Cardiovascular Disease Management and Prevention in Saudi Arabia: Strategies, Risk Factors, and Targeted Interventions
Abstract
Cardiovascular diseases (CVDs) remain the main cause of mortality and are generally among the leading causes of morbidity worldwide, thus placing an immense burden on health care. They include coronary artery disease, heart failure, hypertensive heart disease, and stroke. Among these, common risk factors include hypertension, high cholesterol, diabetes, smoking, obesity, and sedentary lifestyle. Yet, with advancements in medical science and pharmacology, these entities remain major challenges to public health worldwide. In Saudi Arabia, the rise in CVDs has been intensified by rapid urbanization and lifestyle changes and needs unique and tailored public health strategies. This review provides a comprehensive overview of the current situation with regard to cardiovascular health in Saudi Arabia, underlining the need for studying CVDs within the local context. It reviews the epidemiology of CVDs in the Kingdom of Saudi Arabia, outlining some of the major risk factors and also their impact on public health. This study also deals with the pharmacological approaches toward cardiovascular health by offering data from clinical trials so far completed, to point out effective strategies of treatment. The overview of prevention methods also includes public health initiatives, lifestyle programs, patient education, healthcare policies, the role of government initiatives, insurance coverage, and international collaborations. The review also elucidates the problems and barriers of the Saudi healthcare system, especially vis-à-vis the primary healthcare setting. In light of improving its healthcare sector, Saudi Arabia has embarked on several reforms within the Universal Health Coverage development initiative set in the framework of Vision 2030.
1. Introduction
1.1. Background on Cardiovascular Health Globally and in Saudi Arabia
Cardiovascular diseases (CVDs) represent the main cause of mortality and morbidity worldwide; millions are suffering, which places a gross strain on health care. They range from coronary artery disease, heart failure, hypertensive heart disease, and stroke, all having common risk factors. The major modifiable reservoirs of risk for the development and progression of CVDs include hypertension, high cholesterol, diabetes, smoking, obesity, and sedentary lifestyle. Although medical science, particularly pharmacology, has offered immense strides in the management and prognosis of these diseases, they still create immense burdens globally [1]. CVD is an important public health challenge that perturbs Saudi Arabia and is further aggravated by rapid urbanization and large shifts in lifestyle. The prevalence of risk factors such as diabetes, obesity, and smoking has dramatically increased, reflecting a global trend with regional specificities that call for unique approaches. Demographic and epidemiological peculiarities in the Saudi population, genetic predispositions, and cultural practices all influence the extent and expression of CVDs in this population. Variables like these underscore the need for individually tailored public health strategies and interventions. This alone presents the challenge of dual healthcare infrastructure in Saudi Arabia: dealing with CVD and taking preventive measures to curb their incidences in the future. It is important to know how this interplay of these two local factors functions to develop an interventional health approach and policies that would be more effective [2].
1.2. Importance of Studying CVDs in Saudi Arabia
It is important to undertake research on CVDs in Saudi Arabia for a variety of reasons. First is the high prevalence of risk factors for diabetes and obesity, diseases that are exploding disproportionately in the Gulf region, which requires specific research into their effects on cardiovascular health. At the same time, Saudi Arabia is undergoing huge socioeconomic changes affecting health behaviors and access to health care. The understanding of these dynamics becomes critical for the design of effective intervention strategies. Finally, the known genetic and cultural factors in the Saudi population may well influence preconditions and progressions of CVDs, demanding region-specific studies [3]. It also places a considerable economic burden on the Saudi healthcare system in terms of direct and indirect costs for treatment, hospitalization, and productivity loss. An effective reduction in CVDs would lead to a substantial decrease in healthcare expenditure and a dramatic improvement in the quality of life of subjects. Finally, Saudi Arabia’s commitment under Vision 2030 to increase health care and healthy living further underlines the need for focused research and law reform action toward having an effective and winning strategy for health care against CVD [4].
1.3. Objectives: Analyze Risk Factors and Explore Pharmacological Preventive Strategies
This study has two main objectives: first, to critically review the main risk factors responsible for the high incidence of CVD in Saudi Arabia; second, to investigate pharmacological preventive strategies fitting special needs among the Saudi population. In particular, the objectives are as follows.
1.3.1. Detailed Risk Factor Analysis
Epidemiological Review: This would involve conducting a critical review of epidemiology regarding CVDs in Saudi Arabia, with a view to dwelling on the prevalence and major risk factor distributions for hypertension, diabetes mellitus, dyslipidemia, smoking, obesity, and sedentary lifestyle.
1.3.1.1. Sociocultural Factors
The contributions of socioeconomic conditions, cultural practices, dietary habits, and genetic predisposition to the risk of developing atherosclerotic cardiovascular disease (ACVD) in the Saudi population are determined.
1.3.1.2. Trends and Patterns
Recent trends and patterns in morbidity and mortality from CVD, including age, sex, and regional trends and variations within Saudi Arabia, are outlined and analyzed.
1.3.2. Evaluating the Pharmacological Preventive Strategies
Pharmacotherapies Currently in Use: The efficiency and safety of the drugs in use for the prevention of CVD will be reviewed and estimated, taking into account the antihypertensive agents, statins, antiplatelet drugs, and newly emerging novel therapies against CVD.
1.3.2.1. Personalized Medicine
The role of PM and pharmacogenomics in improving CVD prevention and management is examined. The role of genetic profiling in the development of personalized curative measures for improving therapeutic outcomes is explored.
1.3.2.2. Comparative Analysis
The effectiveness of the various pharmacological strategies adopted in Saudi Arabia is compared to those used elsewhere in regions with similar epidemiological characteristics, highlighting best practices and areas that could be adapted and improved.
1.3.2.3. Integrate Into Public Health Policy
Lastly, evidence-based recommendations to include effective pharmacological preventive strategies in national public health policy and clinical guidelines for Saudi Arabia are proposed. The importance of accessibility, affordability, and adherence to treatment regimens is emphasized.
In summary, this paper should contribute to scientific knowledge concerning cardiovascular health in Saudi Arabia and aid in developing effective, targeted strategies to reduce the burden of CVDs. This would allow for appropriate formulation of public health interventions and clinical practices for the Saudi situation, improving cardiovascular outcomes in the region.
2. Epidemiology of CVDs in Saudi Arabia
2.1. Incidence, Prevalence, and Demographic Distribution
With their rates of incidence and prevalence increasing at an alarming rate over the last few decades, CVDs now account for a high percentage of various diseases in Saudi Arabia. The overall prevalence of CVDs, including coronary artery disease, hypertension, and heart failure, was very high. According to studies, nearly one-quarter of the adult population may be affected by some kind of cardiovascular condition [5]. Acute coronary syndrome and myocardial infarction have also increased, reflecting the increasing burden of atherosclerotic diseases (ADs). Hypertension, sometimes referred to as a silent killer, is indeed very prevalent, as a significant percentage of the adult population is diagnosed to have high blood pressure, many of which oftentimes progress to complications such as stroke and heart failure. By the same token, the prevalence of hyperlipidemia, which is another critical risk factor for coronary artery disease, also increases, further compounding this burden of CVDs [6]. The demographic distribution of CVDs in Saudi Arabia shows some interesting trends. It is highest in middle-aged and elderly individuals, but worryingly enough, there is also a trend of appearance of CVDs in more youthful age groups, likely as a result of lifestyle change characteristics such as bad eating habits, sedentary lifestyle, and stress. Gender-wise, the difference is striking, as it is usually observed that CVDs are more common in men compared to women; however, the cardiovascular danger does surge considerably in postmenopausal women [7]. There are geographical differences in the distribution of CVDs within Saudi Arabia. Cities have higher rates of CVD compared to rural regions due to increased pollution, sedentary lifestyles, and changes in dietary patterns. However, rural areas are not far behind as the effects of adopting an urban lifestyle and diet spread. In addition, morbidity and mortality are noticed more in certain areas that have low accessibility to health services due to late diagnosis and poor treatment [8]. The demographic distribution of CVDs in Saudi Arabia is also critical with respect to interplaying genetic factors. Familial hypercholesterolemia (FH) and other genetic predispositions to cardiovascular conditions are relatively common, underpinning cases of very early-onset CVDs in several individuals. It is these genetic factors that, along with those induced by environmental and lifestyle factors, cumulatively contribute to a complex epidemiological landscape; this demands specially aimed intervention strategies to nail down the biggest “moveable feast” contributors [7].
