Introducing a Computerized Care-Pathways System for Older Adults in Home-Care Settings
Abstract
Introducing computerized care pathways for older adults living at home may be a promising way to improve the clinical dimension of integrated care. Evidence on how to implement them in various home-care contexts is, however, sparse. A prospective, comparative multiple case study with nested analysis units was conducted across three home-care settings. Participants included managers, healthcare professionals, and home-care clients. We used a variety of frameworks and both qualitative and quantitative methods to understand the implementation process. The implementation research logic model (IRLM) presents links among determinants, strategies, mechanisms, and outcomes. Twelve barriers and 35 facilitators were similarly perceived, and 40 strategies were commonly adopted during implementation. After 12 months, OCCI implementation was feasible, appropriate, and acceptable at moderate-to-high levels. They were delivered with a moderate level of fidelity, but the level of penetration after 24 months was high. Participants perceived the OCCIs as supporting a holistic approach, good relationships, clinical decision-making, information sharing, and interprofessional coordination, but not as much productivity and efficiency. Home-care clients had a high level of satisfaction with health care and services. They were satisfied about their involvement in decision-making and with computer use by professionals. We identified four causal pathways: engaging interest holders in a partnership model throughout the study; providing an information system that supports clinical processes; building a conducive environment with deliberate efforts to increase buy-in and engagement; facilitating capacity and relationship building to increase adoption; and embedding the OCCIs in usual practice. The results illustrate how a real understanding of contexts was important to elucidate the mechanisms at work during this study. Adapting the innovation to achieve a better fit between it and the clinical contexts was fundamental. Positive outcomes relied on time, appropriated resources, and a continual, iterative process corresponding to “Make It Happen.”
1. Introduction
Over the past 20 years, the province of Quebec, Canada, has been faced with a rapid increase in its aging population and the proportion of older adults experiencing complex interrelated health and social needs that threaten their ability to manage their everyday life [1–3]. Because of their needs, they require a system in favor of integrated care (IC), which facilitates prompt access to community supports, social services, and health care, while eliminating delays, redundant assessments, inadequate information transfer, and inappropriate resource utilization [4–7]. IC can be defined as methods and models on the funding, administrative, organizational, service delivery, and clinical levels designed to create connectivity, alignment, and collaboration within and between the healthcare system (on the primary, secondary, and tertiary levels) and social services with the aim of improving quality of care, consumer satisfaction, and system efficacy for patients with complex, long-standing problems that cut across multiple services, providers, and settings [8, 9]. In the last 25 years, numerous models for organizing IC for older people or people with chronic conditions have been developed and used in different parts of the world [10–13]. However, they greatly varied due to their application in contexts differing in eligibility criteria, levels, domains, types of integration, and finance mechanisms [10, 14–17]. In fact, no one IC model seems best suited to all contexts, settings, and circumstances [14, 18]. Their evaluation studies were also heterogeneous in methodology, and assessments of effectiveness remained mixed. For now, the evidence suggests that IC contributes to better outcomes such as improvement in quality of life, well-being, patient satisfaction, caregiver burden, and resource utilization such as increased access, reduced hospital or emergency admission, and lengths of hospital stay, but the evidence regarding other outcomes is unclear [10–13, 19–22].
Even though there are many models and studies on the topic, it seems that the success of IC systems depends on the ability of all local interest holders to adapt to their new roles and adopt management and clinical tools appropriate to their new tasks. Several factors are frequently reported to influence the spread and scale-up of IC models. They include a change of culture with clinical and management leadership, regulation aligned with services provided across the continuum of care, adequate funding, dedicated time and resources, information and communication technology (ICT) to facilitate communication, physicians’ and healthcare providers’ engagement, effective communication strategies, feedback loops, and a continuous monitoring system [19, 20, 23–25].
Many authors also point out that the patient’s perspective and quality of care should be at the heart of any discussion about IC [13, 14]. Patient-centered care considers the viewpoint of the client by ensuring that services are well coordinated around their needs. Full and accurate information about a patient’s needs and care must be available throughout the care journey to everyone involved, including the patient themselves, using patient portals, and providing them online access to their electronic health records (HERs) [26–28]. This information should be accessible from anywhere in the health system. Nevertheless, even though we possess extensive evidence regarding the factors that facilitate the implementation of IC, we still need a deeper comprehension of their working mechanisms, ideally supported by implementation theories [19, 29].
In Quebec, one ministry already administers all social and healthcare services. Following the positive impacts highlighted by IC projects carried out in our province in the 2000s [6, 30], service integration has since been the central theme of the actions taken by our system to ensure that older adults will remain at home for as long as possible with well-coordinated primary care, health-related services, and support from home care and community-based services (HCBSs) [6, 30–34]. The priority was given to planned and formal coordination at the legislative, administrative, organizational, and clinical levels [33], and components such as local mechanisms for coordination with a single entry point, multidisciplinary teams, comprehensive assessments with care plans introduced in a health information system (HIS), patient empowerment, and case management were gradually implemented for community-dwelling frail older people [15, 32]. However, although IC has gradually been embedded in our health and social care system, some gaps associated with needs assessment, planning, and service coordination have remained [31, 34–36]. In fact, providers have considered that government policy and mergers have strongly influenced the implementation of organizational and functional dimensions of integration to the detriment of clinical integration [35, 37, 38]. According to these authors, healthcare providers considered that the system was focused on providing services rather than needs and that shared decision-making with clients and caregivers was difficult to implement, although person-centered care was a central principle promoted by their organizations. They also suggested that additional efforts were needed to improve the HIS named the RSIPA (2009 version; French acronym for “Réseau de services intégrés pour les personnes adultes”) and its interoperability. Indeed, task-oriented service delivery frequently overlooked the need for psychosocial services [39, 40]. Similar to other systems, we have also observed some issues related to fall prevention, nutritional needs, and the identification of at-risk older adults [41, 42].
Given these challenges, it has become important to find new ways of working to better assess, support the needs, and improve our IC model for home-care clients. Integrated care pathways (ICPs) have been introduced in many settings as a strategy to reduce variations in care by improving adherence to recommended best-care practices [43, 44]. ICPs are also a way to improve coordination of care, multidisciplinary and professional–patient communication, and patient satisfaction [45–47]. Minimally, ICPs are complex interventions based on an assessment with a care planning process that is supported by multidisciplinary teamwork. They structure care around individual needs, combine evidence-based key interventions, and provide feedback on the current care process, like many interventions based on assessment instruments used in home care [48, 49]. However, ICPs are more than that as they emphasize the follow-up of patient-focused care, which includes the monitoring and evaluation of variances and outcomes in real-time [50]. Variance analysis enables the identification of discrepancies between anticipated and actual care, thereby facilitating adjustments to the plan or services to ensure they adequately meet needs [51]. Variance data can enhance systems and clinical practices and aid in the planning of health service delivery [52]. ICPs have been used for over 30 years to improve the quality of care and maximize care outcomes for specific groups of users [43, 53]. However, they are more common in acute care sectors or for unique clinical situations (e.g., stroke) rather than for clientele with complex interrelated health and social needs requiring the expertise of multiple care providers and services [54–57]. In a study comparing various care processes with and without care pathways in hospitals, they found that in around 75% of the cases, a care pathway led to better organized care processes [43]. However, the literature lacks detailed information about the implementation and evaluation of computerized ICPs or similar interventions for frail older adults with multiple needs who are living at home in the context of IC [57, 58].
For now, in common with IC or comprehensive geriatric assessment (CGA), we know that ICP implementation requires robust ICT with combined strategies to address potential barriers. Studies also showed that adequate staffing, professional collaboration, and continuous training are important facilitators to their implementation [49, 59]. One important feature is interoperability between the various ICT systems that necessitate large investments into HER [59]. A review of 77 studies on IC for older people in different settings found that no more than 36 of them were ICT-based IC models and that only 33% of them used HER [21]. Some digital solutions that support communication and data sharing among professionals, such as PROCare4life, tested in six European countries, seem promising but still need significant refinements before being embedded in their health and social care [60].
