The Influence of Integrated Care Coupled With Intermittent Pneumatic Compression on Postoperative Rehabilitation Results in Ankle Fracture Patients
Abstract
Objective: To explore the effects of integrated nursing combined with intermittent pneumatic compression (IPC) intervention on postoperative recovery in patients with ankle fractures.
Methods: Seventy-two patients with ankle fractures who underwent surgical treatment at the Third Hospital of Hebei Medical University from July 2021 to October 2023 were selected and randomly assigned to two groups: 36 patients in the Routine care group and 36 patients in the IPC group. Postsurgery, the Routine care group received standard traditional nursing care, while the IPC group received integrated nursing coupled with IPC intervention. Pain levels, ankle joint function, incidence of complications, psychological state, and quality of life were assessed and compared between the two groups following intervention.
Results: Following the intervention, the IPC group reported lower pain levels compared to the routine care group; ankle joint function scores and range of motion were superior in the IPC group; the incidence of complications was reduced in the IPC group relative to the routine care group; levels of anxiety and depression were diminished in the IPC group; and the IPC group enjoyed a higher quality of life compared to the routine care group.
Conclusion: Postoperative integrated nursing combined with IPC intervention for patients with ankle fractures effectively alleviates pain, enhances ankle joint function, and reduces complications, while also positively impacting patients’ psychological well-being and overall quality of life.
1. Introduction
Ankle fractures, a prevalent category of bone injuries, constitute approximately 10% of all such injuries, with their incidence steadily increasing in recent years [1]. These fractures frequently result in damage to the distal syndesmotic ligament complex, leading to joint instability; consequently, surgery is a commonly employed treatment [2]. Presently, the dominant surgical approach is open reduction and internal fixation, which facilitates nearly perfect anatomical realignment of the ankle joint postoperatively [3]. Nevertheless, research reveals that even with an impeccable anatomical reduction achieved through surgery, over 20% of patients experience less-than-optimal improvement in ankle function, 30%–40% endure pain lasting beyond three months postoperatively, and nearly half of the patients face various complications, including deep vein thrombosis (DVT) [4, 5]. This often results in significant inconvenience in the patients’ daily lives and exacerbates the already considerable socio-economic burden [6]. Consequently, a series of timely interventions is frequently necessary postoperatively to promote patient recovery, although the ideal postoperative rehabilitation strategy for ankle fractures remains a subject of debate [7].
Nursing serves as an essential complement to clinical medical practice, with nurses significantly contributing to enhancing patients’ postoperative clinical outcomes and quality of life through a range of proactive and effective interventions [8]. Preventing venous thromboembolism (VTE) postsurgery is a crucial aspect of routine postoperative care, with intermittent pneumatic compression (IPC) being a common intervention employed to improve blood circulation and prevent DVT [9, 10]. This is primarily due to IPC’s inflation and deflation cycles, which facilitate the periodic emptying of deep veins, and its systemic impact on blood coagulation and fibrinolysis, thereby stimulating fibrinolysis [11]. Furthermore, substantial evidence indicates that IPC is effective in enhancing joint mobility in patients [12].
Comprehensive nursing encompasses the assessment of the patient’s physical condition, provision of holistic care, attention to both physical and psychological health, alleviation of suffering, eradication of negative attitudes, and enhancement of patient confidence [13]. Comprehensive nursing interventions embody a multifaceted, multidisciplinary approach, including health education, dietary guidance, exercise intervention, medication treatment, and other measures to support patients in achieving better recovery and a swift return to normalcy in work and life [14, 15]. Research suggests that comprehensive nursing interventions postsurgery positively impact the reduction of postoperative pain and enhancement of patients’ quality of life [16].
Thus, this study aims to explore the combined application of comprehensive nursing and IPC in patients with ankle fractures postsurgery, investigating the effects of this combination on postoperative recovery, with the objective of offering insights to improve ankle joint function and the overall quality of life for these patients.