2.2. Comparison With Global Trends
Comparing the epidemiology of CVDs in Saudi Arabia to global trends reflects several similarities and distinctions. Nevertheless, at a worldwide level, CVD remains one of the leading causes of death and disability. In industrialized countries, mortality rates from CVDs are now decreasing due to improved health care, early diagnosis, and proper control measures being instituted [9]. In contrast, Saudi Arabia, as in other developing and middle-income countries, is experiencing a rapid rise in the burden of CVD resulting from intense urbanization, lifestyle changes, and increases in cardiovascular risk factors such as diabetes, obesity, and hypertension [2]. Table 1 shows a comparative analysis based on epidemiological data and risk factors with nearby countries. The nation has some of the world’s highest prevalence rates for hypertension, diabetes, and hyperlipidemia, with markedly higher than average global diabetes prevalence, thereby greatly multiplying the risks for CVD. The factors confer lifestyle-related aspects, especially high-calorie diets and cigarette smoking, and physical inactivity is sharp due to high economic growth rates and cultural changes [16]. The traditional diet, characterized by saturated fats and excessive sugar intake, together with low activity of sedentary lifestyles, contributes a great way to high morbidity from CVDs. However, smoking remains prevalent among men, further increasing the risks of CVDs. Although CVD predominantly affects older adults worldwide, the trend in Saudi Arabia indicates increased prevalence in the younger population due to high obesity and diabetes rates attributable to the prevailing sedentary lifestyle [17]. Access to health care, however, remains a problem in certain parts, especially the rural areas of Saudi Arabia, leading to delayed diagnosis and increased mortality. Despite the massive investments made in the infrastructure for health care, inequities in the delivery of care exist [18]. As such, concentrated efforts are needed to enhance accessibility and quality of care. Education and policy interventions at the community level have decreased the incidence of CVD in many parts of the world through public health measures. Another country undergoing similar attempts but at a slower rate of influence is Saudi Arabia, due to sociocultural factors and variable public awareness. This includes efforts through Vision 2030 for healthier lifestyles and the improvement of health service quality within the country. This corroborates the global agenda on many of the risk factors and challenges for CVDs faced by Saudi Arabia, although it experiences many unique quips of local epidemiological and sociocultural features that raise disease liability [19]. Such challenges must be addressed with individual public health strategies tailored to meet Saudi population needs, while learning from successful global interventions.
| Country | Key metrics | Risk factors | Projections | References |
|---|---|---|---|---|
| Saudi Arabia | - 45% of all deaths attributed to CVD | Rising obesity, diabetes (25% prevalence), hypertension (34%), and sedentary lifestyle (86%) | 201,300 CVD cases (2016) expected to rise with aging population and risk factors | [4] |
| - 26% 10-year heart attack risk in adults (2015 study) | ||||
| - $9.8B projected CVD economic burden by 2035 | ||||
| Egypt | - 32.4% of deaths from CAD (WHO 2017) | Metabolic syndrome, psychosocial stress, and poor dietary habits | Leading cause of death with worsening trends due to unmanaged risk factors | [10] |
| - 359.3 age-standardized CVD deaths/100,000 (2019) | ||||
| Kuwait | - 41% of deaths from CVD | Extreme heat exposure | Heat-resilient healthcare infrastructure | [11, 12] |
| - $5.2B economic loss (3.9% of GDP) | High smoking rates | Climate adaptation policies | ||
| - 20,569 heat-attributable CVD cases (2010–2019) | Urban sedentary lifestyles | |||
| Turkey | - 3.4M CVD cases (2016) rising to 5.4M by 2035 | Urbanization, hypertension (25%), and obesity (27%) | Demographic aging driving 59% case increase (2016–2035) | [13] |
| - $19.4 B projected economic burden by 2035 | ||||
| Oman | - 338.9 ACS cases/100,000 person-years | Hypertension (71% of CVD cases), diabetes, and dyslipidemia | Long waiting lists for cardiac interventions due to limited specialized centers | [14] |
| - 21.5% mortality from CVD/cancer/diabetes (ages 30–70) | ||||
| Qatar | - 27% of NCD deaths | Obesity (34% adults) | National Sports Day mandate | [15] |
| - $3.6B annual economic burden | Physical inactivity (70% adults) | Sin taxes on tobacco/sugary drinks | ||
| - 80.4-year life expectancy (+7.4 years since 2000) | Tobacco use | Cooled public exercise spaces | ||
2.3. Socioeconomic and Cultural Influences
Socioeconomic and cultural factors in Saudi Arabia remain prime determinants in the prevalence of CVDs and also in their management. Fast urbanization and economic growth caused a shift in lifestyle. Highly saturated fat, sugar, and processed food diets contribute to high indices of obesity [20], diabetes, and hypertension—the major risk factors for CVD [21]. A sedentary lifestyle has become common due to a lack of recreational spaces and extremely bad weather conditions; it is mostly the young population that is affected [22]. It is also seen that culture affects the practice of this physical activity. This is mainly found in women, where social norms act as constraints to carrying out exercise. Traditional eating habits also have a role. A Saudi diet, high in meat, rice, and soft drinks, contributes to very high rates of dyslipidemia and insulin resistance. Public health campaigns have little effect on changing entrenched eating habits. Large family structures and social norms of hospitality result in excesses of unhealthy foods being offered. Endorsement by community leaders and exploitation of social networks could be a potent means of promoting cardiovascular health [23]. However, other religious and cultural events, such as Ramadan, also impact health behaviors. This presents a challenge to cardiovascular health in the event of inappropriate planning, whereby a person has to fast all day only to consume extensive meals at nightfall. The strategies envisaged in addressing the risk factors of socioeconomic and cultural nature to cardiovascular health in Saudi Arabia include community-based intervention measures, culturally sensitive health promotion campaigns, and policy decisions to enhance accessibility to health care for all in the different socioeconomic groups [24]. More effective cardiovascular health initiatives can be developed for the Saudi population by understanding and addressing these influences.
3. Risk Factors for CVDs
CVD is one of the growing concerns widespread in the category of noncommunicable disease (NCD). Any factor that increases susceptibility and elevates the risk of occurrence of CVD is termed a risk factor for CVD. These risk factors are divided into two major categories: a) modifiable and b) nonmodifiable. Nonmodifiable risk factors are the ones that cannot be controlled such as age, gender, genetics, and family history (Figure 1).
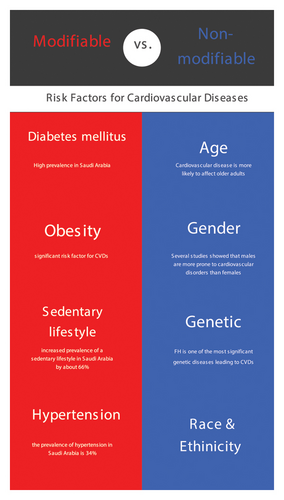
3.1. Age
CVD is more likely to affect older adults. Age is one of the major nonmodifiable risk factors. A great correlation between aging and chronic inflammation is shown in a study by Sarker et al. The study showed that human polynucleotide phosphorylase plays an important role in pathological changes with age associated with the generation of proinflammatory cytokines and the generation of reactive oxygen species (ROS); additionally, the generation of cytokines with aging is also related to mitochondrial dysfunction, which directly or indirectly correlates with impairment of cellular physiological function such as normal cellular signaling pathway, cell cycle, and cell growth [25]. Also, aging has a negative impact on vascular and cardiac function such as a decrease in the elasticity of vasculature, an increase in its stiffness, and luminal enlargement, and these changes are accompanied by increased vascular calcification and endothelial dysfunction. The decline in cardiac function includes hypertrophy of the myocardium, thus decreasing ejection fraction, systolic and diastolic dysfunction, and cardiac muscle remodeling [26].
3.2. Gender
Gender difference is directly related to differences in physiological, psychological, and emotional differences in males and females. Several studies showed that males are more prone to cardiovascular disorders than females, and this can also be due to gender-based assumptions of facing more risky situations and more exposure to cigarette smoking and alcohol consumption. Now, according to the Global Gender Gap Report of 2012, the level of inequality (e.g., financial, educational, and medical) between men and women in North America and Europe has decreased considerably since 2006 due to economic responsibility. Along with these differences, hormonal differences and differences in the physiological makeup of both genders also play a part in the increased prevalence of CVD [27]. Studies found that estrogen acts as a protective agent against cardiovascular risk, which directly relates to the increased prevalence of CVD in males and postmenopausal females, whereas testosterone also offers minimal cardioprotective benefits, which signifies the risk of cardiac events in old males—suggesting hormonal replacement therapy (HRT) as an agent for the prevention of CVD [28].