For professionals, ICPs may also be burdensome because of added documentation, compliance requirements, and communication among multidisciplinary teams [59]. In return, well-designed interoperable, HER systems with predictive algorithms may reduce omissions, enhance care coordination, and enable professionals to intervene much earlier [59, 61]. Other professionals also feel that ICPs may inhibit their judgment in practice and damage their autonomy [62]. But using real-time data from patients and advanced digital analytics may support the shared decision-making process and help find a balance between standardization and personalization through close monitoring of personalized delivery processes and real-time feedback [59, 63].
All these considerations have been appraised when developing ICPs specifically designed to better address the complex chronic needs of frail older adults living in the community. Referred to as Outils de Cheminement Clinique Informatisés (OCCIs for computerized care-pathway systems), they are a promising, innovative way to improve the clinical dimension of service integration [64, 65]. The OCCIs are an extension to a prior research program on IC programs for older adults with disabilities living in a community-based IC network (program on research for integrating services for the maintenance of autonomy [PRISMA]) [6, 66] and diagnoses provincial needs [64]. They consist of a standardized comprehensive assessment and structured multidisciplinary care plans, made with the older person’s or a family member’s input and expectations. These are part of a core decision-support system that tells you what to do in a given clinical situation and then analyzes variations to help you find the best solution for the needs of adults living in the community. They were developed to facilitate communication and support clinical and management processes in home-care services and across the continuum of services. Based on Quebec’s “healthy aging” model—which takes account of all the intervention factors and strategies intended to maintain or improve the health of older persons [67]—the OCCIs included relevant overlapping concepts such as person-centered care, reablement, and proactive care with identification of at-risk older adults.
When the OCCIs were being developed, their inclusion in a HIS was quickly recognized as a key component of their successful use. To this end, the information technology branch of the ministry (DGTI/MSSS) (Direction Générale des Technologies de l’Information du MSSS) integrated them into their computerized clinical and management solution referred to as the RSIPA [68]. This process led to an improved solution—the RSIPA (2016 version). Subsequently, the provincial Ministry of Health and Social Services (MSSS) (French acronym for Ministère de la Santé et des Services sociaux) decided to support a multisite project to test and refine the RSIPA and to determine whether the OCCIs could be a solution to establishing efficient practices. However, the OCCIs are based on components like comprehensive assessment, person-centered care, and e-health technology, for which several known factors could act as obstacles and hinder their implementation [45, 69–71]. Introducing them into home-care standard practices is likely to introduce several changes that could affect clients or their caregivers, professionals, and managers. It is therefore imperative to evaluate these potential changes since many regions in the province have expressed a strong interest in using them.
According to Greenhalgh et al. [72], the OCCIs constitute an innovation in the organization of health services as they bring new clinical, organizational, and technological practices. By measuring the three main stages of OCCI implementation—preimplementation, implementation, and innovation sustainment—we can better inform implementation strategies and explain implementation outcomes, as well as possibly increase their transferability. So, the main goal was to look at how the OCCIs could be used in the right way in the real world, like in home care settings, in providing insight into determinants, strategies, mechanisms, and outcomes of the implementation processes. We also explored whether rolling out the OCCIs was an effective way to support managers and professionals in their work to improve the response to the needs of older adults in the context of IC. In this way, we investigated both services (e.g., quality of clinical decision-making) and client outcomes (e.g., satisfaction).
This multiple case study with mixed methods aimed at conducting a process evaluation to understand what worked, how, and why in OCCI implementation across the three designated home-care settings. The implementation research logic model (IRLM) was used to present and link determinants, strategies, and outcomes in identifying plausible causal pathways [73]. These aims responded to the concerns expressed by the decision-makers and managers associated with this project. Moreover, the findings provided a firmer foundation for future implementation throughout the province of Quebec.
- 1.
How do determinants facilitate or impede OCCI implementation?
- 2.
What strategies are applied to promote OCCI implementation?
- 3.
What are the implementation outcomes?
- 4.
How are OCCI outcomes perceived by managers and healthcare professionals?
- 5.
How are OCCI outcomes perceived by the clients of home-care services?
- 6.
What are the links and plausible causal pathways between determinants, strategies, and outcomes?
2. Methods
2.1. The Quebec Health and Social Service System
Since 2015, the province of Quebec has been divided into 16 regions with 22 functional structures. They include 13 CISSSs (Health and Social Service Centres; French acronym: CISSS for Centre intégré de santé et de services sociaux) and 9 CIUSSSs (Integrated University Health and Social Service Centres; French acronym: CIUSSS for Centre intégré universitaire de santé et de services sociaux) to ensure accessibility, continuity, and quality of services for people in their territory (Act respecting Health Services and Social Services (chapter S-4.2, s. 99, available at https://www.legisquebec.gouv.qc.ca/en/home). Each center had five types of services: CH: hospital center; CHSLD: residential and long-term care center; CLSC: local community service center; CPEJ: child and youth protection center; and CR: rehabilitation center. The 22 CISSSs/CIUSSSs report directly to the MSSS and had to develop strategic partnerships with community and private organizations in their new territories. They are responsible for organizing, managing, and delivering all public health and social care to their local populations. Each center provides home-care services for people with disabilities and older adults through their local community health and social centers (French acronym: CLSC for Centres locaux de santé communautaires). Some services are also available to their family members and caregivers. After a common standardized assessment, clients may receive professional services (such as from nurses, social workers, occupational or respiratory therapists, physiotherapists, and dieticians) and nonprofessional services (such as support for activities of daily living [ADLs]). Community and private organizations in the same territory provide services such as meal preparation, meals-on-wheels, housekeeping, and transportation. Care and services are coordinated by case managers or a main provider, depending on the clinical complexity. The process of client assessment and care planning is supported by different tools included in the secure web platform (RSIPA), which has been available online for health professionals since 2005 [74, 75].
2.2. Description of the Innovation
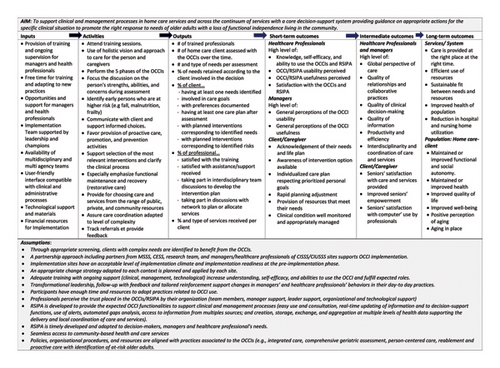
We provide a brief description of the OCCIs here. They consist of five clinical phases [64, 65, 68], and more details are provided in the Additional file 1 using the Template for Intervention Description and Replication (TIDieR) checklist [76]. The various components are summarized under the Logic Model of the OCCIs, which graphically describes the underlying assumptions, planned work, and intended results of this innovation [77] (see Figure 1). Basically, the first phase is a needs assessment that documents the source and causes of the client’s needs, what is most important for them and their caregivers, and the identification of risk factors that must be identified to reduce disabilities. Supported by algorithms, the second phase depicts the concise clinical situation and supports the shared decision-making process in which the client’s priority needs and the goals to be reached in care-plan development and implementation are determined. In the third phase, considering the identified goals, the system proposes interventions based on evidence-based practices. Thus, in agreement with the recipient, the expected pathway appropriate for the clinical situation and expectations of the client and caregivers is produced in a personalized care plan. At the fourth phase, the completed pathway supports the documentation of coordination and service delivery. The final phase involves identifying and analyzing variances or gaps, along with the reasons behind them, to support the necessary plan review and adjustment. At the beginning of this study, the computerization of Phases 4 and 5 had not been completely finalized in the system. During the implementation of OCCI, these phases will continue to be developed using a participatory design (PD) that includes end users and people with an interest [68, 78].