2. Patient Information and Methods
2.1. General Patient Information
A cohort of 72 patients, who underwent surgical intervention for ankle fractures at the Third Hospital of Hebei Medical University between July 2021 and October 2023, was selected for this study. They were assigned sequentially and randomly to either a Routine care group or an IPC group, each comprising 36 individuals. The inclusion criteria were: (1) x-ray or CT imaging confirming ankle fractures; (2) surgical indication; (3) signed informed consent from both the patient and their family; (4) clear consciousness and effective communicative abilities; (5) normal auditory and visual functions. Exclusion criteria included: (1) open fractures; (2) old or pathological fractures; (3) severe cardiovascular or cerebrovascular conditions; (4) other significant injuries; (5) blood coagulation disorders; (6) severe osteoporosis; (7) psychiatric disorders; (8) severe functional impairment of the lower limbs. The IPC group comprised 22 males and 14 females, aged 38–52 years, with a mean age of 45.15 ± 3.43 years; 21 had left ankle fractures, and 15 had right ankle fractures; AO classification: 6 type A, 17 type B, 13 type C; Danis–Weber classification: 11 type A, 12 type B, 13 type C; the disease duration ranged from 23 to 28 days, with a mean duration of 25.31 ± 1.14 days. The Routine care group included 25 males and 11 females, aged 35–54 years, with a mean age of 45.53 ± 4.02 years; 24 had left ankle fractures, and 12 had right ankle fractures; AO classification: 8 type A, 19 type B, 9 type C; Danis–Weber classification: 14 type A, 13 type B, 9 type C; the disease duration ranged from 22 to 27 days, with a mean duration of 25.19 ± 1.24 days. No statistically significant differences were found between the two groups in terms of general data (p > 0.05). This study received approval from the Ethics Committee of the Third Hospital of Hebei Medical University, and written informed consent was obtained from all participants. The study adhered to the principles of the Declaration of Helsinki.
2.2. Nursing Methods
2.2.1. Routine Care Group
The Routine care group received standard nursing interventions, including routine ECG monitoring, vigilant observation of vital signs, and supplemental low-flow oxygen to ensure airway patency. For patients with drainage tubes, careful management was provided to prevent tube kinking, and surgical incisions were meticulously monitored. Any indications of bleeding were promptly reported to the attending physician, and dressing changes were carried out as required.
2.2.2. IPC Group
The IPC group received an integrated care approach in conjunction with IPC intervention. The comprehensive care approach included: (1) Addressing the psychological impact of ankle fractures, such as anxiety and depression, by developing personalized care plans that alleviate psychological burdens, actively listening to patient concerns, building trust, and enhancing treatment confidence through success stories. Maintaining a clean, well-ventilated environment, adjusting room temperature for comfort, and ensuring the cleanliness of bed linens were emphasized to prevent environmental discomfort. (2) Tailoring dietary recommendations to individual preferences and nutritional needs, promoting the intake of protein, vitamins, and calcium-rich foods, and advocating for a light, easily digestible diet to prevent constipation. (3) Closely monitor fluctuations in the patient’s vital signs, including body temperature, heart rate, and respiratory rate. For those patients presenting with swelling, blisters, fever, or pain in the affected limb, conduct comprehensive and corresponding examinations. Postsurgery elevate the affected limb to a height of 15–20 cm above the heart level. Regularly measure the circumference of the affected limb. Educate patients that ankle swelling may persist for several months but will gradually resolve through normal blood circulation, thereby alleviating their anxiety. In the event of blister formation, patients should refrain from self-puncturing. Instead, after thorough disinfection, use a syringe to carefully puncture the blisters, drain the fluid, and then ensure the affected area remains dry. Apply cold compresses using a wet towel wrapped around ice cubes to avoid direct contact of ice with the skin, which could cause additional damage. Administer anti-infective medications precisely as prescribed by the physician. Closely observe and meticulously document the degree of swelling, skin temperature, color, sensory perception of the affected limb, as well as the pulsation of the dorsalis pedis artery. If a patient exhibits pronounced pain and swelling in the lower limb, significant calf tenderness, dark red discoloration of the lower limb skin, and a positive straight leg ankle dorsiflexion test, and DVT is confirmed via lower limb deep vein ultrasound, elevate the affected limb 20–30 cm above the heart level. Assist the patient in turning over regularly to prevent prolonged pressure on any single area. Instruct the patient to avoid strenuous physical activities and massaging the affected limb to prevent potential thrombus detachment. Administer anticoagulant and thrombolytic drugs strictly according to the doctor’s prescription, adhering to the correct dosage and schedule. Actively engage in communication with the patient, gain an in depth understanding of their psychological state, and offer timely psychological support and counseling. Immediately report to the attending physician any occurrence of joint pain or toe traction pain experienced by the patient. Conduct a comprehensive assessment of the patient’s pain. Explain to the patient the pros and cons of using analgesics after surgery. The advantages involve pain relief, reduction of stress response, and improvement of rest and sleep quality, while the disadvantages include the risk of addiction, potential masking of the underlying condition, and the likelihood of adverse reactions. For patients with severe pain, administer analgesics as directed. In cases where the pain is mild, encourage patients to endure the discomfort through willpower. (4) Postsurgery, patients were assisted in maintaining a supine position for at least 5 h, with vigilant monitoring of vital signs. Patients and their families were instructed to abstain from food for 6 h postsurgery, elevate the affected limb 30 cm, and regularly inspect the incision dressing for dryness and cleanliness. (5) Evaluating patients’ conditions comprehensively to formulate individualized rehabilitation plans, adhering to a principle of gradual progression, avoiding overtraining, and controlling exercise intensity and duration, such as ankle and toe movements and walking practice with crutches for those in better physical condition.