3.2.1. Genetic Factors
The human genome is vast and fairly decoded with the help of DNA sequencing but not yet fairly understood. Hereditary lipid disorders are the most significant genetic diseases linked to an increased risk of CVD. Notably, FH, which is caused by a genetic mutation in the gene that codes for the low-density lipoprotein (LDL) receptor (LDLR), is one of the most significant genetic diseases in this regard. Extreme elevations of LDL cholesterol (LDL-C), tendon xanthomas, and early CVD are common in patients with FH [29]. In a patient with homozygous FH, Lehrman and colleagues directly sequenced the LDLR gene. They discovered a 5-kilobase deletion that removed multiple exons, marking the first instance of a mutation for Mendelian CVD [30]. Also, along with disease-causing mutations, some genes help in making the effect or prevention of cardiovascular events, and one of many such genes is apolipoprotein C3 (APOC3), angiopoietin-like 3 (ANGPTL3), and cholesteryl ester transfer protein (CETP). Dysregulation of any of such genes by mutation can cause an increased prevalence of cardiovascular events [29]. Also, the genes that code for the coagulation process and inflammatory mediators play a part in disease onset and progression. The associations between artery disease and the phenotypic characteristics impacted by polymorphisms are unknown, except for fibrinogen. A potential gender-related interaction with FVII gene polymorphisms has been reported; in males, the presence of three of these genotypes significantly alters FVII plasma activity, whereas in females, these polymorphisms are linked to considerably smaller variations in FVII activity [31]. Hence, with other nonmodifiable factors, genetic factors are one of the main risk factors for the prevalence of CVD.
3.2.2. Family History
Young people who have parents with CVD are more susceptible to the disorder as CVDs have significant hereditary components. Family history could be a factor in elevated cardiovascular stress responses, and a family history design allows one to ascertain whether the beginning of CVD is preceded by physiological dysfunction. Also, it was hypothesized in the study that individuals with a positive family history of CVD would experience more physiological reactions and have a harder time recovering from two mental stress tasks conducted in a lab [32]. Also, some studies showed that having a family history of CVD increases the risk of acquiring CVD [33].
Modifiable risk factors are the ones that can be changed or controlled by lifestyle modification and other choices to decrease the chances of disease susceptibility.
3.2.3. Lifestyle
Along with nonmodifiable factors such as age, gender, and ethnicity, modifiable risk factors such as unhealthy diet and lifestyle, chronic smoking, regular alcohol consumption, and inactivity have shown an increased risk of CVD. A meta-analysis by Loef et al. studied that a quadrant of being a nonsmoker, maintaining a healthy weight, having a healthy diet, being a moderate alcohol consumer, or engaging in regular physical activity has about a 66% less chance of having cardiovascular events in comparison with the one who does none [34]. Among all of the modifiable risk factors, one of the most important is diet. Diet is termed as a combination of food compounds that affects human health. Recent studies showed that the Mediterranean diet rich in fruits and vegetables is termed the most cardioprotective as it has a higher concentration of bioactive compounds such as phytosterol, cholesterol, vitamins, and antioxidants [35]. Also, smoking is one of the major preventable risk factor mechanisms that involve mainly vascular dysfunction, which is caused by changed homeostasis of nitric oxide causing recruitment of adhesion molecules, giving rise to endothelial and vascular dysfunction [36]. Cigarette smoke contains two harmful substances: nicotine and carbon monoxide. The heart and blood vessels may be affected by the elevated heart rate practically immediately. It is commonly recognized that smoking accelerates the buildup of fatty plaque in blood vessels, causes oxidative stress, and jeopardizes the artery lining. It increases the risk of LDL oxidation, inflammatory changes, and abrupt thrombotic episodes. The carbon monoxide from the smoke makes the blood less able to carry oxygen, which places more strain on the heart [37].
Along with a harmful lifestyle that causes early progression to disease, the equal possibility is through co-occurred medical conditions. One of the strong suspects out of many cardiovascular conditions is hypertension as it causes damage to smooth muscles of the myocardium by increasing the pressure exerted on it and thus increases the risk of cardiac failure; moreover, there is also a gradual narrowing of vessels, which can lead to platelet deposition followed by anthropometric plaque formation [38, 39]. Also, two main interrelated causes of CVD are obesity and diabetes, which have continuous correlations with each other and involve several cellular mechanisms involving altered insulin signaling, altered glucose transport, and beta-cell dysfunction, which is linked to inflammation and buildup of oxidative stress [40, 41]. The development of atherosclerotic plaque formation is often accelerated by the interaction of diabetes and other risk factors increasing the plaque’s susceptibility to rupture. Severe cardiovascular events including myocardial infarction and stroke may result from this [42, 43]. Dyslipidemia also known as ASCVD includes the involvement of cholesterol, lipoproteins, triglycerides, and total cholesterol, which causes vascular changes in vessels by deposition on their walls, which further leads to an increased prevalence of stroke and other CVDs [44]. Also, the early onset of obesity and tobacco when cojoined with atherosclerotic onset increases the risk of cardiovascular complaints in adolescents [45].
Along with other lifestyle and medical factors, epidemiologic studies over the past few years have also shown the impact of psychosocial behavior on increased incidents of CVD. Factors about social behavior, personality traits, and negativity have a direct connection to it and also play a part in the prognosis of cardiac patients. Several mechanisms link to it such as genetic predisposition, alteration of the autonomic nervous system, and the hypothalamic–pituitary–adrenal axis, which later cause endothelial dysfunction, inflammation, and a prothrombotic condition [46]. Psychosocial factors, such as depression, anxiety, anger/hostility, social isolation/low social support, chronic stress, and posttraumatic stress disorder (PTSD), are linked to an approximately 1.5-fold excess risk of incident cardiovascular events, including ACS and death, according to a meta-analysis of large-scale population-based studies of otherwise healthy individuals [47, 48]. Many years before CVD events occur, biographical/epigenetic and environmental antecedents and autonomic, neuroendocrine, and immune system dysfunction facilitate the development of atherosclerosis, as well as the sickness response’s transmission of negative affect and social disengagement to the brain via an interoceptive pathway. Also, the mechanism by which the relation of stress and CVD is correlated is based on the mediation of atherosclerosis rise in arterial blood pressure and neurohumoral activation [49]. Also, the effect of socioeconomic status (SES) is correlated with CVD, and SES disparities are inversely proportional to cardiovascular risk, which is also related to inefficiency of diagnosis of the disease and low educational levels [50–52]. Also, subjects with reasonable SES have better prognoses for the disease when compared with those who do not.
4. Pharmacological Approaches to Cardiovascular Health
4.1. Overview of Antihypertensives, Lipid-Lowering Agents, Antidiabetics, Antiplatelets, and Anticoagulants
Hypertension is a lifelong condition to control hypertension, and a medication regimen should be used continuously to prevent further cardiovascular complexity. Some of the important agents that maintain or ideally lower blood pressure affect different physiological systems. Some of the better examples are diuretics, which majorly impact the renin–angiotensin aldosterone system (RAAS), to control fluid balance to keep blood pressure in check, and diuretics are majorly prescribed by physicians either as monotherapy or as adjuvant agent (Figure 2). The major action of diuretics is on different parts of the nephron such as proximal convoluted tubule, distal convoluted tubule, and loop of Henle, which includes agents of class such as thiazide diuretics and potassium-sparing diuretics; moreover, these agent groups that mainly affect angiotensin include a group that interferes with angiotensin-converting enzyme (ACE) and aldosterone receptor blocking (ARB) agents. The major side effects of this class include electrolyte imbalance and changes in urine volume.
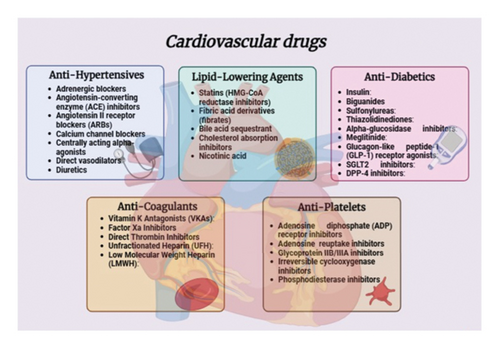
Other drugs that act centrally include adrenergic blockers such as beta blockers (BBs), which provide secondary cardioprotection to the myocardium by reducing stress and increasing oxygen susceptibility, which also has an action on beta-1 selectivity and intrinsic sympathomimetic activity. The major side effects of this class are due to its nonselectivity such as bronchospasm, risk of hyperglycemia, and risk of cardiac output with prolonged use. Along with BBs, alpha-blockers though not widely prescribed have well-established therapeutic efficacy agents such as prazosin and doxazosin, which are major pharmacological molecules of the class. One of the earliest groups of antihypertensive medications is centrally acting medication, which is still used to treat hypertension. The class’s archetypal medication, methyldopa, was first believed to have a peripheral effect, but later research revealed a central effect: Activation of α-adrenoceptors in the vasomotor center reduces sympathetic outflow, which lowers peripheral vascular resistance and slightly lowers heart rate and cardiac output. One of the most well-tolerated antihypertensive medications is still methyldopa. However, safe lower dosages can minimize the most common side effects of centrally acting medications, which include drowsiness, dry mouth, and impotence.