2.3. Study Design
The study design consisted of a comparative multiple case study with nested analysis units. It uses both qualitative and quantitative methods and a prospective evaluation approach in three home-care settings [79, 80]. A comparative case study is useful for examining causality, particularly when understanding the context is crucial for assessing the intervention’s success or failure [81]. This methodology allows for using multiple data sources and methods in order to consider a multiplicity of perspectives, levels of decision-making, and analysis over the time frame of the intervention, as well as to capture complex relationships among contexts, processes, and outcomes of the intervention [79]. Three CISSSs/CIUSSSs (Sites A, B, and C anonymized), from different regions in Quebec, were selected because of their successful collaborations and their potential to respond quickly to the technological changes associated with this project. Each setting was a distinct case, and we use the term case and site interchangeably. The number of cases was limited to three to ensure that each case was studied in enough detail, while considering the short time frame and the available financial resources. Overall, each site delivers home care within the existing governance of the Quebec healthcare system and has the same structure as several public establishments. The cases were purposely selected using theoretical replication logic. They present contrasting specificities in terms of the number and size of the organization given their territorial and population characteristics and modes of delivery (see Table 1). The OCCI implementation, as observed in each case, was the phenomenon under study. It took place over a 24-month period and included three phases: preimplementation (i.e., teaming, initiation, and planning—about 3 months); during implementation (i.e., execution with monitoring—0 to 12 months); and postimplementation (i.e., end of the implementation with outcomes and sustainment—12 to 24 months). The design is consistent with the IRLM, which guides our in-depth investigation of the links among determinants, strategies, and outcomes in order to identify plausible causal pathways over time [73]. Lastly, a monitoring committee—including some representatives of the DGTI/MSSS, the Sherbrooke health expertise center (French acronym: CESS for Centre d’Expertise en Santé de Sherbrooke), the research team, project managers, and some healthcare professionals from the selected sites—was also established for the duration of the study.
| Cases—CISSSs/CIUSSS | Site A | Site B | Site C |
|---|---|---|---|
| Type of area | Semi-urban | Semirural | Highly urban |
| Population | 213,000 | 247,049 | 225,698 |
| Speaking | Mainly French | Mainly French | Mainly English |
| % aged 65 or older | 14% | 17% | 16% |
| Territory | 1346 km2 | 4756 km2 | 132 km2 |
| Living in rural area | 13% | 33% | — |
| # of employees | 2681 | 4330 | 2202 |
| # of hospital | 1 | 1 | 1 |
| # of CHSLD | 3 | 13 | 1 |
| # of CLSC | 3 | 5 | 2 |
| Inhabitant density | 158/km2 | 53/km2 | 1710/km2 |
| Implementation level of RSIPA 2009 before the study | 73% | 84% | 75% |
| Who do the first OEMC | Rapid assessment team | Most often social workers or occupational therapists | Most often social workers or nurses |
| Service with the longest waiting list | Nutrition | Occupational therapist and physiotherapist | Occupational therapist |
2.4. Analysis Units and Participants
The research team initially contacted, by telephone, the three CISSSs, who agreed to participate in this study. We provided them with preliminary information about the study and invited them to share details about the served population and structural characteristics of their institutions. Level 1 consisted of employees in management roles, such as high- and mid-level leaders or those supporting the implementation (referred to as managers herein). Level 2 included healthcare professionals (i.e., nurses, social workers, occupational and respiratory therapists, physiotherapists, and dieticians) likely to use the OCCIs. We invited everyone involved in the study’s implementation to participate. The number of managers and professionals varied per site, depending on the method of data collection and the scope of the planned project deployment at each site. Before each qualitative data collection, participants first received information on the study procedure, data protection, and anonymization, and they provided informed consent prior to their participation in the study. When we used self-report questionnaires, potentially eligible participants received an initial email from management alerting them to the upcoming questionnaire. They then received an individual email outlining the study’s objectives, instructions, and links to the online questionnaire. Completion of the questionnaire via the platform constituted their consent to participate in the study. We sent a reminder 2 weeks later to those who did not complete the questionnaires. We offered them an extension period. Level 3 consisted of a sample of home-care clients who had been assessed with the OCCIs and exposed to computer use during their assessment at home. We randomly selected 10 elders, family members, or caregivers per site to represent different levels of functional autonomy based on Iso-SMAF profiles. They had to speak and understand French. Caregivers were considered in situations in which home-care clients were unable to respond to the interview or in situations in which they wanted to participate with the elder. The list of identified persons was provided by professionals at each site who obtained clients’ consent to be contacted by a research team member. Written informed consents were obtained before the interviews, which were held in client homes. All measures to ensure confidentiality and establish a relationship of trust with clients and their families who agreed to participate were taken. We ensured confidentiality by replacing nominal information with codes. An institutional convenience process was obtained for each site, and the study was approved by the CISSS Chaudière-Appalaches Research Ethics Board (MP-23-2016-343, MP-2016-016) in May 2016. This board acts as the main evaluator for the multicenter research project. The decision of this main board also applied to the other two centers.
2.5. Overall Data Collection Process and Analysis
We first present the general process of data collection and analysis. Then, the specific methodological considerations associated with each research question are detailed in the next section, 2.6. Table 2 presents a summary of the data collection methods according to each research question and implementation phase (see the end of Section 2.5). To guide the data collection and analysis process, we applied different theoretical frameworks or models according to each research question. Data collection included quantitative and qualitative methods with different sources to inform the implementation process and outcomes over the study. We carried out the collection in the same manner at each site, but sequentially, one site after the other, a few months apart. The study started in 2016 at one site and then at the beginning of 2017 at other sites. The implementation process at the three sites finished at the end of 2017. We received the final databases containing the OCCIs data completed during the study for all the home-care clients from the baseline to the postimplementation phase (24 months) in 2019. These data were encrypted and stored on the network of the Research Centre on Aging of the CIUSSS Estrie—CHUS. Nominative information was coded to preserve anonymity.
| Data collection methods | Concepts and framework, model, or taxonomy | RQ |
|---|---|---|
| Preimplementation phase (≈3 months before implementation) | ||
|
|
#1 |
|
|
#1 |
|
|
#1 |
|
|
|
|
|
|
|
|
#1 |
| During implementation (0–12 months) | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| End of implementation phase (12–24 months) | ||
|
|
|
|
|
|
|
|
|
Each data collection method was designed based on the literature review, adapted to the target audience (managers (M) and healthcare professionals (P)), and pilot tested. The quantitative and qualitative data collected from the various sources were first processed and analyzed given equal weightage, then merged in the interpretation stage (when necessary) and linked to each research question after each phase. For each question, a summary of all data sources with three separate descriptive case study reports was built.
