A Comparative Study of the HbA1c Level in Prediabetic Patients With Lifestyle Modification Versus Oral Hypoglycemic Agents
Abstract
Background: Lifestyle modifications are the cornerstone of prediabetes management, aiming to prevent or delay progression to diabetes. In addition to lifestyle interventions, pharmacologic treatment with oral hypoglycemic agents (OHAs), particularly metformin, is frequently considered.
Objectives: The objective of this study was to identify optimal strategies for the management of prediabetes in low- and middle-income countries (LMICs) like Nepal.
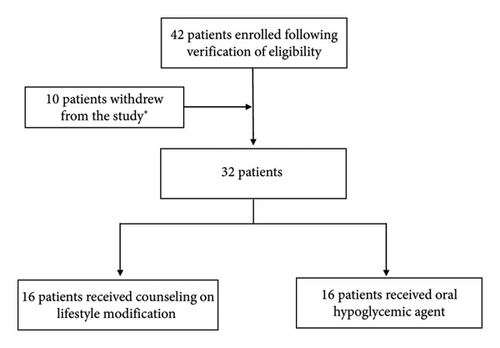
Methods: A comparative experimental study was conducted to assess the effects of lifestyle modification and treatment with OHA separately in prediabetic patients (16 per group). The lifestyle modification group (Group A) received structured counseling on dietary modifications and physical activity, and the OHA group (Group B) was prescribed metformin. Baseline parameters were recorded for all participants, and blood pressure and HbA1c levels were reassessed at 90 days to determine changes from the baseline.
Results: Significant reduction in HbA1c was observed for both the OHA group (p = 0.0034) and the lifestyle modification group (p < 0.001). The lifestyle modification group achieved significantly greater reductions in HbA1c compared with the OHA group (p = 0.0002).
Conclusions: Lifestyle modification and pharmacological therapy with metformin can lead to a significant decrease in HbA1c levels in the prediabetic population as a sole intervention. Lifestyle modification resulting in greater reduction could be a sustainable and cost-effective alternative, particularly in LMICs like Nepal.
1. Background
Diabetes mellitus is a chronic metabolic disorder characterized by persistent hyperglycemia resulting from defects in insulin secretion, insulin action, or both [1]. The global prevalence of diabetes is increasing, with approximately 830 million individuals affected, the majority residing in low- and middle-income countries (LMICs). The most common forms of diabetes include type 1 diabetes (insulin dependent), type 2 diabetes (insulin independent), and gestational diabetes [2].
Prediabetes is an intermediate metabolic state in which blood glucose levels are elevated above the normal range but remain below the diagnostic threshold for diabetes. It includes impaired fasting glucose (fasting plasma glucose: 100–125 mg/dL), impaired glucose tolerance (two-hour postchallenge plasma glucose: 140–199 mg/dL), and an elevated glycated hemoglobin (HbA1c) level of 5.7%–6.4% [3]. Prediabetes is a significant risk factor for type 2 diabetes, with approximately 10% of affected individuals progressing to diabetes annually [4]. In Nepal, the prevalence of prediabetes is rising, while awareness and preventive measures remain suboptimal [5].
Lifestyle modifications are the cornerstone of prediabetes management, aiming to prevent or delay progression to diabetes. Weight reduction, particularly in overweight or obese individuals, has been shown to be highly effective. The American Diabetes Association (ADA) recommends a combination of aerobic exercise and muscle-strengthening activities to enhance glycemic control. Dietary modifications, including carbohydrate regulation, balanced protein and fat intake, and limiting alcohol and sweeteners, further contribute to risk reduction [6]. In addition to lifestyle interventions, pharmacologic treatment with oral hypoglycemic agents (OHAs), particularly metformin, is frequently considered. Metformin, a biguanide-class medication, functions as an insulin sensitizer by reducing hepatic glucose production and improving peripheral glucose uptake [7].
Globally, various studies have explored perspectives on prediabetes education interventions among different stakeholders, including individuals with prediabetes, examining their experiences with dietary and physical activity modifications following diagnosis and participation in lifestyle intervention programs [8–10]. However, most of these studies have been conducted in high-income countries. Therefore, this study aims to identify optimal strategies for the management of prediabetes in LMICs such as Nepal.