IPC intervention involved: positioning the patient supinely and fully relaxing the limbs, followed by the application of the Air wave pressure therapy system (ShenZhen Pumen Technology Co., LTD). The lower limb was inserted into the sleeve, and air was inflated sequentially from the distal to the proximal compartments. After all compartments were inflated, automatic deflation occurred, with a brief interval before the process was repeated. The pressure was gradually increased to the patient’s comfort level. The entire treatment session lasted 20 min and could commence on the day of surgery, administered twice daily.
All patients received 10 days of hospital care and were advised to continue relevant care at home with family support. Follow-up was conducted 1 month postsurgery.
2.3. Observational Indicators
2.3.1. Pain Intensity
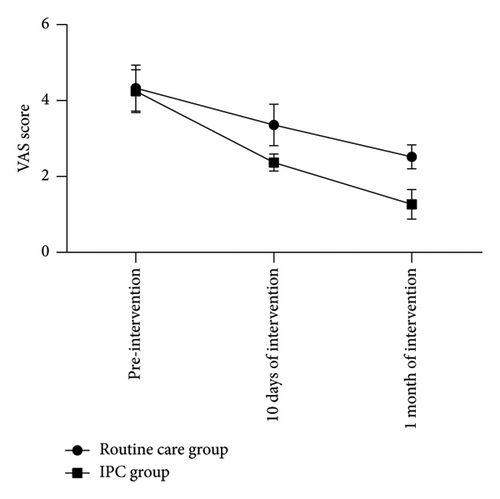
The severity of pain experienced by patients was gauged utilizing the Visual Analog Scale (VAS) prior to intervention, at the 10-day mark, and after one month of intervention. A higher VAS score denotes increased pain severity.
2.3.2. Ankle Joint Function
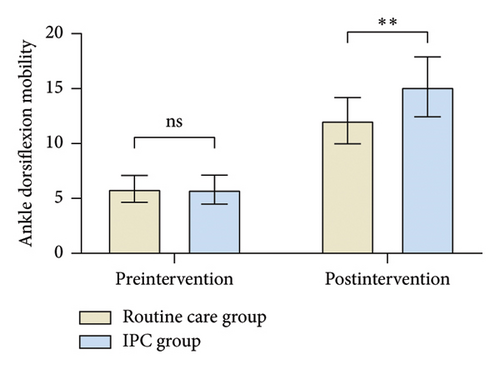
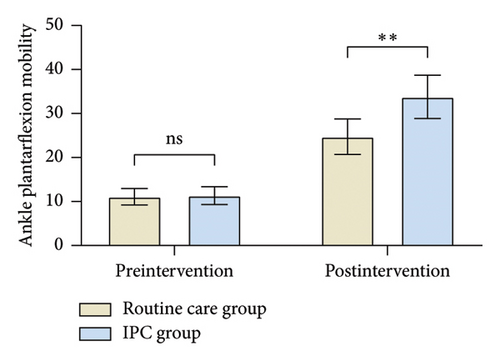
Ankle joint function in both patient groups was appraised employing the American Orthopedic Foot and Ankle Society Ankle-Hindfoot Scale (AOFAS-AHS) before the intervention and following a month. The total score can reach up to 100, with elevated scores indicating improved ankle joint recovery. Additionally, patients were instructed to lie supine with their legs extended, and a goniometer was employed to measure the dorsiflexion and plantarflexion angles in both groups to evaluate the range of motion of the ankle joint.