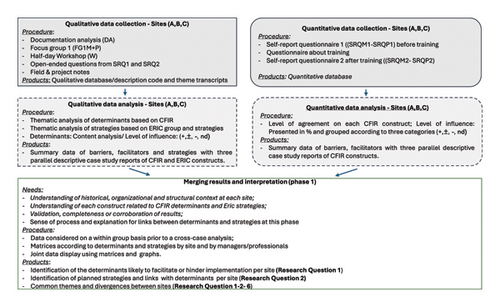
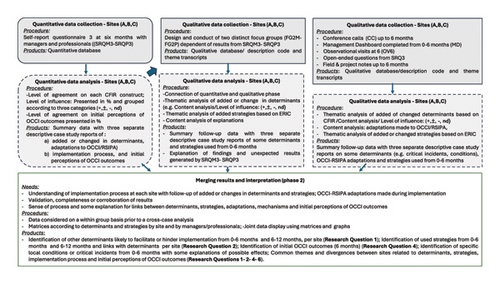
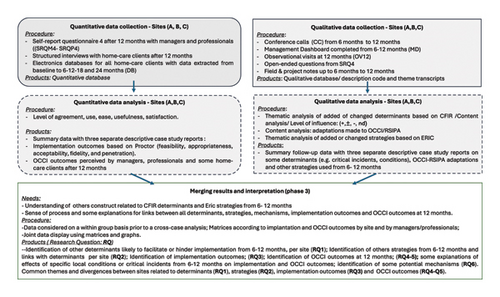
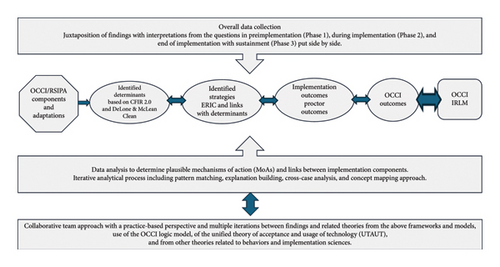
Figures 2, 3, 4, and 5 schematize and describe the analysis process, which allowed us to answer each research question within each phase (see Figures 2, 3, 4, and 5 after Table 2, before Section 2.6). We developed a case study database using Microsoft Excel to manage and organize all data collection and analysis [79]. Concerning quantitative methods, they included Likert-scale questionnaires used in internet Lime surveys or in-person interviews distributed at various times during the study. We also used the data coming from an anonymized electronic database containing the OCCIs data completed during the study for all the home care clients. To develop the questionnaires, we chose questions from validated instruments that have been shortened due to the limited time available for participants to respond and to minimize respondent fatigue (see Table 2). Questions were prioritized based on relevancy to cover selected frameworks or models, and the wording was adapted specifically to the context of OCCI implementation. Descriptive statistics were used to analyze quantitative data using IBM SPSS Statistics 24. Responses to each question from structured questionnaires were grouped and presented in percentages according to their constructs and the scale used (e.g., level of agreement, frequency, and so on). Bivariate analyses were performed, including some nonparametric statistical tests because of the small number of participants at two sites. Specifically, as an example, Fisher’s exact test was used to evaluate the relationship between two categorical variables, while the Mann–Whitney U test or the Kruskal–Wallis test was used for continuous variables. We tested the differences in perceptions between each site. We analyzed the open-ended questions and optional comments at the end of the questionnaires along with all the qualitative data. We presented the quantitative results as tables with their respective themes and constructs across sites, considering the type of participants (managers or professionals). We also graphically displayed the results in various colors to facilitate the analysis and understanding both within and between sites.
Qualitative methods included document analysis, focus groups, interactive workshops, conference calls, management dashboards, observational visits, and open-ended questions. All the conversations were audiotaped, and they were transcribed verbatim by the experienced research coordinator. Next, we conducted a hybrid process of inductive and deductive thematic analysis, drawing inspiration from Braun and Clarke [89]. We first developed a code manual that included detailed definitions according to each framework or model selected and adapted to the specific context of the study. A senior research assistant experienced in qualitative studies (CC) conducted the qualitative data analysis by reading each transcript and the field notes for familiarity with the data. The assistant developed preliminary codes and subthemes manually using both inductive and deductive approaches (open coding and coding of theoretical constructs). Major themes were then mapped to the selected framework or model. The codes that did not fit in a framework were evaluated and reconsidered. A research team member (ND) independently reviewed a random selection of about one-third of the transcripts. The research team discussed discordant coding until they reached a consensus (CC, AN, ND, and NDC). Consistent with Braun and Clarke [89], the inclusion was based on the extent to which the theme contributed to expanding knowledge to answer research questions, not just occurrences within the data. The first member sometimes checked the findings and interpretations with the study participants. Systematic and iterative reading and coding allowed for findings focused on research questions. To support the cross-case analyses, the data were organized in Word and Excel documents using matrices broken down according to the specific constructs associated with each research question, the targeted adopter type when available (managers/professionals), and by site [90]. Representatives’ quotes for each of them were manually selected. Peer debriefing and reflexive writing throughout the coding process were carried out. A reflexive journal was used to keep track of emerging impressions of what the data meant, how the data related to each other, or to follow the decision trail. Regular research meetings were held to discuss codes that did not seem to fit into the main themes, discrepant data, or inadequacies in the initial coding.
Finally, depending on the research question, we used a side-by-side display that juxtaposes quantitative results with related qualitative results and evaluated convergence, complementarity, and expansion to support integration, understanding, and interpretation of both types of data [91].
2.6. The Specific Methodological Considerations Associated With Each Research Question
- •
Research Question 1: How do determinants facilitate or impede OCCI implementation?
- •
Research Question 2: What strategies are applied to promote OCCI implementation?
-
We assessed determinants and strategies both before and during the implementation process (0–6 months; 6–12 months). One method for comprehending determinants is the Consolidated Framework for Implementation Research (CFIR 1.0) [95]. Commonly referred to as “barriers” and “facilitators,” determinants may also be utilized to direct the choice of strategies to get past obstacles and make the subsequent implementation easier [96]. To capture the determinants, we started this study using the original CFIR 1.0 [95]. But by the time our analyses and preliminary manuscripts were finished, the updated CFIR version 2.0 was published, which was based on user feedback and more recent literature [97]. We decided to review our data with the CFIR 2.0 as it clarified and added several concepts. Apart from the intervention characteristics domain, which is now known as the innovation domain, all five of the updated CFIR’s domains have additional constructs and subconstructs that were useful to better describe our data. The use of “recipients” rather than “patients,” and “deliverers” for all those involved in providing the innovation were among the few changes made to each domain and construct overall. It now includes five domains with 48 constructs and 19 subconstructs: (1) Innovation domain refers to the perceptions of OCCI features, including their clinical and technological contents (RSIPA); (2) outer setting domain is the feature of external context in which our CISSS/CIUSSS are embedded, i.e., the healthcare and social services system with its policies, including the MSSS; (3) inner setting domain refers to the characteristics of each setting named CISSS that houses the CLSCs in which the OCCIs were implemented; (4) individuals domain considers the different roles and characteristics of individuals such as managers and healthcare professionals; and (5) implementation process domain relates to the implementation strategies, including adaptations made during OCCI implementation (https://cfirguide.org/). Adaptations are any deliberate change made to the design or delivery of the OCCIs/RSIPA with the goal of improving fit or effectiveness or in reaction to unanticipated challenges arising in each context [98].
-
Implementation strategies can be defined as methods or techniques used to enhance the adoption, implementation, and sustainability of a clinical program or practice. The strategies outlined by each site were mapped to the Expert Recommendations for Implementation of Change (ERIC), which is a published compilation of 73 implementation strategy terms and definitions [99].
-
We used six methods of data collection in the preimplementation phase (see Table 2). (1) Documentation analysis permitted gathering information about the served population and the structural characteristics of their institutions. (2) Then, a focus group was conducted in-person by researchers and coordinators with key people in management roles or directly involved in planning or carrying out the future implementation at each site. The discussions focused on their current governance structures, project management methods (e.g., Lean methodology), organizational processes, clinical practices, and the type of usual support (clinical and technological) provided to clinical teams. (3) Shortly afterward, a computerized self-reported questionnaire (SRQ1) adapted to the target audience (managers (M) and healthcare professionals (P)) was sent to all potentially eligible participants. The questions aimed at finding out how the individual participants perceived their current work contexts; their practices, such as knowledge about assessment, planning, shared decision-making, patient-focused care, reablement, and prior interdisciplinary and intersectoral practices; and the tools used (e.g., OEMC, PSIAS) before becoming familiar with the OCCIs. (4) In a subsequent step, we organized a half-day workshop with the individuals directly involved in planning or carrying out the implementation at each site. One investigator conducted the focus group, supported by a coinvestigator who probed questions if necessary. The research coordinator recalled questions as needed and kept track of time. After a more detailed presentation of the OCCIs, we asked interest holders about initial perceptions of OCCI characteristics, in terms of how they could be of added value for them, healthcare professionals, and home-care clients. Then, we discussed issues related to each current context and further OCCI implementation. Based on all this information, they presented their ideas on the most promising strategies for their contexts and considered the maximum study duration. (5) Subsequently, a 2-day training session with formalized tools and methods was developed by the research team and the CESS according to the needs of all the sites. This team delivered and validated the training at the first site before offering it at the other sites. Each training session concluded with an assessment of satisfaction with its content, trainers, locations, organization, and learning. (6) Lastly, around 1 month after training, another self-reported questionnaire (SRQ2) was sent to each audience to document their knowledge and perceptions of the OCCIs, as well as their perceptions about their ability to use them.