2. Methods
It was a comparative experimental study conducted to assess the effects of lifestyle modification and treatment with OHA separately in prediabetic patients. The study was conducted at Shree Birendra Hospital, Kathmandu, Nepal. Participants were recruited from the general outpatient department (OPD) and emergency department over a 6-month period from 20 October 2023 to 19 April 2024. Data were collected using a structured proforma after obtaining written and verbal consent from the patients. The study was conducted in accordance with ethical guidelines and was approved by the Nepalese Army Institute of Health Sciences-Institutional Review Committee (NAIHS-IRC) with registered number 877.
Eligible participants included individuals with HbA1c levels between 5.7% and 6.4%, classified as prediabetic. Patients were excluded from the study if they were admitted to the hospital due to multiple comorbidities, required dialysis, had a diagnosed psychiatric illness, and were undergoing chemotherapy.
-
Group A (lifestyle modification group): Participants received structured counseling on dietary modifications and physical activity. Adherence was monitored through regular phone calls, with compliance reassessed at bimonthly follow-ups.
-
Group B (OHA group): Participants were prescribed metformin as a pharmacological intervention for prediabetes. Adherence was assessed by reviewing returned medication strips.
Baseline parameters were recorded for all participants, including weight, blood pressure, complete blood count (CBC), urine routine examination (R/E), liver function test (LFT), renal function test (RFT), lipid profile, fasting blood glucose, postprandial blood glucose, and glycated hemoglobin (HbA1c). Additionally, demographic data and comorbidities such as hypertension, chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), and other relevant conditions were documented along with concomitant medications. Follow-up assessments were conducted every month, during which compliance, adverse effects, and symptom resolution were evaluated through physical examinations and verbal inquiry. Blood pressure and HbA1c levels were reassessed at 90 days to determine changes from baseline.
Data were analyzed using Statistical Package for Social Sciences (SPSS) Version 16. Descriptive statistics, including frequencies and percentages, were calculated for categorical variables. The normality of continuous variables was assessed using the Shapiro–Wilk test. Given the potential for non-normal data distribution, the Wilcoxon signed-rank test was applied to evaluate changes in variables over time. Comparisons were made against baseline values within each group. A p value of < 0.05 was considered statistically significant.
3. Results
A total of 32 participants were enrolled in the study and were randomly assigned into two equal groups. Group A (n = 16) received lifestyle modification counseling, while Group B (n = 16) was prescribed metformin. Group A comprised 11 males (68.75%) and 5 females (31.25%), whereas Group B included 13 males (81.25%) and 3 females (18.75%). In terms of age distribution, 7 participants (43.75%) in Group A and 9 participants (56.25%) in Group B were aged 60 years and above. In addition, 7 participants (43.75%) from each group fell within the 40–59 years age category. The majority of study participants resided in urban areas, with 12 individuals (75%) in Group A and 11 individuals (68.75%) in Group B. Conversely, rural participants comprised 4 individuals (25%) in Group A and 5 individuals (31.25%) in Group B. Regarding concomitant comorbidities, a higher proportion of participants in Group B were free of comorbid conditions compared with Group A (12 [75%] vs. 9 [56.25%]). In Group A, 2 participants (12.50%) had hypothyroidism, 3 (18.75%) had hypertension, and heart disease and kidney disease were each diagnosed in different participants. In Group B, hypothyroidism, hypertension, heart disease, and kidney disease were each diagnosed in different participants. None of the participants met the WHO criteria for obesity. However, 6 participants (37.50%) in Group A and 4 participants (25%) in Group B were classified as overweight (preobese, BMI: 25.0–29.9 kg/m2). The majority of participants had a normal BMI (18.5–24.9 kg/m2), including 10 individuals (62.50%) in Group A and 12 individuals (75%) in Group B (Table 1).
