspect of professionalism involves advancing professional experience and clinical skills.
3.2.2. Competence
Competence is an important attribute for an ICU nurse, encompassing a blend of clinical knowledge, technical skills, and the ability to apply them effectively in high-pressure, complex care environment. The ability of ICU nurses to provide excellent care for critically ill patients hinges on their competence since it affects both physical health and mental well-being outcomes. The multifaceted nature of competence in intensive and critical care nursing encompasses four key domains: knowledge, skill, attitude, and experience. The research reveals nurses with greater autonomy show higher basic competence (F value 60.85, β 0.11, SE 0.01, and p ≤ 0.0001). When nurses experience autonomy, it leads to both their professional advancement and improved implementation of evidence-based practices alongside ethical patient care principles. ICU nurse professional development depends heavily on field experiences which underscores the need for hands-on learning experiences in critical care education and orientation programs. Educational programs must develop clinical competence together with theoretical knowledge following national framework standards to ensure superior patient care results [21].
3.2.3. Clinical Decision-Making
Clinical decision-making is a cognitive process through which nurses can identify problems that may directly or indirectly impact their patients and take prompt actions to mitigate the worsening of these problems [22]. It involves enhancing cognitive abilities and intuition to quickly recognize issues related to patients and select appropriate interventions. Nurses in critical care settings often make quick, evidence-based decisions regarding patient care. This requires not only strong clinical knowledge but also the confidence to act based on their assessment of the patient’s condition. In the ICU, nurses are expected to analyze patient data and information to make clinical decisions that prevent further deterioration or complications. According to Yee [23], accurate clinical decision-making is an essential skill for ICU nurses due to the complexity and high acuity of the patient population. The clinical decision-making of ICU nurses is characterized by the prompt assessment of patients’ conditions, timely recognition of cues, and immediate response to clinical problems.
3.2.4. Assessment Skills
Physical assessment skills are essential for clinical decision-making and the early detection of patient decline, forming the foundation of ICU nursing practice. Rosli et al. [24] identify these skills as monitoring vital signs, conducting neurological assessments, evaluating respiratory function, and assessing cardiovascular stability. ICU nurses frequently make critical clinical judgment before consulting physicians or advanced practice providers (APPs) because they perform assessments independently. Their professional autonomy is demonstrated through the accurate interpretation of clinical data and timely interventions.
ICU nurses who pose proficient assessment skills can identify minor physiological changes which allows them to deliver interventions in time to stop further patient deterioration. Autonomy in ICU nursing improves patient safety while building stronger interdisciplinary teamwork because nurses need to communicate assessment results clearly and advocate for patients while coordinating with APPs and physicians to ensure optimal patient care. ICU nurses’ function under established protocols which grant them permission to perform interventions such as modifying oxygen therapy or giving emergency medications without a physician’s direct command. The effectiveness of these critical skills relies on continuous training and standardized assessment protocols which must be supported by institutional backing. When nurses develop better physical assessment skills, they gain greater autonomy which leads to better patient results in critical care environments.
3.2.5. Critical Thinking
Ghazivakili et al. [25] described critical thinking as integrating knowledge, performance, and attitude, enabling individuals to analyze and evaluate information through deductive and inductive reasoning. In critical care setting, critical thinking is essential for professional autonomy, as it allows nurses to apply safe, well-organized, and skillful interventions to address patients’ problems [26]. Critical care nurses must process, synthesize, and evaluate data obtained from patients’ observations, reflections, and experiences to develop sound clinical judgment [26]. According to Hayes et al. [27], diagnostic errors are the most common cause of medical malpractice claims and account for approximately 10% of in-hospital deaths. Many of these errors stem from deficiencies in critical thinking. Given the fast-paced and high-acuity nature of ICU environments, where medical errors can lead to severe consequences, fostering strong critical thinking skills is crucial in reducing adverse patient outcomes.
Critical thinking extends beyond cognitive and analytical skills to require recognition and challenge of assumptions, personal biases, and structural inequities. Critical care nurses need to understand the effects systemic racism and implicit bias have on healthcare delivery and patient outcomes. Through the integration of antioppressive practice within their critical thinking process nurses become advocates for justice and equality while delivering culturally sensitive care in high-pressure environments. Nurses must examine power dynamics while ensuring their care decisions remain clinically valid and ethically as well as socially responsible.