-
During the implementation phase (from 0 to 12 months), five methods of data collection were used: (1) First, 6 months after implementation, a computerized self-reported questionnaire, SRQ3, tailored to each participant group, was fulfilled to cover mainly CFIR 2.0 determinants associated with the implementation process domain and some others about the relative advantage of the OCCIs. Since the OCCIs are integrated into an information system (IS), specific determinants, such as experience of users, system reliability, response time, information quality, and service quality, were considered [92]. (2) Consecutively, two distinct focus groups were conducted by two researchers and the research coordinator with participants directly involved in planning or carrying out the implementation and considered as having the most experience with the OCCIs. We began by presenting the results from the self-reported SRQ3M or SRQ3P questionnaire. This allowed us to start the discussion to determine whether they modified or added some strategies, if some events were crucial for local appropriation of the OCCIs, and what factors could explain the initial OCCI outcomes. (3) During the implementation process, a management dashboard was also completed by each site to report the difficulties encountered with the solutions adopted. (4) In parallel, regular conference calls were held between all partners, and a decision log that compiled all challenges and decisions regarding implementation was completed. (5) Two periods of field observation were carried out at 6 and 12 months to identify the conditions of OCCI use at each site. The observations were based on a template with specific indicators (e.g., availability or layout of workstations or technical information).
-
Concerning the analysis of determinants assessed with questionnaires, responses to each question were first grouped and presented in percentages according to three categories: disagree (strongly disagree, disagree), neutral (neither agree nor disagree), and agree (agree, strongly agree). To simplify the presentation of results, facilitate integration with qualitative data, and preserve the anonymity of sites and participant groups, each exact percentage was replaced with a plus sign (potentially positive effect on implementation), a minus sign (potentially negative effect), a plus-or-minus sign (potentially mixed effect), or nd (no data or question not asked of a category of participants). The item was considered as having a potentially positive effect (+) when more than 50% of participants (M = managers) or (P = healthcare professionals) agreed or strongly agreed with the statement. For example, under the Innovative relative advantage, if the statement “I recognize the advantage of using the OCCIs daily in my practice” gets 80% of agreement by managers, the percentage in the M column was replaced with +. The item was considered as having a potentially negative effect (−) when more than 50% of participants disagreed or strongly disagreed with the statement. Lastly, the item was considered as having a potentially mixed effect (±) when more than 50% of participants were neutral (neither agreed nor disagreed) about the statement or when none of the percentages were > 50%.
-
Regarding determinants assessed with qualitative methods, each code was reviewed to indicate whether it represented a potentially positive, negative, or uncertain/neutral influence represented by signs (+, −, or ±). During coding, the research coordinator periodically checked the interpretation with other members to ensure consistency of interpretation and guard against bias.
-
Finally, to facilitate linkages between all determinants and strategies, we confirmed links with the CFIR ERIC matching tool [100]. It contains 73 techniques organized into nine clusters available in an Excel-based matching tool, which allows users to input implementation barriers, defined by the CFIR, to receive recommendations about expert-recommended implementation strategies (ERICs) that might address these barriers (https://cfirguide.org/choosing-strategies/). See Figures 2 and 3 schematizing the process of data collection, analysis, merging results, and interpretation during these implementation phases.
- •
Research Question 3- What are the implementation outcomes?
-
Evaluation of implementation outcomes was based on the Proctor Implementation Outcomes Framework [101, 102]. They can be defined as the effects of intentional and purposeful actions to implement new practices or services and serve as indicators or markers of the implementation process and success. Furthermore, they are seen as essential conditions for achieving later intended improvements in clinical or service outcomes. We also considered some subconstructs associated with the usage of technology in ISs [103–105]. More specifically, we considered feasibility (i.e., the OCCIs can be successfully implemented, and it is simple to use them), appropriateness (i.e., compatibility for a given context and usefulness), and acceptability (i.e., satisfaction when using them). These outcomes were measured through a self-reported questionnaire, SRQ4, conducted after 12 months with managers and healthcare professionals (see Table 2).
-
Additionally, we considered penetration, sustainability, and fidelity, which were measured using anonymized data from the OCCIs completed in the RSIPA solution extracted from the baseline to the postimplementation phase (24 months). The extractions cover data from the clinical chart itself, i.e., all the forms that make up each record, plus the logging of data on daily entries and exits by professionals for modifications and consultations of these records. The chart comprised the CGA covering 6 domains with 16 major dimensions. There was also a specific module with a summary to support the structured decision-making process and care plans. Penetration is defined as the integration of a practice within a service setting and its subsystems. From a service perspective, this construct is like the reach of the RE-AIM frameworks [106] that is the coverage of the intended target groups, i.e., the number and characteristics of home-care clients assessed with the OCCIs. Sustainability is the extent to which a newly implemented intervention is maintained or institutionalized within a service setting’s ongoing, stable operations. It was measured as the evolution of the OCCIs completed once the field study had been completed (after 12 months) until 24 months. The outcomes of penetration and sustainability are related in that higher penetration may contribute to long-term sustainability. OCCI Fidelity is the degree to which the OCCIs were delivered as intended by OCCI developers. Fidelity has been measured typically in terms of adherence, dose, and quality of the program [68, 69]. Fidelity-Adherence measures the delivery of the key components of an intervention as it was designed (i.e., structure: the element is present). Fidelity-Dose refers to the specific amount of OCCI completed, which includes the number of assessments and care plans over the study period, ranging from 0 to 12 and up to 18 months. Fidelity-Quality measures the way providers deliver the OCCIs using the overall clinical process (the different OCCI phases and subcomponents) as attended by the developers (process). Here, it also includes the use of the RSIPA IS with the OCCIs integrated. To this end, we reviewed the content of the overall assessment and determined the prevalence of user care needs, preferences, and goals; their involvement in the goal-setting process; and the planning of services/interventions. It was impossible to link data from the RSIPA solution to the e-CLSC (SIC) database, so we could not estimate study services. Lastly, a total fidelity score was calculated. We scored each component as “yes” if conducted and “no” if not. We then calculated a percentage of the number of cases (observation or record) for which the component was scored as “yes” over the total number of observations conducted and records reviewed. Here, it also included the frequency of use of the OCCIs as perceived by the professionals (available in the SRQ4) (see Table 2).
-
Research Question 4- How are OCCI outcomes perceived by managers and healthcare professionals?
-
The service outcomes were judged by how well the OCCIs were thought up by participants to improve practices that were meant to meet the needs of older people in a network of IC services. We assessed them twice: once at six months (preliminary outcomes) using the SRQ3 and again at 12 months using the SRQ4 (see Table 2). The benefits include global perspectives, quality of relationships, quality of clinical decision-making, quality of information, productivity and efficiency, interdisciplinary coordination, and coherence. Global perspectives focus on a holistic approach to care that includes understanding client needs and difficulties, while the quality of relationships emphasizes trust and continuity. Collaborative practices involve multiple professionals working together with clients and their caregivers to deliver the highest quality care. Clinical decision-making relies on quality information, which is complete, accessible, and structured. This information is used to establish one or more diagnostic hypotheses and to subsequently verify, test, and confirm the final clinical decision. It reduces time, duplication, and paper usage while ensuring productivity and efficiency. Interdisciplinary coordination ensures effective collaboration between professionals, while coherence involves resource choice, timing, and professional contributions to achieve common objectives. Results from the conference calls, observational visits, and management dashboards were considered to understand results from SRQ4 (see Figure 3).