2.3.3. Incidence of Complications
The occurrence of complications such as DVT, wound infections, or other adverse events during the intervention period was meticulously documented.
2.3.4. Psychological State
The psychological state of patients was assessed before the intervention and after 1 month utilizing the Self-Rating Anxiety Scale (SAS) and the Self-Rating Depression Scale (SDS). SAS scores of ≥ 50 and SDS scores of ≥ 53 denote the presence of anxiety and depression, respectively, with higher scores indicating greater severity of anxiety and depression.
2.3.5. Quality of Life
Quality of life was appraised using the Generic Quality of Life Inventory-74 (GQOLI-74) both prior to the intervention and after one month. The evaluation encompasses four domains, including social and physical functions, with scores ranging from 0 to 100. Elevated scores signify an improved quality of life.
2.4. Statistical Methods
Statistical analyses were conducted utilizing SPSS 25.0 and GraphPad Prism 9.0 software. Measurement data are presented as mean ± standard deviation ( ± s), with intergroup comparisons performed using the independent samples t-test. Categorical data are reported as frequencies and percentages, with intergroup comparisons made using the χ2 test. A p value of < 0.05 was deemed statistically significant.
3. Results
3.1. Comparison of Pain Levels in Patients
Prior to the intervention, the VAS score for patients in the routine care group was (4.33 ± 0.61), whereas the IPC group recorded a score of (4.25 ± 0.56), with no statistically significant difference observed between the two groups (p = 0.564). Following 10 days of intervention, the VAS score for the routine care group decreased to (3.36 ± 0.54), while the IPC group’s score fell to (2.37 ± 0.22). Both groups exhibited a reduction in VAS scores relative to preintervention levels, with the IPC group demonstrating markedly lower scores than the routine care group (p < 0.05). One month postintervention, the VAS score for the routine care group was (2.52 ± 0.32), and for the IPC group was (1.27 ± 0.39). The VAS scores in both groups had diminished compared to preintervention and 10 days postintervention, with the IPC group consistently showing significantly lower scores than the routine care group (p < 0.05) (Table 1, Figure 1).
| Groups | Preintervention | 10 Days postintervention | 1 Month postintervention |
|---|---|---|---|
| Routine care group (n = 36) | 4.33 ± 0.61 | 3.36 ± 0.54∗ | 2.52 ± 0.32∗# |
| IPC group (n = 36) | 4.25 ± 0.56 | 2.37 ± 0.22∗ | 1.27 ± 0.39∗# |
| t | 0.560 | 10.187 | 14.867 |
| p | 0.564 | < 0.05 | < 0.05 |
- Note: Compared to preintervention within the same group, ∗p < 0.05; compared to the intervention at 10 days within the same group, #p < 0.05; data are expressed as ( ± s).
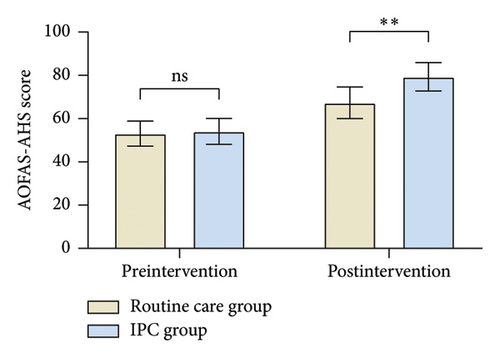
3.2. Comparison of Ankle Joint Function in Patients
Before the intervention, the range of dorsiflexion for the routine care group was (5.88 ± 1.21), plantarflexion range was (11.09 ± 1.86), and the AOFAS-AHS score was (53.10 ± 5.82). In the IPC group, dorsiflexion range was (5.81 ± 1.32), plantarflexion range was (11.35 ± 2.03), and the AOFAS-AHS score was (54.11 ± 5.99). No statistically significant differences were found between the two groups regarding AOFAS-AHS scores and the ranges of dorsiflexion and plantarflexion (dorsiflexion range: p = 0.815; plantarflexion range: p = 0.573; AOFAS-AHS score: p = 0.471). After the intervention, the dorsiflexion range for the routine care group increased to (12.09 ± 2.11), plantarflexion range to (24.75 ± 4.04), and the AOFAS-AHS score to (67.36 ± 7.29). For the IPC group, dorsiflexion range was (15.17 ± 2.73), plantarflexion range was (33.78 ± 4.91), and the AOFAS-AHS score was (79.34 ± 6.53). All measures of AOFAS-AHS scores and ranges of dorsiflexion and plantarflexion were significantly higher postintervention compared to pre-intervention, with the IPC group achieving superior outcomes compared to the routine care group (p < 0.05) (Table 2, Figure 2).