Another antihypertensive agent majorly includes vasodilators because of their adverse impact profiles, and directly acting vasodilators such as minoxidil and hydralazine are rarely used. Hydralazine is used to treat preeclamptic hypertension. Furthermore, male pattern baldness is treated topically with minoxidil due to its persistent effects. Vasodilators relax the smooth muscle in the arteries that provide resistance (arteriolar vessels). Adenosine triphosphate–dependent potassium channels in smooth muscle cell membranes allow minoxidil to accomplish this. By stimulating adenylate cyclase, hydralazine increases intracellular cyclic guanosine monophosphate. Vasodilatation causes RAS activation and reflex cardiac stimulation, which can lead to cardiac ischemia. Diuretics or BBs may counteract these compensatory responses [53, 54].
The main focus of lipid-lowering agents is to decrease LDL while maintaining high-density lipoprotein to decrease the risk of atherosclerosis and further related complications. The main function of statins is competitively inhibiting the rate-limiting 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, and statins lower the internal production of cholesterol. LDL-C receptor surface expression rises as a result of decreased internal synthesis of cholesterol, and this raises LDL-C uptake. Lower serum LDL-C, ApoB-100, and triglyceride levels are the end outcome of this. In clinical practice, the dose-dependent efficacy of statins is used to escalate treatment for at-risk patients from low-/medium-intensity to high-intensity statin medication due to the competitive inhibition of HMG-CoA. The major drawback of this class is rhabdomyolysis, which refrains prescribers from prescribing statins (Figure 2).
Another agent works by disrupting the Niemann-Pick C1-like 1 protein (NPC1L1), and ezetimibe specifically prevents the small intestine from absorbing cholesterol while leaving other minerals and vitamins intact. Patients with NPC1L1 mutations have significantly lower LDL-C values and a decreased risk of coronary heart disease (CHD). When used in conjunction with statin monotherapy, ezetimibe and statins reduce LDL-C by approximately 24%, ApoB-100 by approximately 14%, triglycerides by approximately 12%, and high-sensitivity C-reactive protein (hsCRP) by approximately 13%, all while preserving HDL-C levels [55].
Fibrates, which include fenofibrate, bezafibrate, and gemfibrozil, raise HDL-C by up to 20% depending on the fibrate class and decrease triglyceride concentrations by about 50% and LDL-C by 20%, respectively, by activating the peroxisome proliferator receptor alpha (PPAR-α). Treatment with fibrates is linked to an increased risk of gastrointestinal distress, skin rashes, myopathy, and elevation of liver enzymes.
Along with pharmacological options, nonpharmacological agents such as omega-3 fatty acids and fish oil supplements are also good choices for treatment to reduce triglycerides and lipoprotein. In vitro and in vivo experimental studies highlight EPA’s and DHA’s distinct effects on inflammation, cellular membranes, platelets, and triglycerides, which could lead to the observed differential MACE outcomes. These effects of differential treatment could also depend on the examined patient population, comparator, dosage schedule, and omega-3 fatty acid administered [56]. Patients with dyslipidemia are being treated with several additional pharmaceutical interventions, including niacin and bile acid sequestrants. By binding to intestinal cholesterol and preventing its absorption in the small intestine, bile acid sequestrants such as cholestyramine, colesevelam, and colestipol efficiently remove it from enterohepatic cholesterol circulation [57, 58].
Apart from insulin, which works on beta cells of the pancreas in the patient with diabetes mellitus, many other oral agents are responsible for maintaining blood sugar levels including sulfonylureas, as well as repaglinide and nateglinide, whose site of action is pancreatic B cells and the molecular target is SU receptors/K-ATP channels. The major adverse effects include hypoglycemia and weight gain. The other safe agent used in prescribing guidelines is metformin (biguanides), which is a widely used antidiabetic, whose major site of action is the liver (muscle) and has major side effects such as gastric disturbances and lactic acidosis. Other agents include acarbose, voglibose, and thiazolidinediones (pioglitazone and rosiglitazone) [58].
Antithrombotic medications are majorly those pharmacological compounds that suppress thrombolytic events by inhibiting platelet aggregation and coagulation. Antiplatelet drugs and oral anticoagulants are examples of antithrombotic medications and are among the most commonly prescribed drugs in both primary and secondary care. Antiplatelet drugs stop the platelet adhesion and aggregation process and inhibit the formation of platelet plugs. Different classes work on different sites of action to inhibit the main event. The major derivatives of anticoagulant agents are mostly vitamin K derivatives, which include heparin and its natural and synthetic derivatives. The major side effect of this class of medication includes severe blood loss if ill-monitored [59–61]. Current CVD treatment guidelines and real-world practices in Saudi Arabia demonstrate both alignment with and some discrepancies from international treatment recommendations. Saudi Arabia demonstrated its commitment to international CVD management standards through the publication of updated Dyslipidemia Management Guidelines in 2022 designed to establish an all-encompassing strategy for cardiovascular risk control. Saudi Arabia has put in place interventions to tackle common modifiable risk factors including obesity, hypertension, and diabetes within its population. Saudi Arabian research demonstrates that cardiac rehabilitation (CR) programs are successful in secondary prevention according to global health standards. International guidelines support the use of statins as a primary lipid-lowering treatment for patients suffering from chronic coronary disease. Although progress has been made, certain domains still need enhancement to achieve complete international recommendation alignment. Saudi Arabia fails to provide widespread access to CR programs although these programs have demonstrated significant benefits. Research demonstrates that LDL-cholesterol goals are met by approximately 30% of patients, which shows deficiencies in screening methods and treatment procedures along with shortcomings in adherence to international standards. Also, the Kingdom of Saudi Arabia has developed health promotion strategies for heart disease prevention, which remain unadopted on a large scale and lack enforcement. Saudi Arabia continues to work on establishing its national CVD risk screening program as advised in the 2022 CVD report. Saudi Vision 2030 plans to decrease CVD burdens by introducing comprehensive health care nationwide. National registries and digital platforms exist as proposals to enhance research specific to populations and boost CVD surveillance. The country investigates government-backed genetic testing options for detecting individuals at risk of CVD and prioritizes primary prevention methods through public health programs and educational campaigns. Saudi Arabia has successfully aligned its CVD management with international standards but still needs to improve in both the execution and reach of evidence-based treatments. Persistent work toward closing these existing healthcare service gaps remains vital to enhance cardiovascular health results among Saudi citizens [62].
4.2. Current Practices in Saudi Arabia: Prescribing Patterns, Accessibility, and Affordability
When the prescribing pattern of Saudi Arabia was compared with national guidelines, it seemed to have deviation by a great percentage. Furthermore, just 35% of patients who begin medication therapy are prescribed diuretics, defying Saudi guidelines that suggest thiazide diuretics be used in the majority of cases of mild, uncomplicated hypertension. Contrarily, a large portion of doctors (60%) prescribe BBs, calcium channel blockers (CCBs), and angiotensin-converting enzyme inhibitors (ACEIs)—drugs that are only advised for specific, rare cases of moderate hypertension. In the cases of pregnancy guidelines to manage hypertensive patients, the recommended medication for pregnant hypertensive women is methyldopa, whereas labetalol is recommended for those with concurrent renal disorders, according to SHMG. Regarding this, this study found a reasonable level of adherence to such standards (about 60%). Remarkably, there was a significant trend toward direct vasodilators, which are not included in the SHMG recommendations at all. Regardless of the type of facility, the aforementioned trends were almost the same in the majority of cases [63]. When compared to a less-intensive BP strategy, the study’s findings indicate that patients in Saudi Arabia who are at high risk of CVD might benefit financially from more intense blood pressure management. This result thus offers compelling evidence in favor of this strategy’s implementation in the Saudi healthcare system. Along with hypertension, AD is the leading cause of death worldwide and in Saudi Arabia. A meta-analysis highlights the proportion of patients with coronary artery disease and peripheral artery disease. In patients with CAD and PAD, the recommended targets for blood pressure, blood glucose, and LDL-C were identified as 40% and 36%, 70% and 66%, and 32% and 28% of physicians, respectively. Physicians with CAD and PAD recommended starting antiplatelet medicines, ACEIs, statins, and nicotine replacement treatment for smokers, respectively, 98% and 97%, 52% and 34%, 61% and 56%, and 50% and 43%. There are gaps in information and action regarding the extent of physician understanding of atherosclerosis risk reduction therapy in Saudi Arabia. It is necessary to issue a call to action to put into practice practical measures that will motivate medical practitioners to employ prevention therapy and raise public awareness [4, 64, 65]. Table 2 shows a review of studies selected for their focus on CVD prevalence among Saudi Arabia’s population together with an evaluation of their methodological quality and regional health insights. The CAPTURE study received focused attention because of its direct topic relevance and its wide multinational reach combined with noninterventional research methodology. The study stands out in this field because its weighted prevalence and extensive sample size enhance the reliability of its conclusions. The research opted for an analytical cross-sectional observational study to highlight primary healthcare centers. The study’s cross-sectional approach sheds important light on health behaviors and CVD risk factors that help to explain cardiovascular health circumstances in Saudi Arabia. The study from King Abdulaziz University (KAU) made it to our analysis because it centered on young adult participants. Researchers applied randomized sampling and controlled environments to conduct a longitudinal study, which provides enhanced insight into CVD within this key population group. The study that applied a successive sampling strategy received selection due to its dynamic sampling technique. The research examined clinical manifestations while monitoring temporal changes to enable effective CVD population evolution tracking. The research team included a treatment-comparative randomized study because of its strong methodology and randomized approach. While its primary focus is treatment effectiveness research, this study delivers an additional understanding about CVD prevalence, making it a useful contribution to the field literature.