3.3. Presentation of Model Case Cases
The model case illustrates every attribute of critical care nurse autonomy as it functions in real-world scenarios [28].
Jessica, a highly skilled ICU nurse takes charge of a patient experiencing multiple-organ failure who requires critical care. The nurse performs hourly evaluations of patient status through advanced assessment techniques to track vital signs, lab outcomes, and clinical changes. During her discussions with the physician team, Jessica suggests possible treatment plans by considering the patient’s age background and present medical situation. She analyzes both the potential risks and benefits of the intervention through critical thinking before suggesting a specific treatment plan. Jessica communicates her recommendations with professionalism which ensures respect and confidence while following hospital protocols. Jessica demonstrates clinical expertise by making informed decisions based on evidence which leads to optimal patient outcomes. Her independence in patient care coordination with the multidisciplinary team demonstrates her autonomous work in the ICU.
3.4. Identifying Borderline, Related, and Contrary Cases
A borderline case partially demonstrates the attributes but may lack one or more essential elements or show a less complete embodiment of the concept. Related cases are examples that are connected to a concept but lack some of the specific attributes that define it, while a contrary case does not embody critical care nurse autonomy because it lacks essential attributes or demonstrates a lack of appropriate qualities [28].
3.4.1. Borderline Case
The critical care nurse Tina is responsible for a patient who is healing from major surgery. Tina exhibits professionalism and effective communication with patients and families but consistently seeks guidance from the attending physician during clinical decision-making instead of utilizing her own independent judgment. Her routine patient assessments prioritize standard tasks such as vital checks over comprehensive critical evaluation and detection of subtle signs of deterioration. Tina displays her nursing skills effectively yet fails to demonstrate leadership by making independent decisions or proposing different treatment options during rounds. The nurse shows professional competence but lacks clear independent decision-making abilities in the ICU.
3.4.2. Related Case
Sophie works as a critical care nurse in the ICU and she has been given responsibility for a patient who is healing from a significant traumatic injury. Sophie demonstrates professional interaction skills with patients and families which results in them feeling supported and knowledgeable about their care plan. Her routine nursing duties demonstrate competence as she administers medications and monitors vital signs. Sophie faces uncertainty about her next steps when she observes unexpected changes in the patient’s condition along with signs of decline. Sophie chooses to rely on the physician for guidance rather than applying her own critical thinking to assess the situation and explore potential interventions. She performs regular assessments yet fails to thoroughly investigate the slight changes that might show a problem. She adheres to established procedures and waits for the physician to decide while ignoring her own potential alternative recommendations based on her evaluations. Sophie shows professional ability and competence yet lacks visible evidence of strong critical thinking skills and decision-making ability which restricts her independence in the intensive care setting.
3.4.3. Contrary Case
As a newly hired ICU nurse Lydia finds it challenging to care for a critically ill patient who needs continuous monitoring and regular care adjustments. She doubts her clinical decision-making abilities and does not know when to work independently. Despite the patient requiring immediate medical intervention, Lydia delays making decisions until receiving physician orders when the patient’s health deteriorates. She fails to recognize minor signs of patient deterioration during assessments because she depends too much on colleagues to notice vital sign changes instead of using her critical thinking to predict potential complications. The absence of experience inhibits Lydia’s professional skills while her hesitation to make choices shows she lacks independent functioning in critical care situations.
3.5. Identifying Antecedents and Consequences
The seventh step in the Walker and Avant’s concept analysis is to determine the antecedents and consequences. Antecedents are the conditions or factors that must be present before a concept can occur, while Consequences refer to the outcomes that arise from the occurrence of a concept, aiding in the identification of ideas that may have been overlooked [29]. The conceptual map of critical care nurse autonomy is illustrated in Figure A2.
3.5.1. Antecedents
The antecedents of critical care nurse autonomy include education and training, supportive work environment, role clarity, leadership and mentorship, professional socialization, and personal characteristics.