| Groups | Dorsiflexion range of motion | Plantarflexion range of motion | AOFAS-AHS score | |||
|---|---|---|---|---|---|---|
| Preintervention | Postintervention | Preintervention | Postintervention | Preintervention | Postintervention | |
| Routine care group (n = 36) | 5.88 ± 1.21 | 12.09 ± 2.11∗ | 11.09 ± 1.86 | 24.75 ± 4.04∗ | 53.10 ± 5.82 | 67.36 ± 7.29∗ |
| IPC group (n = 36) | 5.81 ± 1.32 | 15.17 ± 2.73∗ | 11.35 ± 2.03 | 33.78 ± 4.91∗ | 54.11 ± 5.99 | 79.34 ± 6.53∗ |
| t | 0.235 | 5.356 | 0.567 | 8.521 | 0.726 | 7.345 |
| p | 0.815 | < 0.05 | 0.573 | < 0.05 | 0.471 | < 0.05 |
- Note: In comparison to the preintervention values within the same group, ∗p < 0.05; data are presented as ( ± s).
3.3. Comparison of Patient Complication Rates
During the intervention period, one patient in the IPC group suffered from an incision infection, resulting in a complication rate of 2.78%. Conversely, the Routine care group experienced two cases of ankle joint stiffness, three cases of DVT, and three cases of incision infection, leading to a complication rate of 22.22%. The complication rate in the IPC group was markedly lower compared to the Routine care group (p = 0.033) (Table 3, Figure 3).
| Groups | Incisional infection | Joint rigidity | Deep vein thrombosis | Complication rate |
|---|---|---|---|---|
| Routine care group (n = 36) | 3 (8.33) | 2 (5.56) | 3 (8.33) | 8 (22.22) |
| IPC group (n = 36) | 1 (2.78) | 0 (0) | 0 (0) | 1 (2.78) |
| X2 | 4.571 | |||
| p | 0.033 |
- Note: The data is presented as n (%).

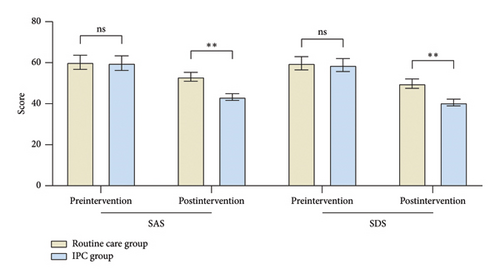
3.4. Comparison of Patient Psychological Status
Prior to intervention, the SAS score for patients in the Routine care group was (60.22 ± 3.42), and the SDS score was (59.75 ± 3.22); for the IPC group, the SAS score was (59.81 ± 3.57) and the SDS score was (58.86 ± 3.15). The differences in SAS and SDS scores between the two groups before intervention were not statistically significant (SAS score: p = 0.620; SDS score: p = 0.240). Following the intervention, the SAS score for patients in the Routine care group was (53.16 ± 2.18) and the SDS score was (49.81 ± 2.31); for the IPC group, the SAS score was (43.28 ± 1.62) and the SDS score was (40.59 ± 1.65). Both SAS and SDS scores decreased postintervention in both groups, with the IPC group demonstrating significantly lower SAS and SDS scores compared to the Routine care group (p < 0.05 for both) (Table 4, Figure 4).
| Groups | SAS score | SDS score | ||
|---|---|---|---|---|
| Preintervention | Postintervention | Preintervention | Postintervention | |
| Routine care group (n = 36) | 60.22 ± 3.42 | 53.16 ± 2.18∗ | 59.75 ± 3.22 | 49.81 ± 2.31∗ |
| IPC group (n = 36) | 59.81 ± 3.57 | 43.28 ± 1.62∗ | 58.86 ± 3.15 | 40.59 ± 1.65∗ |
| t | 0.498 | 21.826 | 1.186 | 19.487 |
| p | 0.620 | < 0.05 | 0.240 | < 0.05 |
- Note: In comparison to the preintervention values within the same group, ∗p < 0.05; data are presented as ( ± s).