-
Research Question 5- How are OCCI outcomes perceived by the clients of home-care services?
-
At the end of the implementation, we also evaluated a sample of ten home-care clients with caregivers per site who had been assessed with the OCCIs and exposed to computers for at least 4 months. We randomly selected them to represent various Iso-SMAF autonomy profiles. Initially, many professionals were concerned about how clients would react to using a computer at home and whether this could harm the clinical process and their relationships with them. The goal of this investigation was to use preliminary results to rapidly determine clients’ perceptions of computer use by health professionals, the clinical process for identifying and meeting their needs during assessment and care planning, and if something needed to be adjusted.
-
Specifically, we interviewed clients in their homes using standardized questionnaires, similar to those used in previous IC studies [93, 94, 107–109], concluding with two open-ended questions. The dimensions of client outcomes were: (1) Satisfaction: (a) Satisfaction in the relationship with the healthcare professional with concerns about interpersonal relations (e.g., trust, courtesy); (b) satisfaction with services delivered with concerns about the way professionals deliver services, offer choices, give advice or information about available services, and so on; (c) satisfaction with the general healthcare organization related to the accessibility of services at convenient times, the ease in obtaining appointments with a professional, and so on. (2) Empowerment: This refers to (a) the client’s involvement in decision-making, such as their perception of being able to choose the type of care and services they need; (b) interaction, which refers to the process of obtaining information or assistance to meet their needs; and (c) the level of control, which refers to the recipient’s feelings about seeking explanations or advice. (3) Perceptions about the specific process of shared decision-making using the OCCIs; and (4) perceptions about the computer use by the professional during home visits. Open-ended questions provided insights into what clients and their caregivers thought about the process to identify and meet their needs and if they had encountered any problems during their episode of care and services that, in their opinion, needed improvement.
-
Research Question 6- What are the links and plausible causal pathways between determinants, strategies, and outcomes?
-
The IRLM [73] advances the traditional logic model for the requirement of implementation research and practice. It provides a means to describe the complex relationships between determinants, strategies, and mechanisms, leading to positive outcomes under a compact visual depiction of the implementation project. Mechanisms are processes through which strategies operate to affect their desired outcomes [110].
-
To facilitate interpretation and linkages, the potential mechanisms observed were mapped to the work of McHugh et al. [111] and the Behavior Change Technique Taxonomy V1 (BCTT) [112, 113]. The BCTT consists of 74 behavior change methods, including 26 mechanisms of action (MoAs) or theories explaining “how” the mechanism of action works. That therefore testifies as to “why” we can expect a causal link between application of the methods and behavior changes.
-
To identify possible causal pathways and synthesize all elements of the implementation under the IRLM, the various findings were examined in parallel (i.e., descriptive case study reports and matrices produced during the different phases of the study to answer the first five questions). To build explanations linking the various components, we used an iterative analytical process including pattern matching, explanation building, cross-case analysis, and a concept mapping approach. First, we used predetermined questions and hypotheses to look at all the data within and between sites. We then looked for certain factors or elements that seemed to be most responsible for certain outcomes (like a high, moderate, or low level of acceptability) based on a number of plausible theoretical mechanisms. “What were the strategies that occurred over time that have favored the OCCI fidelity?” or “How and why did this outcome occur or not, or in this way, in this site, but not in other sites?” are examples of questions.
-
We formulated the hypotheses using our OCCI logic model and the conceptual frameworks or models employed in this study. We also considered the unified theory of acceptance and usage of technology (UTAUT) [105, 114, 115] with its eight underlying theories (theory of reasoned action (TRA [116]), technology acceptance model (TAM [117]), motivational model (MM [117]), theory of planned behavior (TPB [118]), combined TAM-TPB [119], model of PC utilization (MPCU [120]), innovation diffusion theory (IDT [121]), and social learning theory [122]. For example, based on the UTAUT model, one hypothesis stated that if a person perceives an innovation as useful and simple to use, she will be more likely to use it. Moreover, positive social influence and support will strengthen their intention to use the innovation.
-
In certain situations, we found alternative factors or other combinations that could have produced the same or unintended results, and therefore, we conducted a literature review to describe and support these observed patterns. We have also thought about possible counterfactual explanations many times during interpretations, using frameworks, theories, literature reviews, and our practice-based view. We shared our analysis and interpretations with the wider research team to verify and discuss the selection of certain elements over others. To organize and capture all this information, we drew out in parallel possible common or diverging patterns through the cases using a graphical tool such as concept maps (CMapTools software) that illustrate relationships between all components using labels, nodes, boxes, and links [123]. Many concept maps were built, and several meetings with research members were held to check that concepts and links were adequately reflected. At this stage, it was often necessary to go back and forth to the literature and the cases to review some findings and interpretations. Thus, the maps were frequently revised, and several of them were connected under a plausible main pathway. When the maps were deemed good enough, the final step was to make them easy to understand, and we presented them in a logical way by telling a story about the most likely causal pathways. Lastly, the IRLM was completed to summarize the findings across sites and illustrate the relationships between determinants, strategies, mechanisms, and outcomes (implementation/services/home-care clients).
3. Results
3.1. Participant Characteristics
Tables 1 and 2 in the Additional file 2 show details in participation rates and sociodemographic characteristics of participants in response to quantitative questionnaires SRQ1 (before implementation), SRQ2 (after training), SRQ3 (6 months after implementation), and SRQ4 (12 months after). Overall, the managers involved in the project at the three sites returned participation rates from 81%–100% for SRQ1, 80%–100% for SRQ2, 78%–89% for SRQ3, and 70%–100% for SRQ4. The managers at the three sites were mostly women with a high level of education (29%–77% with a master’s degree) and a full-time job. They had nearly 20 years of experience in home-care services. The participation rates of the professionals ranged from 57%–95% for SRQ1, 60%–86% for SRQ2, 57%–100% for SRQ3, and 48%–100% for SRQ4. Most of the professionals had a bachelor’s degree; those at Sites A and B were more experienced than those at Site C.
The next section describes results according to each research question. To prevent recurrence of some findings, we underlined only the most relevant information for understanding the plausible underlying mechanisms leading to outcomes. A summary of results and links between specific determinants, strategies, mechanisms, implementation outcomes, and OCCI outcomes is illustrated through the IRLM see Figure 6 at the end of the results section.
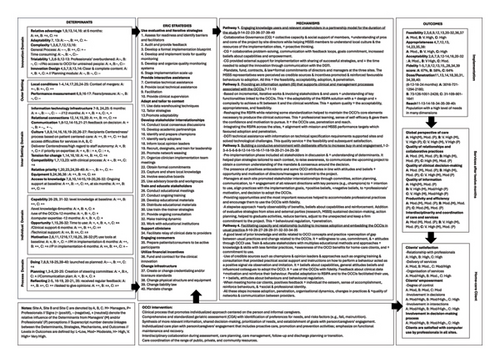
3.2. Research Question 1: The Determinants
Overall, the three sites perceived 35 facilitators and 12 barriers similarly, while each site perceived differently 38 other determinants. The barriers belonged more to the innovation domain, inner setting domain, and outer setting domain, while facilitators were linked to the implementation process domain and individuals domain. According to the CFIR 2.0 Framework Guidance, we briefly describe below each domain (in bold) with their constructs and subconstructs, which are the most significant (in italics). Detailed information on the identified determinants acting as facilitators or barriers during OCCI implementation can be found in the Additional file 3. The first column of the IRLM (Figure 6) also summarizes them.