3.5.1.1. Education and Training
Taleghani et al. [30] emphasized that education and training serve as fundamental antecedents to critical care nurse autonomy within the framework of a “powerful human workforce” while pinpointing knowledge and skill development as essential factors together with other personal characteristics such as education level. The combination of educational background and clinical experience establishes professional competence as essential for nurses to make independent clinical decisions in intensive care environments. Nurses who receive enhanced knowledge and training are better equipped to exercise their autonomy which leads to improved patient care and safety and shows that nurses’ technical skills combined with collaborative abilities with fellow healthcare professionals strengthen their autonomy and enable them to have a greater impact on patient outcomes.
3.5.1.2. Supportive Work Environment
Critical care nurse autonomy is shaped by the supportive nature of their work environment. According to Mabona et al. [31], leadership-supported professional independence creates environments that foster autonomy. Nurses should be allowed to make professional decisions according to their expertise and knowledge but they must also accept responsibility for those choices. Effective nurse leadership must create a workplace that promotes open communication while building trust and respect. Autonomy develops through cooperative teamwork efforts and leadership approaches that focus on empowerment and skill-building together with collegial support.
3.5.1.3. Role Clarity
The definition of nursing roles through precise job descriptions allows nurses to perform their tasks independently and authoritatively which helps them practice autonomous decision-making. The nurse must understand their position and specific duties within the multidisciplinary team for effective team functioning. Nurses who fully understand their professional scope and responsibilities tend to exhibit greater autonomy in healthcare settings. Clinical environments face role ambiguity and diminished autonomy along with increased frustration when nurses lack defined role descriptions. ICU nurses require role clarity to achieve necessary autonomy for effective decision-making which leads to improved patient outcomes [30].
3.5.1.4. Leadership and Mentorship
Leadership and mentorship emerge as foundational elements for nurse autonomy with special relevance in critical care settings. Clinical leadership skills function as a vital resource that enables nurses to achieve greater independence through empowerment. Clinical leaders fulfill key mentorship roles by coaching nurses as they learn critical thinking and reflective practice techniques. Through this leadership position nurses gain the confidence and competence required for their autonomous decision-making skills. Through mentorship nurses receive important knowledge and expertise which supports their ability to operate independently in clinical environments [32].
3.5.1.5. Professional Socialization
Professional socialization functions as a key element in building nursing identity and grasping professional values which together establish the foundation for nursing autonomy. The internalization of essential functions like advocacy, decision-making, and patient leadership by nurses leads to increase in their autonomy. The socialization practices within the nursing profession serve as a crucial element for developing professional autonomy among nurses. The relationship between nursing autonomy and professional socialization is inherently reciprocal: Nursing autonomy and professional socialization maintain a reciprocal relationship because the progression of nurses in their roles leads to independent practice abilities that develop through ongoing socialization. Through this process, nurses develop essential skills and clinical judgment alongside self-confidence which allows them to make decisions independently. When nurses obtain greater autonomy, their professional socialization strengthens which helps them to perform independent decision-making more effectively in their practice [5].
3.5.1.6. Personal Characteristics
Taleghani et al. [30] emphasized that nurses’ autonomy levels depend on their age and work experience. Less experienced younger nurses may not focus on autonomy but older nurses with more experience commonly demonstrate higher levels of autonomy. Critical care nurse autonomy develops from key personality traits which include courage, assertiveness, self-confidence, self-esteem along with stress management abilities. Nurses with these personality traits demonstrate greater work autonomy. Personal competencies such as professional skills along with work experience and individual professional attitudes determine the level of autonomy nurses achieve in ICU environments.
3.5.2. Identifying the Consequences
The consequences of autonomy among critical care nurses include improved patients’ outcomes, job satisfaction, and multidisciplinary collaboration.