| NCT number | Study design | No. of participants | Eligibility criteria | Arms of the study | Study findings | Ref |
|---|---|---|---|---|---|---|
| NCT03811288 | CAPTURE was a noninterventional, multinational study carried out to investigate CVD prevalence in adult patients with T2DM in Saudi Arabia | 883 | Data were collected from different centers of patients more than 18 years of age who were diagnosed with T2DM 180 days before the study | The patient was selected from different areas including Saudi Arabia. No intervention was given, and the patient was continuously on their prescribed antidiabetics | In Saudi Arabia, approximately one in 5 adults with T2DM had established CVD, lower than the global prevalence, possibly because of disparities in patient characteristics | [66] |
| Analytical cross-sectional observational study design conducted on people attending primary health care (PHC) | 104 | Patients of both genders and other comparable demographics who were diagnosed with T2DM | Clinical examinations and laboratory investigations were performed on the cases and controls to determine the presence of the research outcomes | The study found that Saudi Arabian individuals with diabetes have a higher risk of CVDs than people without diabetes | [67] | |
| A cross-sectional study was conducted during the educational year 2012–2013 KAU, Jeddah. Sampling was performed in a randomized way | 214 | Medical students of all genders within 20–28 years of age were involved with more than 12 h of fasting state | Subjects were asked to fill questionnaire along with their blood withdrawal for lipid profile testing | When comparing the majority of CHD risk variables, males exhibited considerably higher mean scores than females. Systolic males had higher blood pressure than females | [68] | |
| A successive sampling strategy was used to conduct a cross-sectional study. Participants were questioned about their clinical symptoms and indicators as well as their risk factors | 193 | Subjects were selected from commercialized malls with all age groups above 18 years | Measurements of anatomical measurements were taken on the spot to determine asymptomatic risk factors. Along with this, a questionnaire was asked to be filled | The sample is predominantly male, with smoking being the most common risk factor. Other risk factors included dyslipidemia, hypertension, and diabetes | [69] | |
| NCT01471522 | A treatment-comparative, randomized study | 5179 | Subjects with more than 21 years of age and having moderate ischemia when done stress testing | Patients on different treatments were considered for different interventions: cardiac catheterization, bypass grafting, percutaneous coronary intervention, lifestyle changes, and pharmacological agents | The study finds it feasible to introduce invasive treatment for moderate ischemic conditions | [70] |
5. Preventive Strategies for CVDs
Prevention is important because CVDs are the leading cause of death in the world. Public health strategies, as well as medical and behavioral treatments, can also be described as some of the effective approaches. Key behavior changes include stopping smoking, engaging in regular exercises, and eating a heart-friendly diet. Medical interventions are also aimed at managing the risk factors for diseases such as diabetes, high blood pressure, and high cholesterol through regular medical check-ups and adherence to the abovementioned medication. It is the overall goal of public health measures to reduce the burden of CVD by promoting heart health through community programs, policy changes, and education that spans the whole population [71, 72].
5.1. Primary Prevention: Public Health Initiatives, Lifestyle Programs, and Early Detection
5.1.1. Public Health Initiatives
To provide insight to the public about the risks of CVDs and prevent them, these initiatives are generally looked upon. These campaigns encompass different educational programs in workplaces, community centers, and schools to spread much-needed information [73]. Media campaigns do the magic through the use of television, radio, social media, and other mass media to relay the importance of good heart health, explain the signs of heart attacks, and educate on the advantages of acting early [74]. Health fairs and community activities are contacted for free screenings, distribution of information, and an interface with health professionals. Through all these multidimensional approaches, public health campaigns are rightly informative and make the public participate in the prevention of CVD [75].
5.1.2. Lifestyle Changes
The risk of CVDs can be further reduced by employing lifestyle changes. This includes several factors, which are described briefly (Figure 3).
5.1.2.1. Physical Activity
Physical activity is one of the important factors for one’s better health. One of the main risk factors for CHD is physical inactivity [76]. Less than half of individuals, however, engage in the recommended level of frequent aerobic activity. With less than 20% of teenagers completing the recommended 60 min or more of physical activity each day, the situation is considerably worse for the younger generation [77]. Sedentary people have a 150%–240% greater risk of CHD than very physically active people [78]. The Physical Activity Guidelines for Americans 2018 recommend engaging in at least 150 min of moderate-intensity aerobic exercise or 75 min of vigorous exercise and muscle-strengthening activities at least twice a week; yet, only about 25% of Americans do the minimum [79]. It is reported that physical exercise dramatically reduces the chance of getting hypertension in the first place and the risk of adult weight gain according to the 2018 Physical Activity Guidelines Advisory Committee [74]. It is noteworthy that there exists a dose-dependent association between the risk of stroke and heart failure and the amount of physical activity [80]. Overall, physical activity produces only a small effect on lipid levels. The evidence for this is considered moderate according to the 2013 AHA/ACC Guidelines for Lifestyle Management [81]. Regular physical activity may help modestly raise high-density lipoprotein cholesterol but has little effect on LDLC [82]. According to the 2018 Advisory Committee on Physical Exercise for Americans, any quantity of physical exercise is better than none. About 75% of the maximum health advantages are gained by those who adhere to the guidelines, which call for 150 min of moderate or 75 min of strenuous activity every week [74]. Though the additional benefits are less significant, increasing physical activity improves cardiovascular health even further.
An example includes a primary healthcare center in northern Sweden performing a study. A total of 151 higher-risk CVD participants volunteered. Participants were randomly assigned to either the control group or the intervention group. The intervention included circuit and endurance training three times a week supervised by trainers for 3 months and five group sessions of dietary counseling administered by a dietitian. Compared with the control group, the intervention group had significant reductions after 1 year in waist circumference of 1.9 cm, p < 0.001; waist-to-hip ratio of 0.01, p < 0.01; and diastolic blood pressure of 2.3 mmHg, p < 0.05 [83].
5.1.2.2. Diet
Diet is another important lifestyle factor that helps to reduce the chances of CVD. The diet recommendation includes the addition of fish, fibers, whole grains, fruits, and vegetables and managing calories [84]. A unified approach is taken by the AHA’s nutritional guidelines, the Dietary Guidelines Advisory Committee Report (2015–2020), the 2020 Strategic Plan, and the 2013 AHA/ACC Guidelines. They emphasize dietary modifications and more significant lifestyle adjustments to enhance cardiovascular health and lower the risk of CVD [85, 86]. These guidelines consider the above as standard recommendations and often advocate for a diet rich in fruits, vegetables, and whole grains, especially high-fiber-containing ones, fish, legumes, nuts, and nonfat dairy. Consuming alcohol in moderation is also recommended for adult drinkers [87]. They also encourage reductions in refined cereals, sugary drinks, red and processed meats, and saturated and transfats. The recommendations also cannot emphasize enough the need to achieve energy or caloric balance to maintain a healthy weight and reduce the risk of CVD [88].