Concerning the I. innovation domain, from the outset, the participants from all sites recognized that the OCCIs were evidence-based (I.B) and offered several advantages compared to past practices (I.C). In return, they considered them very time-consuming, complex, and lengthy (complexity, I.F.), and the care plans were not user-friendly (design, I.G.). Innovation Adaptability (I.D.) was a great concern before and during the study; several changes have been made to either the RSIPA solution or to the OCCIs. Additional file 4 shows these adaptations made according to the three phases of the OCCIs (assessment, synthesis, and planning).
Under the II. outer setting domain, local conditions (II.C), financing II.F), and performance pressure (II.G.3) were noted as barriers. The study highlights the negative impact of reform on health care (local conditions), including instability, but acknowledges the need for improvement, despite resource constraints and accessibility issues. All sites evoked fears about the performance targets linked to MSSS accountability (G.3. performance pressure). The MSSS assured project implementation would be considered without penalty, but 6 months later, managers remained concerned about reaching targets, but professionals did not perceive this pressure.
In the III. inner setting domain, sites shared numerous common facilitators, including effective collaboration to implement changes, the ability to solve clinical problems, and the appreciation of interdisciplinary and intersectional practices within and between teams/services (III.B relational connections). Sites have built on their existing working relationships and organizational units to seek consensus around their implementation decision to increase the commitment of all parties (III.D—Culture). Professionals were receptive to change (III.E. Tension for Change) despite the healthcare reform and resource restrictions (III.J.1 Available Resources—Funding). Professionals at Sites B and C recognized that the OCCIs were compatible with their clinical process (III.F. Compatibility).
On the other hand, there were significant organizational changes with significant turnovers of managers and professionals, exhaustion, overburden (III.A.3 Work infrastructure), and communication issues (III.C). The project faced IT infrastructure issues (III.A.2.) at Sites B and C, including data loss, system instability, and internet access issues, which were more prevalent at these sites than at Site A. After 12 months, most professionals at three sites considered establishing connections to the RSIPA or the internet acceptable. Site A found the funding (III.J.1) offered by the MSSS inadequate and did not consider OCCIs compatible (III.F) with their clinical process. All participants received the necessary training and clinical support (III.K. Access to knowledge), although it was less observed at Site C.
On the topic of IV. individuals domain, all sites also evidenced a good level of knowledge and self-efficacy with the various concepts and clinical processes targeted by the OCCIs (IV. Characteristics—B. Capability). After 6 months, all professionals expressed their confidence, expertise, and ability in using RSIPA functionalities and OCCI components. Nevertheless, they indicated that they still needed sessions to increase their knowledge and understanding of specific aspects (e.g., how to manage risk factors) (IV.A. Needs). The teams received necessary clinical and technological support, with an acceptable delay. However, they expressed ambivalence about sufficient time to assist with OCCIs usage (IV.C. Opportunity). After 12 months, all professionals demonstrated high confidence in using RSIPA functionalities for assessment, shared decision-making, and care planning, with Sites A and C experiencing difficulties with scales and plan generation (IV.B. Capability). Except for Site C, the good level of motivation (IV.D) observed among both managers and professionals has been a facilitator.
Under the V. process domain, many activities were accomplished in sequence from the preimplementation phase to the end of the study. Concerning deployment, only Sites B and C adopted a stepwise approach with small steps, obtaining some success before going to a larger deployment (V.G. Doing). A monitoring committee representing members of the MSSS, CESS, research team, project managers, and representatives from the selected pilot sites was formed and maintained for the duration of the study (V.A. Teaming). This committee allowed for discussion of the priorities, preferences, and needs of the interest holders at each site (V.B. Needs). All sites developed and followed their own action plans with strategies that varied little between sites, even if the observed barriers and facilitators were different (V.C. Assessing Context, V.D. Planning, and V.E. Tailoring Strategies). At all sites, the use of a steering committee with a project coordinator that tracked implementation via monitoring strategies allowed to ensure that the activities were carried out as planned (V.H. Reflecting and evaluating). During these meetings, they also involved champions and local opinion leaders from the clinical field in the hopes that they will influence colleagues to adopt the OCCIs (V.F. Engaging).
3.3. Question 2. The Implementation Strategies
Additional file 5 describes the implementation strategies that were linked to the CFIR determinants and mapped to the ERIC tool to facilitate analysis and interpretation. Through the 8 groups, 40 strategies were commonly adopted across all the sites. Most of them had been planned from the study’s outset. Their selection was based on managers experience with previous implementation projects in our healthcare system. Considering the different deployment approaches at the three sites, some strategies were used to varying degrees for a dozen of them. The highest number of strategies fell within the group of “develop interest holder interrelationships (12),” followed by “train and educate interest holders” (8) and “use evaluative and iterative strategies (6).” Four strategies were linked to “provide interactive assistance” and “change infrastructure.” Three were used to adapt and tailor the innovation to the context. There was only one strategy mapped in each group labeled “support clinicians,” “engage consumers,” and “utilize financial incentives.”
3.4. Question 3. The Implementation Outcomes Perceived by Managers and Healthcare Professionals
3.4.1. Feasibility
Overall, Site B found the OCCI components and the RSIPA functions easy to use, followed by Sites C and A (see Table 1 in Additional file 6). Ease includes the use of sections such as assessment, risk factor assessment, client and caregiver need information, professional analysis, recommendation, and disciplinary plans. Sites A and C professionals found it challenging to effectively utilize the health-status domain, psychosocial situation, and decision-making process. Except for those at Site C, none of the professionals found it easy to complete the interdisciplinary or services plans (compared to the disciplinary plan), or they did not complete them. Except for Site B, professionals from Sites A and C did not really appreciate using the scale and the automatic plan generation function.
3.4.2. Appropriateness
Managers at Site C were more likely than those at Sites B and A to agree that the OCCIs were useful for their teams (see Table 2 in Additional file 6). Apart from the interdisciplinary and services plans, all professionals considered all the above elements useful/very useful. Most RSIPA functionalities were considered useful by all participants, but professionals from Sites A and B did not find so useful functions such as “using scales,” “open all or close all,” “add/modify a group,” or “automatically generate the plan.”
3.4.3. Acceptability
Globally, professionals from Site B were very satisfied with almost all components, more so than those at Site C (see Table 3 in Additional file 6). The professionals at the three sites strongly appreciated the SMAF, the economic conditions, and physical environment domains in the assessment as well as the global expectations and capabilities/strengths sections in the synthesis. Conversely, professionals from Sites A and C were less satisfied with domains such as health status, psychosocial situation, and the use of risk factors.
3.4.4. Fidelity, Penetration (Reach), and Sustainability
Regarding fidelity dose and penetration, at baseline, the number of trained providers who delivered the OCCIs was higher at Site A (n = 72) than at Sites B (n = 13) and C (n = 10). Throughout the year, it increased very slowly to 87 at Site A, 15 at Site B, and 28 at Site C. After 12 months, deployment at all the sites was broad. The number of trained professionals increased in such a way that the number of OCCIs completed between 12 and 24 months rose sharply from 721 to 2180 at Site A, from 126 to 2428 at Site B, and from 109 to 1641 at Site C. From baseline to 12 months, the OCCIs were mostly used by nurses and social workers at Sites A (77%) and C (97%) compared to Site B (41%). Other professionals included occupational therapists, physiotherapists, and respiratory therapists. After 24 months, the proportion of nurses and social workers using the OCCIs increased to 84% at Site A and 78% at Site B but remained stable at Site C (96%).
Additional file 7 presents the characteristics of home-care clients assessed at each site with the OCCIs (Reach). After 18 months, 1074 clients at Site A, 986 at Site B, and 850 at Site C had at least one assessment completed. Briefly, we can confirm that this clientele had multiple complex needs. Around 60% of clients had moderate levels of disability (ISO-SMAF profiles 4 to 9). The proportion of clients with a low level of disability, requiring help mainly with domestic activities (profiles 1–3), was higher at Site A than at Sites B and C. As a result, the proportion of clients with a high level of disability (profiles 10–14) was greater at Sites C and B than at Site A. Clients in this category are often eligible to enter a nursing home since they usually require more than 3 hours of nursing care and assistance per day. Nearly half the clients were at moderate risk of malnutrition and about 10% at high risk. On average, about 8–12 needs were identified for the 16 clinical dimensions assessed. Care goals retained for care planning were frequently associated with ADLs and psychosocial situations. Some less prevalent needs at assessment, however, were chosen in care planning more frequently, such as special care, instrumental activities of daily living (IADLs), and economic conditions.