3.5.2.1. Improved Patient’s Outcomes and Satisfaction
ICU nurses who exhibit autonomy demonstrate greater confidence and clinical decision-making skills which result in prompt interventions and improved patients’ outcomes for critically ill patients. Saeed et al. [33] reported that increased nurse autonomy allows nurses to fulfill patients’ expectations which result in enhanced outcomes. Early detection of changes in patients’ clinical conditions and prompt intervention promote improved outcome. Positive outcomes such as decrease in nosocomial infections, death rate, and ICU length of stay are associated with patients’ and family satisfactions. According to Yuk and Yu [34], critical care nurse autonomy serves as a crucial determinant affecting patient safety activities. Nurses with autonomy were more involved in patient safety activities. The results of multiple regression analysis showed professional autonomy (β = 0.234 and p = 0.001) as a variable with significant effects on patient safety activities.
3.5.2.2. Job Satisfaction
Professional organizations recognize autonomy as a fundamental component that consistently aligns with job satisfaction. Nursing workplace where autonomy is supported result in higher job satisfaction for nurses [35]. Critical care nurse autonomy is a key to achieving job satisfaction because it grants nurses the power to make independent clinical choices thereby building their professional confidence and stress management skills which enhances job satisfaction and improves nurse retention as well as patient care quality [36]. Job satisfaction contributes positively to job productivity, accountability, and critical thinking among nurses, thereby further enhancing the quality of care and patient outcomes.
3.5.2.3. Multidisciplinary Collaboration
ICU nurses who possess autonomy can take a proactive approach toward interacting with other healthcare team members. The result of this dynamic is enhanced teamwork in patient care along with better nurse collaboration and a unified team setting. Abu Hattab et al. [37] reported that critical care nurses achieve more autonomy through multidisciplinary collaboration between nurses and physicians. Critical care nurses perform better in their collaboration with physicians when they have autonomy. Enhanced clinical decision-making by nurses combined with power disparity reduction efforts lead to stronger critical care multidisciplinary team collaboration which results in improved healthcare outcomes.
3.5.2.4. Burnout
The literature indicates burnout as a harmful consequence of critical care nurse autonomy. Dall’Ora et al. [38] explained that critical care nurse autonomy leads to significant burnout when job demands are high and support systems are lacking. Nurses who experience autonomy without sufficient resources and recognition develop emotional exhaustion and depersonalization which leads them to feel less accomplished and these elements form the main aspects of burnout. When workplace autonomy lacks sufficient rewards and positive relationships along with sufficient decision-making power it results in employee burnout. Nurses experience negative effects on their well-being and patient care quality due to extended shifts and high work burdens compounded by poor leadership support.
3.6. Define Empirical Referents
The final step in Walker and Avant’s concept analysis framework [28] involves defining empirical referents. This phase illustrates how the attributes of a concept are operationalized and measured in real-world contexts. However, no prior study has comprehensively measured all the attributes of critical care nurse autonomy. Some of the quantitative studies reviewed, nonetheless, identified empirical referents for measuring select attributes of critical care nurse autonomy.
Lakanmaa et al. [21] utilized the Intensive and Critical Care Nursing Competence Scale version 1 (ICCN-CS-1) to assess and describe ICU nurses’ self-perceived basic competence and its related factors such as autonomy. The tool, based on a Likert scale ranging from 1 (poor) to 5 (excellent), was administered to a sample of 431 Finnish ICU nurses. The most significant factor influencing nurses’ perceived basic competence was their sense of autonomy in nursing care (F value 60.85, β 0.11, SE 0.01, p ≤ 0.0001). The reliability and validity of the ICCN-CS-1 were also evaluated. The scale is grounded in a comprehensive theoretical framework, and the internal consistency of the ICCN-CS-1 was found to be 0.99 in this study.
Rosli et al.’s [24] cross-sectional survey study analyzed how critical care nurses in Malaysia perform physical assessments and what factors affect their practice implementation. This study was conducted in a Malaysian government hospital involving 133 nurses from three critical care units who achieved a 96.4% response rate. The study collected data through a three-section self-administered survey.