3.5. Comparison of Patient Quality of Life
Before intervention, the social functioning score for the Routine care group was (60.03 ± 3.43), the psychological functioning score was (63.27 ± 3.57), the material life status score was (64.09 ± 2.66), and the physical functioning score was (63.18 ± 2.43); for the IPC group, the social functioning score was (60.23 ± 3.52), the psychological functioning score was (63.95 ± 3.28), the material life status score was (64.72 ± 2.83), and the physical functioning score was (64.08 ± 2.56). Comparisons of these GQOLI-74 scores between the two groups before intervention showed no statistically significant differences (social functioning score: p = 0.808; psychological functioning score: p = 0.403; material life status score: p = 0.334; physical functioning score: p = 0.131). After intervention, the social functioning score for the Routine care group was (82.15 ± 3.82), the psychological functioning score was (78.83 ± 4.01), the material life status score was (81.29 ± 3.87), and the physical functioning score was (79.53 ± 3.62); for the IPC group, the social functioning score was (90.47 ± 4.12), the psychological functioning score was (88.65 ± 4.53), the material life status score was (64.72 ± 2.83), and the physical functioning score was (90.03 ± 3.81). All GQOLI-74 scores improved postintervention in both groups, with the IPC group attaining superior scores across all GQOLI-74 domains compared to the Routine care group (p < 0.05 for all) (Table 5, Figure 5).
| Groups | Social function | Psychological function | Material living conditions | Physical function | ||||
|---|---|---|---|---|---|---|---|---|
| Preintervention | Postintervention | Preintervention | Postintervention | Preintervention | Postintervention | Preintervention | Postintervention | |
| Routine care group (n = 36) | 60.03 ± 3.43 | 82.15 ± 3.82∗ | 63.27 ± 3.57 | 78.83 ± 4.01∗ | 64.09 ± 2.66 | 81.29 ± 3.87∗ | 63.18 ± 2.43 | 79.53 ± 3.62∗ |
| IPC group (n = 36) | 60.23 ± 3.52 | 90.47 ± 4.12∗ | 63.95 ± 3.28 | 88.65 ± 4.53∗ | 64.72 ± 2.83 | 89.65 ± 4.22∗ | 64.08 ± 2.56 | 90.03 ± 3.81∗ |
| t | 0.244 | 8.885 | 0.842 | 9.739 | 0.973 | 8.760 | 1.530 | 11.987 |
| p | 0.808 | < 0.05 | 0.403 | < 0.05 | 0.334 | < 0.05 | 0.131 | < 0.05 |
- Note: In comparison to the preintervention values within the same group, ∗p < 0.05; data are presented as ( ± s).

4. Discussion
Ankle fractures, being relatively prevalent orthopedic injuries, demonstrate favorable therapeutic outcomes when managed surgically, facilitating the restoration of anatomical alignment and preserving the integrity of the distal syndesmosis ligamentous complex [17]. Prompt postoperative interventions are pivotal in optimizing patient recovery and reinstating normalcy in both daily life and occupational activities [18]. This study, which amalgamates comprehensive nursing with IPC for postoperative rehabilitation in patients with ankle fractures, reveals that routine care, when complemented by IPC intervention, significantly alleviates pain, enhances ankle joint functionality, diminishes the incidence of complications, and fosters improvements in psychological well-being and quality of life.