| Variables | Particulars | Group | Total | |
|---|---|---|---|---|
| OHA (metformin) treated | Lifestyle modification | |||
| Sex | Male | 13 (81.25%) | 11 (68.75%) | 24 (75.00%) |
| Female | 3 (18.75%) | 5 (31.25%) | 8 (25.00%) | |
| Age (years) | Below 40 | 0 (0.00%) | 2 (12.50%) | 2 (6.25%) |
| 40–59 | 7 (43.75%) | 7 (43.75%) | 14 (43.75%) | |
| 60 and above | 9 (56.25%) | 7 (43.75%) | 16 (50.00%) | |
| BMI | Normal | 12 (75.00%) | 10 (62.50%) | 22 (68.75%) |
| Overweight | 4 (25.00%) | 6 (37.50%) | 10 (31.25%) | |
| Obese | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| Comorbidities | None | 12 (75.00%) | 9 (56.25%) | 21 (65.62%) |
| Hypothyroidism | 1 (6.25%) | 2 (12.50%) | 3 (9.38%) | |
| Hypertension | 1 (6.25%) | 3 (18.75%) | 4 (12.50%) | |
| Heart disease | 1 (6.25%) | 1 (6.25%) | 2 (6.25%) | |
| Kidney disease | 1 (6.25%) | 1 (6.25%) | 2 (6.25%) | |
| Location | Urban | 11 (68.75%) | 12 (75.00%) | 23 (71.88%) |
| Rural | 5 (31.25%) | 4 (25.00%) | 9 (28.12%) | |
| Total | 16 | 16 | 32 | |
- Abbreviations: BMI, body mass index; OHA, oral hypoglycemic agent.
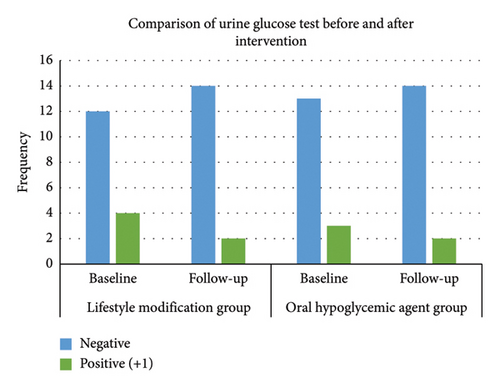
The distribution of urine glucose dipstick test in both groups at the baseline and follow-up is depicted in Figure 2.
Baseline blood test results in Group A demonstrated a mean fasting blood glucose level of 121.33 ± 3.72 mg/dL, postprandial blood glucose of 166.66 ± 14.05 mg/dL, and HbA1c of 6.06 ± 0.23%. In Group B, the mean fasting blood glucose was 119.56 ± 4.09 mg/dL, postprandial blood glucose was 165.79 ± 15.17 mg/dL, and HbA1c was 6.04 ± 0.2%. At the 90 days follow-up, the mean HbA1c was 5.76 ± 0.25% in Group A and 5.96 ± 0.15% in Group B (Figure 3).
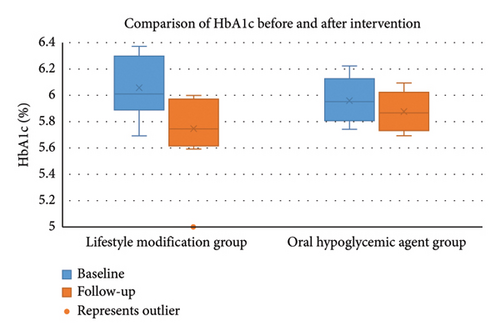
Both interventions demonstrated statistically significant reductions in HbA1c levels from the baseline to follow-up. The OHA group exhibited a mean reduction of 0.076 units (p = 0.0037), while the lifestyle modification group achieved a substantially larger mean reduction of 0.301 units (p < 0.001). Normality testing indicated that change scores for the lifestyle modification group violated normal distribution assumptions (p = 0.0066). To address this, nonparametric analyses were conducted. The Wilcoxon signed-rank test confirmed significant reductions in HbA1c for both the OHA group (p = 0.0034) and the lifestyle modification group (p < 0.001). The Mann–Whitney U test further confirmed that the lifestyle modification group achieved significantly greater reductions in HbA1c compared with the OHA group (p = 0.0002).