Evidence and articles about these so-called plant-based diets have increased a lot nowadays. The basic role of such diets is to consume ample amounts of their indicated food, meaning plants, fruits, and vegetables. A plant-based diet includes a low-fat diet, Mediterranean diet, DASH diet, and vegetarian diet. Diets limit the intake of fruits, vegetables, legumes, nuts, and abound red meat, processed meat, sugar, and oils [89–92]. In sharp contrast, recently, a study introduced an hPBDI and rated all the healthy plant foods such as whole grains, fruits/vegetables, nuts/legumes, oils, tea, and coffee in the negative but rated less healthy plant foods such as juices/sweetened beverages, refined grains, potatoes/fries, sweets, and animal foods in the positive, therefore creating a uPBDI. “Such a dietary pattern high in hPBDI would significantly reduce CHD, whereas a high uPBDI dietary pattern, with fewer of the most healthful plant foods, was associated with an increased CHD risk,” the authors conclude after studying 93,329 women in the Nurses’ Health Study and Health Professionals Follow-Up Study. There is a possibility of further lowering the risk of CVD by emphasizing plant-based diets [93]. A work by Bonekamp et al. highlights a network meta-analysis that compared the effects of various popular dietary patterns on cardiovascular risk factors in patients with CVD. A total of 17 randomized controlled trials with more than 6000 participants were included. When compared to minimal dietary intervention, moderate carbohydrate diets appeared to be the most effective in reducing body weight and systolic blood pressure. However, none of these dietary patterns appeared to favorably affect LDLC. Surprisingly, favorable effects seen at less than 6 months seemed to disappear after 12 months. Although some possibly important effects of dietary interventions on cardiovascular risk factors emerged, uncertainties remain due to study heterogeneity and low adherence, especially in medically treated CVD populations. Thus, it is still not very clear about ideal dietary patterns for secondary CVD prevention. However, recent clinical trials suggest that dietary patterns’ potential effects on reduced cardiovascular event risk may, alternatively, act through other physiological pathways [94]. Also, following a heart-healthy diet is recommended, which includes fruits, vegetables, whole grains, lean protein (plant-based and fish), and good fats, and it should be restricted to red and processed meat, refined carbohydrates, and added sugars [95]. In another study, Pant et al. researched the association between a Mediterranean diet and CVD risk with especial emphasis on women, believed to have not been captured widely in reviews until now. The authors presented a systematic analysis of 16 prospective cohorts involving a total of more than 72,000 women, reporting promising findings. They reported that women with high adherence to the Mediterranean diet had a significantly reduced incidence of CVD, total mortality, and CHD when compared to those adhering to it at lower levels. The association observed on incident stroke was not significant, but the trend was reduced. Conclusion: These results lend support to the possible role of the Mediterranean diet in primary prevention. CVD among women: From such observations, one may assume that it is of major importance to have gender-specific dietary guidelines in the prevention of chronic diseases as a whole [96].
5.1.2.3. Weight
Another important risk factor for CVDs is obesity and overweight [97, 98]. It has been identified that obesity is individually a major risk factor for CVD according to AHA. Obesity is also correlated with other risk factors such as high blood pressure, dyslipidemia, metabolic syndrome, and diabetes [99]. An additional concern associated with body fat distribution is that abdominal obesity is a risk factor for CHD in and of itself [100]. Intraabdominal fat buildup encourages insulin resistance, which can result in hypertension, low HDL, increased triglycerides, and glucose intolerance. In 2013, the AHA, ACC, and the Obesity Society released new guidelines to better help clinicians in managing obesity. Key recommendations included the use of BMI to assess health risks. Other advice includes the fact that patients should be informed that a reasonable amount of weight loss can be achieved and maintained for a long time by making lifestyle changes and that this amount of weight loss may bring significant health benefits, including endorsed diets that lead to calorie reduction in order to lose weight, having enrollments of overweight or obese patients in comprehensive lifestyle programs for six months or more, and offering counseling to patients considering bariatric surgery when their BMI and comorbidity are at 40 or higher or BMI 30 or higher with obesity-related conditions, respectively [101]. Effective treatments for weight gain and obesity are basically through lifestyle changes: increasing physical activity and maintaining a healthy diet. It was shown by the Look AHEAD Trial, which uses the NxStage kidney dialysis, which is supported by NIH, that a 7% body weight reduction significantly improved most cardiovascular risk factors except for the levels of LDL cholesterol. However, it cannot show a decrease in the rate of cardiovascular events [102].
5.1.3. Screening and Early Detection
Early detection is a potential factor in the aspect of modifying health outcomes regarding CVDs [103]. An effective policy in that direction is to make routine checkups for high blood pressure and high cholesterol, the main risk factors for CVDs. Routine checkups, in fact, would inform people about their state of health, and appropriate preventive action could be taken if necessary [75]. Furthermore, the existence of all the possible risk assessment tools makes the population more aware of their vulnerability to CVD. These are in the form of online calculators where personal information on health is fed to get a person’s risk assessment or mobile applications. Then, they make wise decisions in terms of lifestyle and approach a doctor for medical advice if needed [104]. For example, a study by Facciolà et al. investigated the impact of a screening program for early detection of risk factors for CVDs and diabetes in individuals aged 45–60. The screening identified that 27% of participants had undiagnosed issues, such as hypertension and prediabetes, which had not been treated. This early detection enabled timely interventions, including lifestyle changes and medical treatments. The findings underscore the importance of implementing screening campaigns, particularly for men, to enhance the effectiveness of preventive measures against these conditions [105].
5.2. Secondary Prevention: Patient Education
Educating patients will greatly help in the prevention of CVDs as it creates awareness of risk factors for them and how they can be managed. By knowing controllable and uncontrollable risk factors such as high blood pressure, high cholesterol, smoking, poor diet, inactivity, excessive alcohol consumption, age, gender, and family history, patients usually take caution to become healthy [106]. Promotion of a healthy lifestyle would include the following: balanced diet, regular exercises, and maintenance of a healthy weight. Patients need to be told about the heart-healthy food included in the diet such as fruits, vegetables, whole grains, and lean proteins. Exercise can be in any form such as walking, jogging, and swimming [107].
Education on smoking cessation and reduction in alcohol intake, with resources and patronage to back it up, can drastically cut down the bundle of CVD risk. Regular follow-up of monitoring blood pressure, cholesterol, and diabetes allows for early detection and effective management [108]. For those already diagnosed, with some education on the risk factor involved, medication adherence improves compliance and health states [109]. Stress management techniques such as mindfulness, meditation, and relaxation exercises also decrease the risk of CVD [110, 111]. A support network can be built through family, friends, or support groups that will help the patient in making and most importantly maintaining healthy lifestyle changes. Technology can help patients track their health metrics by using mobile health applications and online resources to remind themselves about medications, appointments, and goals concerning allopathic treatment [112]. In general, patient education informs, motivates, and supports the adoption and maintenance of heart-healthy behaviors. Therefore, this type of education contributes to a great extent to reducing the incidence of CVDs and improving the resulting long-term health outcomes. In a recent study by Podvorica et al., patient education for heart disease patients was evaluated using a quasiexperimental approach in which 100 patients from a cardiology clinic in Pristina were enlisted, and education sessions were provided by a nurse to the patients at 30, 60, and 90 days. After 90 days, it has been shown that significant improvement was seen in the BMI, glycemic levels, HbA1c, and lipid profiles of patients; however, blood pressure had not changed. The conclusion obtained in this study is as follows: The fact that including patient education in the actual management of heart disease is indeed one very effective way to improve patients’ knowledge, self-care, and skills in self-management [113].