Postoperatively, persistent pain remains a predominant and recurrent complaint among patients, markedly affecting their daily activities [19]. This discomfort is attributable to factors such as the fracture itself, inflammatory mediators, and the surgical procedure, potentially leading to extended hospital stays, restricted and delayed mobility, prolonged bed rest, diminished adherence to physical therapy, and heightened postoperative complications [20]. During postoperative care, appropriate interventions can proficiently manage pain, ensuring patient comfort and facilitating the restoration of physiological functions [21]. Comprehensive nursing delivers a more standardized and targeted service beyond routine care, proving exceptionally effective in managing various disease-related pains [22]. Numerous studies have proposed that IPC intervention operates through cyclic inflation and deflation, skillfully emulating the natural processes of muscle contraction and relaxation. This emulation effectively stimulates blood circulation, mitigates blood stasis, and decreases the concentration of inflammatory factors, potentially offering notable relief for patients’ pain [23]. In the present study, while patients were undergoing the combined treatment of comprehensive nursing and IPC intervention, nurses meticulously conducted a thorough pain assessment. Based on the assessment results, they implemented well-considered pain management strategies. Postintervention analysis revealed that these patients exhibited significantly lower scores on the VAS compared to those who received only routine nursing. This outcome carries substantial clinical significance. From the patients’ standpoint, a reduced VAS score indicates a marked reduction in the pain they experience. This not only substantially enhances their comfort but also bolsters their confidence in the treatment and improves their compliance. Consequently, patients are more likely to actively engage in subsequent rehabilitation programs. Moreover, the successful pain alleviation achieved by integrating comprehensive nursing with IPC intervention presents a novel and efficient pain management paradigm for the clinical care of ankle fracture patients. It broadens the spectrum of pain management approaches and elevates the overall standard of nursing services.
Although surgical intervention can restore anatomical alignment in ankle fractures, patients frequently fail to achieve satisfactory recovery of ankle joint function in the immediate postoperative period [24]. This may be related to intra-articular damage resulting from the fracture or issues such as reduced tibiofibular overlap, tibial inclination, and fibular widening [25, 26]. Comprehensive nursing vividly reflects the patient centered nursing philosophy. With meticulous attention to each patient’s unique circumstances, nurses craft customized physical training regimens that are precisely tailored to meet individual needs. This training effectively curtails muscle atrophy, sustains muscle function, and enhances joint stability, positively influencing bodily function in patients with ankle fractures [27]. IPC, through mechanical pressure applied to the muscles, alleviates muscle spasms, mitigates nerve stimulation, decreases sympathetic activity, augments blood flow, and enhances muscle volume, thereby improving joint range of motion [28]. After receiving comprehensive nursing combined with IPC intervention in this study, patients showed a significant increase in both ankle function scores and ankle range of motion compared to those who only received routine nursing. This indicates that patients can resume their normal life and work earlier, thereby enhancing their independence and self-sufficiency in daily life. Simultaneously, the combination of comprehensive nursing and IPC intervention offers a novel and effective model for improving the prognosis of patients with ankle fractures. It enriches the content of nursing practice for ankle fracture patients and propels the advancement of their rehabilitation process.
Patients with ankle fractures may encounter a range of complications. On one hand, fractures can lead to cartilage loss, bone remodeling, and degenerative changes, while on the other hand, surgical intervention may result in postoperative wound infections and DVT [29]. Comprehensive nursing, recognized as a cutting edge nursing paradigm, revolves around the nursing process. It methodically weaves together crucial stages like assessment, diagnosis, planning, implementation, and evaluation [30]. Within the scope of this study, nurses carried out thorough and painstaking assessments. Through these efforts, they were able to gain an in depth and accurate understanding of patients’ medical circumstances, emotional well-being, and daily routines. Based on this comprehensive knowledge, individualized nursing plans were crafted for each patient. Throughout the nursing journey, nurses adhered rigorously to the pre-established plans. They executed a diverse array of nursing interventions, encompassing wound care, pain alleviation, rehabilitation coaching, and psychological encouragement. Moreover, they promptly conducted evaluations and made appropriate modifications as needed. This systematic and well-orchestrated approach to nursing guarantees that every facet of patient care is not only precise but also highly effective. As a result, it significantly elevates the overall quality of nursing services. When it comes to the tangible impact on patients, comprehensive nursing has the potential to optimize patients’ prognoses, expedite the restoration of their physical capabilities, and minimize the incidence of complications [31]. Additionally, IPC, a widely utilized clinical measure for thrombosis prevention, has exhibited commendable preventive effects against DVT [32]. In the context of this research, patients undergoing the combined intervention of comprehensive nursing and IPC witnessed a notably lower incidence of complications, including DVT and wound infection, compared to those who received only routine nursing care. From the patients’ vantage point, this reduced complication rate translates into a swifter recovery process. Patients can bid farewell to the hospital earlier, with their medical expenses substantially cut down, leading to a much-improved treatment experience. Simultaneously, the integrated approach of comprehensive nursing and IPC intervention presents a novel and potent nursing model for staving off complications in ankle fracture patients. It broadens the horizons of prevention strategies and enriches the toolkit of measures dedicated to keeping complications at bay for these patients.