The first part of the survey collected demographic information from participants. The second part assessed the frequency of 40 physical assessment skills used by nurses, which were based on previous studies and validated through a Delphi method. These skills covered multiple body systems, including vital signs, neurological, cardiovascular, respiratory, gastrointestinal, nutritional, urinary, integumentary, and musculoskeletal systems, and were measured using a six-point Likert scale. The third part included open-ended questions where nurses were asked about factors influencing their use of physical assessment skills and suggestions for improving performance. The study concluded that ICU nurses with stronger assessment skills tend to demonstrate greater autonomy in their roles. The survey instrument was validated through feedback from local experts, including senior nursing and medical lecturers, department heads, and nursing leaders, ensuring the study’s relevance and accuracy.
Ghazivakili et al. [25] conducted a descriptive-analytic, cross-sectional study to examine the relationship between critical thinking, learning styles, and students’ academic performance. Critical thinking was measured using the California Critical Thinking Skills Test (Form B), which consists of 34 multiple-choice questions across five critical thinking areas: evaluation, inference, analysis, inductive reasoning, and deductive reasoning. The researchers assessed the reliability and validity of the tool based on previous studies, which reported a reliability coefficient of 62% and strong construct validity for all subscales, with positive correlations ranging from 60% to 65%.
4. Discussion
Critical care nurses need full autonomy to improve patient outcomes and increase job satisfaction and teamwork across disciplines. The analysis shows that ICU nurses depend on clinical decision-making skills, professionalism, competence, and critical thinking to make autonomous and responsible patient care decisions. Autonomy in critical care is the ability to act swiftly and decisively in fast-paced environments. Education and training, a supportive workplace, and clear role definition and leadership are fundamental antecedents that promote autonomy. Professional growth and strong leadership support establish a setting where nurses can independently execute patient-focused decisions through autonomy.
Autonomy improves patient outcomes because nurses who make independent decisions can respond quickly and improve patient care. Increased job satisfaction derived from autonomy leads to lower turnover rates and decreases burnout among nurses. Autonomy without adequate support systems causes burnout among nurses, which shows that healthcare organizations need to establish balanced support structures. Understanding autonomy should extend beyond individual perspectives by integrating relational autonomy, especially in critical care nursing situations. Relational autonomy argues that autonomous decision-making emerges from social and cultural relationships and professional networks instead of being purely an individual choice. The relational autonomy perspective recognizes that nurse’s function within interlinked care systems, which shape their independent actions through team dynamics, institutional power structures, and cultural guidelines. A relational model promotes teamwork while fostering mutual respect and shared responsibilities in interdisciplinary groups. This approach matches decolonial and antioppressive practices because it acknowledges that historical and structural inequalities limit autonomy for both patients and nurses.
Additionally, while autonomy enables critical care nurses to exercise independent judgment, it must be balanced with the equally important autonomy of patients and families. In high-stakes ICU settings shared decision-making becomes essential because professional assessments often conflict with patient or surrogate preferences. Patient-centered care requires professional autonomy to function within a system that honors the rights and voices of care recipients. Evaluating the roles of clinical decision-making, competence, and critical thinking shows how autonomy influences individual nurses and the broader healthcare team. However, accountability in this context must extend beyond adherence to professional codes and institutional policies. It should also reflect a moral commitment to patients and families and broader values of equity, justice, and inclusion in healthcare. Balancing professional autonomy with these ethical obligations strengthens the nurse’s role as an expert and an advocate within the multidisciplinary team.
The concept of critical care nurse autonomy is multifaceted and warrants further exploration. Many studies examined in the concept analysis have assessed various attributes of critical care autonomy. However, to understand what autonomy truly means for ICU nurses, further research is needed that explicitly explores ICU nurses’ perspectives on professional autonomy. It is essential to clearly define and measure all the attributes of professional autonomy within the critical care nursing context. Findings from such studies could inform policy changes that promote the advancement of the nursing profession. The absence of nursing representation on the national COVID-19 task force highlighted the marginalization of the nursing profession despite nursing being one of the most significant and integral components of the healthcare team. This exclusion underscores the impact of limited autonomy, which is often associated with a lack of involvement in healthcare policy decisions. It is crucial to engage nurses in defining what autonomy means to them and identify strategies to ensure their active participation in multidisciplinary healthcare teams at local, state, and national levels.