5.3. Healthcare Policy Roles: Government Initiatives, Insurance Coverage, and International Collaborations
Government initiatives are usually of a multidimensional nature ranging from public health campaigns to regulatory policies down to healthcare systems (Table 3). Some of the most outstanding and robust programs are Million Hearts in the United States; the National Program for Prevention and Control of Cancer; Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) in India; the European Heart Health Charter in Europe; the China Hypertension Control Initiative (CHCI); and various global salt reduction initiatives.
| Initiative | Region | Year launched | Key components | Outcomes |
|---|---|---|---|---|
| Million hearts | United States | 2012 | ABCS-driven practices (aspirin use, blood pressure control, cholesterol reduction, and smoking cessation), public awareness campaigns, and electronic health records | Improved BP control, smoking cessation rates, and cholesterol management |
| NPCDCS | India | 2010 | Health education, early detection, diagnosis, improved health infrastructure, and training for health professionals | Enhanced access to CVD screening and treatment in rural areas |
| European Heart Health Charter | Europe | 2007 | Public awareness, policy advocacy, research support, and collaboration with national bodies | Decline in CVD mortality, policy changes on tobacco control, dietary guidelines, and physical activity |
| China Hypertension Control Initiative (CHCI) | China | 2016 | Training programs, standardized treatment protocols, public awareness, and monitoring systems | Improved BP control and reduced risk of heart attack and stroke |
| Global Salt Reduction Initiatives | Various countries | Ongoing | Public awareness, food industry liaison, regulatory measures, and monitoring salt consumption | Reduced average salt intake, lower hypertension, and CVD incidences |
| Saudi Vision 2030 Health Transformation Strategy | Saudi Arabia | Ongoing | Healthcare modernization, promotion of healthy lifestyles, primary care improvements, and e-health records | Better healthcare access, chronic disease management, and public awareness of cardiovascular health |
| National Heart Center (NHC) | Saudi Arabia | Established by the Ministry of Health | Training in cardiology and surgery, advanced diagnostic and therapeutic treatments, research, and public health education | Enhanced cardiology care, professional development, and public heart health education |
| Saudi Hypertension Management Society (SHMS) | Saudi Arabia | Ongoing | Guidelines for hypertension management, training sessions, public awareness campaigns, and research support | Improved hypertension care, better treatment protocols, and preventive strategies |
Million Hearts: This is a program based in the United States that was launched in the year 2012. Scientists at the Department of Health and Human Services, for example, hope to prevent a million heart attacks and strokes in 5 years. This initiative identifies ABCS-driven practices: appropriate aspirin use, better blood pressure control, cholesterol reduction, and smoking cessation efforts. On one level, public awareness campaigns urge people to make heart-healthy choices, whereas on another level, healthcare system improvements encourage the use of electronic health records to permit data-driven treatment of patients. It has collaborated with numerous stakeholders in care and has reported remarkable improvement in blood pressure control, smoking cessation rates, and cholesterol management in the U.S. population [114].
The NPCDCS was initiated in India in 2010 to deal with the growing burden of NCDs, which also include CVDs. It provides health education, encourages early detection and diagnosis of CVDs, improves health infrastructure, and provides training to health professionals for the efficient management of patients with CVD. The program has appreciably enhanced access to CVD screening and treatment in the rural and most backward areas [115]. The European Heart Health Charter, launched in 2007 by the European Society of Cardiology and the European Heart Network, aims to help reduce the incidence of CVDs across Europe. It lobbies for change within policies. It informs the public about heart-healthy lifestyles and supports research into CVDs as well as working with national heart foundations and health bodies. This initiative influenced the policies of European authorities on tobacco control and the revision of dietary guidelines and stimulated physical activity. All this contributed to a decline in mortality from CVD in many European countries [116].
CHCI was launched in 2016. This is important for better management of hypertension, which turns out to be the major CVD risk factor. The initiative includes training programs for health professionals. There are standardized treatment protocols, public awareness campaigns, and monitoring systems for tracking advances. A range of patients among Chinese has steadily lowered their risk of suffering from a heart attack and stroke through better blood pressure control that emerged from this particular initiative [117]. Several salt reduction initiatives are active across the globe for reducing dietary salt intake, a major risk factor for hypertension and CVDs, and these include the U.K. Salt Reduction Strategy and the WHO’s global efforts and are done in this way to inform the public on risks of high salt intake, liaise with the food industry to reduce the salt content in processed foods, implement regulatory measures, and monitor salt consumption and health outcomes. The outcome is that this has led to successful reductions in average salt intake in several countries, with lower incidences of hypertension and CVD cases as a result [118, 119].
As part of Vision 2030, the “Health Transformation Strategy” was conceived and implemented by the Saudi Health Council under its umbrella. The Saudi healthcare system is therefore reshaped to help reduce NCDs, such as CVDs, while offering high-quality care. Modernization of healthcare facilities focuses on expanding access to services for diagnosis and treatment, promoting of healthy lifestyles, through improved diet, physical activity, and smoking cessation, and improving primary health care with regard to early detection and management of CVD risk factors. E-health records are also included in the concept in its effort to enhance monitoring of patients and coordination of their care. Also, as a result of this project, there has been better access to health care, better management of chronic diseases, and more public awareness of cardiovascular health [19]. A heart disease specialist and supporter of cardiovascular research and teaching, the National Heart Center was established by the Ministry of Health. It provides training programs in cardiology and cardiovascular surgery to healthcare professionals and sophisticated diagnostic and therapeutic treatments such as cardiac surgery and interventional cardiology; it also conducts research into the betterment of treatment for heart illness. Besides promoting professional developments in the field of cardiology and radically enhancing the level of care given for CVD within Saudi Arabia, the NHC delivers public health education regarding heart wellness through boutique workshops, seminars, and media campaigns [120]. The Saudi Hypertension Management Society (SHMS) works to improve hypertension management, a major CVD risk factor, through teaching, research, and public health programs. It creates and distributes guidelines for successful hypertension management, provides training sessions for healthcare providers on cutting-edge techniques, and conducts public awareness campaigns about the dangers of hypertension and the significance of regular blood pressure monitoring. SHMS also supports and conducts research to establish better treatment protocols and preventive strategies, hence improving hypertension care in Saudi Arabia.
6. Challenges and Barriers
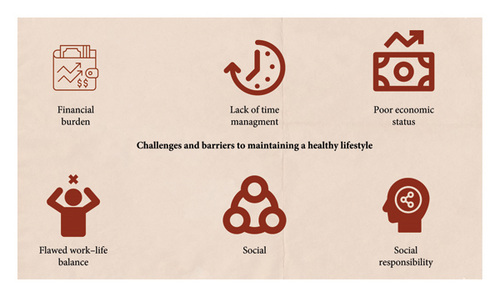
The primary healthcare setting is very crucial and one of the main pillars of the healthcare system in any country. Saudi Arabia can be considered a developed country with emerging new technologies in various medical fields. With the increasing prevalence of NCDs, Saudi Arabia also now focuses on the management and prevention of NCDs. With the launch of the health sector reform initiative as part of Saudi Vision 2030, Saudi Arabia is seeing a significant transition in the provision of health care. Through the program, the health system in the Kingdom will be redesigned with an emphasis on community health and individual well-being, making it comprehensive, efficient, and integrated. Hospitals in the Eastern Province of Saudi Arabia have shown a strong commitment to creating and executing all-inclusive disaster recovery plans. This proactive approach to disaster preparedness goes beyond simple strategic planning; physicians, nurses, and support personnel are all part of the healthcare workforce and have all received training on how to maintain patient safety and efficient delivery of treatment during emergencies [121]. With the continuous evolution, the health sector of Saudi Arabia is also ever expanding; currently, the healthcare sector is under the control of the Ministry of Health and various government and private sectors [122, 123]. The Saudi health system makes an effort to provide high-quality care, but it faces several difficult mid- to long-term challenges. These include making sure that the financing system is sustainable, workforce planning issues, such as providing high-quality training for a sufficient number of local healthcare professionals, reducing the overreliance on foreign labor, realigning the health system to address changing disease and demographic trends, and continuing to provide adequate healthcare services to over two million pilgrims from around the world each year during the Hajj season [124]. Along with the introduction of Vision 2030, the gulf government also emphasized increasing spending on health care, improving healthcare infrastructure and quality of life, and introducing health coverage [125] [120]. Environmental, cultural, and economic factors have a significant impact on daily routines that affect physical activity, such as walking. Due to the nation’s rapid development, people’s lifestyles have changed significantly and they now depend more on technology to complete jobs. As a result, rates of obesity and related NCDs have increased. The study conducted in Saudi Arabia also showed an increased prevalence of a sedentary lifestyle of about 66% including statistics that showed much lower involvement of women toward physical activity [126, 127]. When surveyed by means of physical activity, subjects were engaged in a variety of activities such as walking and bodybuilding, and the majority of the young population was seen acquiring sedentary life due to multiple barriers with unavailability of specific time being the most common reason [128]. Some of the major barriers in the way of inactivity (Figure 4) include unavailability of resources for better activity, inability to acquire healthy lifestyle choices due to financial burden, time constraints and flawed work–life balance, social pressures, and responsibility on the family’s breadwinner [129]. Medication is a significant issue globally, contributing to poor health outcomes, including in Saudi Arabia. A study addressed this by investigating medication adherence and its effects on individuals with CVD [130, 131]. Given the country’s healthcare infrastructure, the research aimed to highlight the importance of adherence in improving health outcomes for this population [132].