Comprehensive nursing, hailed as an avant-garde nursing ideology and practice paradigm, is dedicated to delivering all-encompassing, scientifically-grounded, professionally-executed, holistic, empathetic, and tailor made nursing services to patients [33]. This model transcends the mere treatment of physical illnesses; it places a strong emphasis on a comprehensive understanding and care of the patients’ overall well-being. Within the framework of this research, when implementing comprehensive nursing, nurses are tasked with harmoniously integrating nursing theory, hands on nursing skills, and the pursuit of high quality care. This integration compels nurses to delve deeply into nursing theoretical knowledge and deftly apply it in real-world nursing scenarios. As a result, they can constantly refine their nursing proficiency, enabling them to offer patients nursing services of an even higher caliber. By adopting this approach, nurses can more effectively navigate the entire landscape of nursing work, enhancing both the efficiency and the quality of their caregiving endeavors. By implementing nursing management systems, standardizing medical team responsibilities and philosophies, and employing a comprehensive set of clinical nursing methods, comprehensive nursing provides extensive care for patients’ physical and psychological states, alleviating negative emotions such as anxiety and stress, and significantly enhancing quality of life [34]. In the present research, patients who underwent the combined intervention of comprehensive nursing and IPC experienced remarkable enhancements in their psychological state and quality of life, outperforming those who received only routine nursing care. The amelioration of the psychological state empowers patients to confront the illness and the arduous rehabilitation journey with a more upbeat mindset, thereby heightening their subjective sense of well-being. The upswing in the quality of life manifests in patients’ improved capacity to engage in daily living activities. They exhibit greater self-sufficiency in taking care of themselves and are more actively involved in social interactions. Simultaneously, the findings of this study offer robust empirical support for the innovation and evolution of nursing models. They act as a driving force, propelling the nursing discipline forward towards a future where the holistic health of patients takes center stage.
Undoubtedly, this study is not without its limitations. Firstly, it is a single-center research with a relatively small sample size. Only 72 patients were recruited, which inevitably casts doubts on the generalizability and applicability of the findings. Further investigations are required to determine the efficacy of the combined intervention of comprehensive nursing and IPC in a more extensive population of ankle fracture patients. Secondly, the study’s observation period was short. Given that ankle fracture rehabilitation is a protracted process, numerous complications and functional recovery outcomes may only surface during long-term follow-up. This study failed to evaluate the long-term effects and safety of the combined comprehensive nursing and IPC intervention, making it difficult to accurately gauge the sustained impact of this model throughout the patients’ rehabilitation journey. Consequently, the research findings are somewhat one-sided. Lastly, due to the current absence of standardized protocols for comprehensive nursing, some aspects of this study may not be readily transferable to other hospitals, thus constraining the practical application of the results.
In summary, the combination of routine nursing and IPC intervention has demonstrated remarkable positive effects on the postoperative rehabilitation of ankle fracture patients. It alleviates pain, enhances ankle joint function, reduces the incidence of complications, improves patients’ psychological well-being and quality of life, and effectively promotes their overall recovery. Therefore, we advocate for its widespread adoption and promotion in clinical settings. In clinical practice, healthcare providers should deepen their understanding of the combined routine nursing and IPC intervention, master the operational techniques and precautions proficiently, and deliver high quality, effective nursing care to ankle fracture patients. Moreover, hospitals and relevant authorities should develop appropriate training programs and quality control standards to ensure the standardized implementation of this intervention, thereby elevating the quality of clinical nursing and benefiting a larger cohort of ankle fracture patients.
Ethics Statement
This study has been reviewed and approved by Ethics Committee of the Third Hospital of Hebei Medical University, bearing the ethics approval number: W2021-053-1.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
M.Z. and J.L. contributed to the conception and design of the study. C.L. and S.L. performed the data collection and analysis. Y.L. and S.L. contributed to the interpretation of the data. M.Z. and Y.F. drafted the manuscript. All authors critically revised the manuscript for important intellectual content and approved the final version to be published. Mo Zhang and Yekun Fang contributed equally to this work and should be considered co-first authors.
Funding
This study was funded by the Effect of Comprehensive Intervention on Postoperative Swelling in Patients with ankle Fracture (No: 20211422).
Acknowledgments
The authors have nothing to report.
Open Research
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.