5. Implications for Practice
This concept analysis of autonomy in critical care nursing reveals important outcomes that affect clinical practice, organizational policies, educational standards, and leadership roles within healthcare environments. Understanding autonomy as an essential component of critical care nursing practice highlights the importance of developing environments that enable nurses to apply independent clinical judgment confidently and effectively.
5.1. Enhancing Clinical Practice
ICU nurses can make informed decisions quickly when they are supported to exercise autonomy, which proves vital for effective intensive care operations. Healthcare institutions must set standard protocols that give nurses more freedom to assess and treat patients, enhancing patient safety and outcomes. Create hands-on training, simulation-based learning opportunities, and continuing education to develop clinical decision-making competence and physical assessment skills.
5.2. Organizational Support and Policy Development
Hospital administrators and nurse leaders must establish organizational values centered around trust, teamwork, and professional respect. Detailing job descriptions and explicit practice scopes are essential elements for diminishing role ambiguity while increasing professional autonomy. Leadership that focuses on empowerment and mentorship helps build autonomy and reduces burnout while improving nurse retention rates. Quality improvement processes and professional development objectives must integrate metrics evaluating autonomy.
5.3. Leadership and Mentorship Strategies
Leaders and mentors have a crucial influence on developing and maintaining autonomy for critical care nurses. Novice nurses who participate in structured mentorship programs develop confidence, critical thinking skills, and independent practice abilities. Experienced nurses require training in coaching and reflective practice through leadership development initiatives to demonstrate autonomous behavior and promote team professional advancement.
5.4. Education and Professional Socialization
Critical care training in nursing education programs must emphasize critical thinking, ethical reasoning, and leadership education as essential elements. Curricula development should include opportunities for interprofessional collaboration and exposure to complex clinical scenarios to prepare nurses for autonomous practice. Through professional socialization focusing on advocacy and patient-centered care, nurses learn decision-making skills that enable them to function autonomously.
5.5. Policy Advocacy and Representation
Critical care nurses’ active participation in healthcare policy-making processes is essential to incorporating their perspectives in decisions that influence clinical settings. Institutional, state, and national advocacy should work to remove structural obstacles to nursing autonomy while promoting leadership roles for nurses in interdisciplinary healthcare teams.
Disclosure
We appreciate the opportunity to submit our manuscript, “Analyzing Autonomy in Critical Care Nursing: Unveiling the Distinctive Aspects,” to the Nursing Forum Journal. We affirm that we have met the submission requirements. In this paper, we have analyzed and unveiled the distinctive aspect of autonomy among critical care nurses. We provided a conceptual definition to enhance understanding of autonomy within this context.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Appendix A
| Concept | MeSH terms |
|---|---|
| Autonomy | “Autonomy” AND “nurses” AND “conceptual framework” AND “critical care” |
| “Nurses’ perspectives” AND “autonomy” AND “critical care practice” | |
| “Autonomy in critical care” AND “nursing practice” AND “defining attributes” |
| Author/year/country | Discipline | Definition |
|---|---|---|
| Pursio et al. [2] (2021) Finland | Nursing | Critical care nursing autonomy as making independent clinical decisions based on professional judgment while applying personal competence to patient care |
| Ito et al. [14] (2024) Japan | Nursing | ICU nurses’ autonomy as a trait that develops through clinical decision-making abilities and general professional independence based on personal competence |
| AllahBakhshian et al. [15] (2017) Iran | Nursing | Critical care nursing autonomy exists when nurses can make decisions based on their clinical judgment and knowledge that supports the complete range of nursing practice as defined by professional and ethical standards |
| Randall [16] (2020) United States of America | Nursing | Critical care autonomy is defined as an active involvement in decision-making processes and possessing the power to exercise personal influence over patient care decisions |
| Nightengale College [17] (2021) United States of America | Nursing | Nursing autonomy is defined as the ability of nurses to conduct patient assessment and apply nursing treatments based on their knowledge and professional abilities |
Open Research
Data Availability Statement
Qualified researchers can request the study data from the corresponding author Frances Okpaluba at [email protected]. Privacy and ethical regulations prevent public access to the data. Qualified researchers may request the relevant data used in the concept analysis which contains systematic search results along with study inclusion criteria and analytical framework.