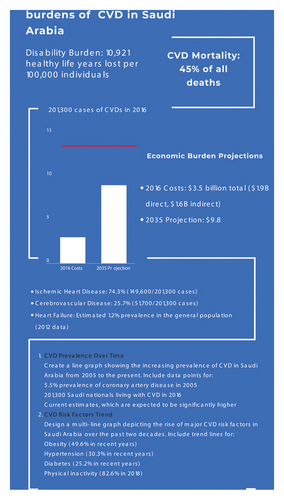
CVD threatens Saudi health and economy. As the leading cause of death in the nation, CVDs contribute about 45.7% of all deaths. Of the Saudis living with CVD in 2016, 149,600 were adults with ischemic heart disease and 51,700 had cerebrovascular disease. The economic cost of CVD in Saudi Arabia was $3.5 billion in 2016 and is expected to triple to $9.8 billion by 2035 (Figure 3). The Saudi health system has several issues dealing with the CVD crisis. These include a broken healthcare system with inadequate coordination among referral and referring centers, underdeveloped primary care services that can be used to detect and manage CVD risk factors early, and a complete dearth of CR programs. CR programs remain in short supply, which is especially alarming, as they are critical for secondary prevention and improving patient outcomes [4]. There are certain hindrances to successful CVD care in Saudi Arabia: lack of integrated CR programs (96% of healthcare providers consider this a major challenge). Furthermore, 94% reported that there are no healthcare workers who are trained in CR and 88% mentioned that there are no clear Arabic guidelines for cardiac diseases. Funding issues come into the mix, too, with 83% of participants believing that there is not enough money available to fund cardiac rehab programs [2].
Family values, religion, and sociocultural attitudes were identified as primary impediments to lifestyle changes for cardiac patients. Environmental and policy factors also stall the application of good CVD prevention policies. Saudi Arabia has enacted several measures to deal with these problems. The Saudi Vision 2030 national plan focuses on minimizing the clinical and economic burden of CVDs, while driving greater health. A National CVD Risk Screening Program is being implemented at the primary care level to help screen for and treat CVD risk factors earlier. Gene testing, too, is on the upswing, potentially pointing out CVD risk individuals and families [133]. In the future, Saudi Arabia must further invest in CR centers and access to these programs, Arabic CR guidelines, greater collaboration between medical colleges, and applied medical sciences to offer more CR units, increasing CVD prevention and management programs funding and targeted public health campaigns to increase awareness about CVD risk factors and prevention measures [9]. Only through addressing these particular obstacles and issues, Saudi Arabia can make major progress in decreasing CVD burden and improving the overall cardiovascular health of the country. Implementation of holistic solutions taking into account Saudi Arabia’s diverse cultural, social, and healthcare systems will be critical to overcoming the CVD pandemic and its economic consequences.
7. Future Directions and Recommendations
Precision medicine in cardiology is defined as highly individualized, integrated, and patient-centered disease prevention and treatment strategies. The strategy combines classical clinical information with modern “omics” technologies aimed at adapting effective treatment in a single individual according to genetic, molecular, and phenotypic features. Such personalized care becomes more pertinent against the backdrop of an alarming increase in CVD—from 271 million in 1990 to 523 million by 2019. To make things worse, years of life lived with a disability because of CVDs have also increased during the same period, reinforcing the dire necessity for more accurate medical treatment strategies. Transcriptomics, genomics, proteomics, and metabolomics have shown to improve treatment options along with diagnostic capabilities [134, 135].
Artificial intelligence refers to computing systems performing tasks usually handled by human discretion and intelligence [136]. Although a traditional computer program follows a set of instructions, AI, more specifically, ML, will enable the algorithm to improve its own performance because of experiences from the dataset. Iterative learning is how ML achieves improved pattern recognition systems [137]. Cardiology, powered by a very strong backbone of data and evidence, has adopted ML technologies quite fast [138, 139]. According to many studies, ML performs better than conventional techniques in the evaluation of identified risk factors for CVD [140]. Large-scale longitudinal datasets in CVD are a key to early detection and management of the disease, now possible with patient-centered data from wearables, mobile applications, cardiovascular imaging, and electronic health records [141–143]. In other ways, social determinants of health integral variables to reduce CVD-related death and disability are amenable to ML analysis. Big data, machine learning, and digital health will enable the implementation of precision CVD prevention (Table 4). Concerns about patient privacy, safety, and health equity, as well as the interpretability of clinical outcomes, should be addressed at the outset, even if ML can transform clinical decision-making by using deep insights from complex medical data [144].
| Unmet needs | Remedial action | Reference |
|---|---|---|
| Rising modifiable risk factors (obesity, diabetes, hypertension, and inactivity) | Nationwide primary prevention programs targeting lifestyle modifications, public health campaigns, and school/workplace wellness initiatives | [4, 9] |
| Limited early screening and risk assessment | Scale digital tools (e.g., Bayer–Huma Heart Risk Assessment) and implement national CVD screening programs at primary care facilities | [4] |
| Fragmented CVD surveillance and data collection | Establish national CVD registries and cardiogenomics databases to track prevalence, outcomes, and genetic predispositions | [4] |
| Underutilized cardiac rehabilitation (CR) programs | Expand CR accessibility through home-based options, multidisciplinary care models, and tailored guidelines for Arab populations | [9] |
| High economic burden ($9.8B projected by 2035) | Invest in cost-effective policies (e.g., salt reduction and tobacco control) and prioritize preventive care to reduce direct/indirect costs | [2] |
| Gaps in postacute care and specialized services | Strengthen virtual care infrastructure (e.g., Seha Virtual Hospital) and train healthcare professionals in CVD management and rehabilitation | [62, 64] |
| Low public awareness of CVD risks and prevention | Launch culturally adapted awareness campaigns via media, religious institutions, and community partnerships to promote heart-healthy behaviors | [120] |
mHealth is a mobile approach to health peppering and has held great promise in CVD prevention and management with patient-centered, timely care. Zhao et al. conducted a study to make out the different mHealth strategies available and assess their common practice application. Literature available on this topic, however, lacks standard metrics that can be referred to measure the engagement, feasibility, acceptability, and usability of mHealth interventions. Little has also been reported regarding the design and development processes of such interventions. Next-generation mHealth should entail advanced technologies in AI, machine learning, and augmented reality for increased effectiveness. It should also include cost-effectiveness studies necessary for policymakers to embrace mHealth. Infodemiology, the study of information-seeking behaviors online for health, is central to its effective enhancement of public access to quality information. The research set out to fill these gaps and further operationalize the mHealth strategies for CVD prevention and treatment [145]. The lack of a consistent approach to evaluating the success of mHealth interventions in Saudi Arabia is a critical missing element in current research. This gap is a critical obstacle to evaluate the efficacy and impact of mobile health interventions in the Saudi healthcare system. To overcome this challenge, future research may seek to design and implement more comprehensive evaluation frameworks specific to the Saudi context. These models should include quantitative and qualitative indicators, such as user engagement, health outcomes, cost-effectiveness, and patient satisfaction. Furthermore, researchers may consider adopting global mHealth assessment tools such as the mERA checklist and tailoring them to Saudi Arabia’s specific cultural and healthcare context. By implementing common measures, stakeholders will better monitor the effectiveness of mHealth initiatives, compare different interventions, and ultimately promote evidence-based decision-making in the Kingdom’s burgeoning mobile health technology landscape. Novel approaches and therapies in the struggle against CVDs are very stringent. RNA-based treatments, including messenger RNA and small interfering RNA, have proven to be effective in reducing LDL cholesterol in ongoing trials [146]. Gene editing techniques, particularly CRISPR-Cas9, are under research to rectify genetic mutations responsible for hereditary CVDs [147]. Moreover, advanced biomaterials are used in the form of better stents and bioresorbable scaffolds for trying to ensure better outcomes for procedures related to CAD [148].
8. Conclusion
The CVDs present a major health challenge in Saudi Arabia, which is further aggravated by the fast process of urbanization and change in lifestyle. Corresponding multimodal strategy-effective pharmaceutical interventions should be proposed, including measures that are preventive in nature, such as healthcare reforms that would be all-inclusive according to National Vision 2030. This will require overcoming some obstacles such as therapy nonadherence or socioeconomic inequalities. CVD prevalence can be significantly reduced, and results improved with better patient education, effective public health campaigns, and healthcare facilities. Such tailored interventions will subsequently be needed, informed by local epidemiological data, if the burden of CVDs is to be reduced and cardiovascular health promoted in Saudi Arabia.
Ethics Statement
The author has nothing to report.
Consent
The author has nothing to report.
Disclosure
The author confirms that this is an original manuscript and has not been previously published or submitted to another journal.
Conflicts of Interest
The author declares no conflicts of interest.
Author Contributions
Aseel Awad Alsaidan took sole responsibility for study conception, design, data collection, analysis, interpretation of results, and manuscript preparation.
Funding
This research was funded by the Deanship of Graduate Studies and Scientific Research at Jouf University through the Fast-Track Research Funding Program.
Open Research
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.