Effect size analysis revealed a small-to-moderate effect for OHA (Cohen’s d = 0.425) and a large effect for lifestyle modification (Cohen’s d = 1.249) groups, with a very large between-group difference (Cohen’s d = 1.446). A statistical power analysis was conducted to assess the adequacy of the sample size (n = 32). Despite the small sample size, the study achieved excellent power (1.0) due to the large observed effect size (Cohen’s d = 1.446). For an effect of this magnitude, only 6 participants per group would have been required to achieve 80% power. However, for smaller effect sizes, the current sample size would be underpowered, highlighting the need for caution when generalizing these findings or detecting more modest effects.
4. Discussion
This study demonstrated a significant change in HbA1c levels within 90 days in the study group counseled for lifestyle modification as well as the group under pharmacotherapy with metformin. However, the group counseled for lifestyle modification resulted in a significantly greater reduction. These findings are in conformity with the findings of similar studies conducted worldwide. A randomized control trial conducted by O’Brien et al., published in the American Journal of Preventive Medicine, demonstrated marginal improvement in HbA1c levels in prediabetic patients with intensive lifestyle intervention as compared with prediabetic patients receiving metformin and standard care [11].
Similarly, a study by Basavareddy et al. published in the Journal of Diabetology proves that lifestyle modification alone was equivalent to lifestyle modification with metformin in effective control of blood sugar [12]. The Indian Diabetes Prevention Program concluded that both lifestyle modification and metformin significantly reduced the incidence of type 2 diabetes in prediabetic Asian Indians and that there was no added benefit from combining the two interventions [13]. The study published by Ramachandran et al. also claims that progression from prediabetes to full-blown diabetes is high in native Asian Indians [13]. This study is of great value in the case of the Nepalese population due to the close proximity between the Indian and Nepalese populations and shared traits between the people, both genetic and environmental.
Likewise, a clinical trial conducted by Knowler et al. has claimed that both lifestyle modification and metformin reduced the incidence of type 2 diabetes in high-risk individuals. However, lifestyle intervention seemed to be a more effective option as compared with metformin treatment [4]. A review published by Echouffo-Tcheugui et al. also shows that both lifestyle modification and metformin treatment are effective in preventing full-blown diabetes mellitus in prediabetics; however, lifestyle modification, such as weight loss and exercise, is associated with larger benefits than metformin [14].
There are contrasting reports in relation to the larger benefits of lifestyle modification as compared with metformin treatment. A meta-analysis published by Mousavi et al. shows that lifestyle modification can be more efficacious than metformin in reducing the incidence of type 2 diabetes mellitus [15]. However, another meta-analysis by Vajje et al. has concluded that the incidence of type 2 diabetes being slightly higher in patients receiving metformin alone as compared with lifestyle intervention was not statistically significant [16].
This study was conducted in a single tertiary care hospital with a limited number of patients (n = 32) in a limited time frame (90 days). The study could potentially possess response bias as the participants may inaccurately report adherence to lifestyle modifications or medication regimens, potentially affecting the reliability of findings. Selection bias could be encountered as the sample may not be fully representative of the prediabetic population at Shree Birendra Hospital, limiting the generalizability of the results. The effects of different medications, comorbidities, age, and sex were not assessed, which might have an impact on HbA1c levels over time. Our study did not explore the dose relation of exercise and reduction in HbA1c levels in the study population. This study might not reflect the scenario of the general LMIC population in its entirety. Although the study aimed to compare two approaches to managing prediabetes, differences in the statistical distribution of data prevented a direct comparison.
5. Conclusion
The findings of this study suggest that both lifestyle modification and pharmacological therapy with metformin can lead to a significant decrease in HbA1c levels in the prediabetic population. Lifestyle modification, which resulted in greater reduction, could be a sustainable and cost-effective alternative, particularly in settings like LMICs such as Nepal. It has the potential to promote behavioral changes in the general population, encouraging the adoption of healthier lifestyles to combat the rising prevalence of noncommunicable diseases like diabetes.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
No funding was received for this manuscript.
Open Research
Data Availability Statement
Data available on request due to privacy/ethical restriction.