For fidelity, we first described the following clinical process (see Table 1 in Additional file 8): Nearly, all professionals consulted the client’s records in preparation for home visits. Except at Site A, most professionals documented this information in the OEMC before the visit. Professionals filled one OEMC on average per client per year. In some cases, the delay in obtaining a second assessment was about 5 months at Sites A and B, compared to 3 months at Site C. The professionals filled out all the assessments because they could not advance to the next phase without finishing all the sections. Professionals primarily generated the summary in the presence of the client, as they completed the assessment at the office. Almost all professionals discussed the prioritization of needs and care planning in the presence of the client or caregiver. Most home-care clients at all sites had at least one care plan after the first assessment. The delay between an assessment and a care plan was about 20 to 38 days in the first year, but it decreased at all sites in the second year (17 to 25 days).
During the care planning process, about half of the professionals participated in interdisciplinary discussions. The proportion of professionals participating in interdisciplinary discussions varied considerably when allocating services. Most of the care goals had at least one planned intervention. After 12 months, 5%–13% of goals were modified, with 24%–46% not achieved.
A fidelity score for adherence and quality was calculated, and Table 2 in Additional file 8 gives the details. Overall, the total score was slightly higher at Sites A and C than at Site B. In preparing for the assessment, only the professionals at Site A needed to improve the documentation of the OEMC before the home visit. They also needed to improve how to document difficulties with the drop-down during the assessment. In the synthesis, professionals at all sites should have learned how to transfer needs directly to the plan to save time and to complete the summary in the client’s presence. The loss of points in this phase was also attributed to the difficulty in retaining goals related to client care preferences, which might have been influenced by the available services. Despite not fully appreciating the PSIAS care planning module (French acronym: PSIAS for planification des services individualisés et d’allocation de services), most professionals successfully completed the necessary planning. The study found challenges in interdisciplinary and intersectoral practices, possibly due to the lack of interoperability within the ISs. After a year, professionals used the computer with the client at home frequently at Site B and moderately at Sites A and C, with connection, unsanitary environments, and speed issues being common reasons. There was also a sense that the computer acted as a barrier to the client’s relationship.
3.5. Question 4. The OCCI Outcomes Perceived by Managers and Healthcare Professionals
They were investigated after 6 and 12 months (see Additional file 9). After 6 months, we observed that the effects were quite moderate. A large percentage of Site B and C managers had a positive perception of using the OCCIs to support many practices, while their professionals often saw few benefits. According to professionals from Sites B and C, the enhanced OEMC provided a better understanding of the specific situation of the clients, helped to better identify their needs, and facilitated the collaborative practices between professionals and with home-care clients, as well as enabling them to make better clinical decisions. Additionally, they considered that it yielded a higher quality of information relevant to developing care plans. Conversely, at this moment, neither site agreed that the OCCIs could better guide clients across the continuum of services or produce benefits in terms of productivity and efficiency. In fact, even if it increased the time in the client’s presence, it also increased the time to complete records. Most professionals did not see any positive effects for many dimensions of practice; 30%–50% indicated that they did not observe positive effects (see Table 1 in Additional file 9).
After 12 months, the situation had greatly changed. Generally, for most dimensions of practice, Sites B and C managers and professionals strongly agree with OCCI benefits, while Site A professionals moderately agree. Most managers and professionals agreed that the OCCIs promoted a better quality of information relevant to service planning, a better understanding of the specific situation of clients, and a better definition of appropriate interventions and took more account of the contribution made by clients and by the public and community networks. The managers at Sites B and C had a more positive opinion than professionals about the quality of relationships and collaborative practices. Unlike managers, professionals at all sites did not agree that the OCCIs reduced errors and allowed a better exchange of information between professionals. Considering the productivity and efficiency dimension, the OCCIs seemed to reduce the repetitions, did not affect the delay between a request and the provision of service, and did not increase the volume of paper. In contrast, they did not reduce repeated calls between professionals but still increased the time required to complete client records. In terms of interdisciplinary and coordination, the managers at Sites B and C agreed that the OCCIs improved all aspects of this dimension. Those at Site C also agreed, but in a lower proportion according to subdomains. This site already had interdisciplinary issues before the study (see Table 2 in Additional file 9).
3.6. Research Question 5. The OCCI Outcomes Perceived by Home-Care Clients and Their Caregivers
This section concerns the preliminary results for the interviews with home-care clients on how they perceived the clinical process using the OCCIs and a computer during assessment. Site C had trouble recruiting 10 participants given the criteria that the client had to speak and understand French and be exposed to computer use during the assessment. Due to the small sample size and skew distributions, we have no power to detect any difference across sites. While the results must be interpreted with caution, they are nevertheless informative. Sociodemographic and clinical characteristics are provided in Table 1 (Additional file 10). The mean age varied per site from 73 to 85 years old. Almost 40% of elders had a good or very good perception of their general health status, while 33% did not have the capacity to answer that question. A proportion of 13% of clients had a low level of disability (i.e., Iso-SMAF profiles 1 to 3); approximately 67% had a moderate level of disability (profiles 4 to 9) and 20% of clients belonged to profiles 10 to 14, which represent a high level of disability.
Concerning satisfaction (see Table 2 in Additional file 10), the clients at all sites had a high level of general satisfaction with health care and services. Under the relationship dimension, clients underlined that professionals were courteous, honest when answering questions, and used easy-to-understand language. They felt they could trust the professionals and were satisfied with respect for privacy. They were less satisfied, however, about not always having the same professional each time. In terms of service, clients were mostly satisfied when it came to receiving information on the services available, where to go, what to do, and so on. They were less satisfied regarding receiving information about their different choices and the fact they were not encouraged to get support from their caregivers. Clients were mostly satisfied with the accessibility of services at convenient times and the ease and speed of obtaining appointments, and so on, but they were somewhat dissatisfied about the number of steps it took to obtain the help they wanted.
Concerning involvement in decision-making (see Table 3 in Additional file 10), clients felt that they could decide what care and services they needed and the type to receive but that they could not decide how much. They felt that their choices were respected, they received all the information they wanted, and they got the help they needed. Their level of control about asking questions, requesting explanations, or asking for advice, however, was relatively low. Concerning the process of shared decision-making associated with the OCCIs (see Tables 4 and 5 in Additional file 10), all clients considered it was very/extremely important that professionals give them all the necessary information to decide which needs should be prioritized, that professionals pay attention to their understanding of each need discussed, and apprize them of the risks and advantages of the options for care and services. When we asked the clients how they perceived these actions in their cases, most felt that professionals paid a lot of attention to their understanding of each need discussed. In contrast, only 60% of them felt other actions had been taken in their cases.
Concerning the conditions of computer use, the professionals were taught during training how to present the computer screen to their clients and to present the various sections to facilitate the decision-making process and help clients better follow the clinical process. Clients expressed disinterest in screen presentations and information, but over half expressed desire for home access to their records. Most clients did not have the impression that computer use negatively affected the professionals’ attention or discussions with them. In fact, it did not bother them at all. Some even said that using the computer helped them communicate with the professional. When asked what could have improved their experience, half of the participants replied that they had not encountered any obstacles or problems during their episode of care and services. Nevertheless, one-third mentioned that they found the assessment very time-consuming, and some added that this made no difference to their services. Others said that there was a delay in obtaining certain services (e.g., waiting for a return call, a long delay between the request and the assessment, or obtaining technical aids). Some informal caregivers said they had not received enough information. For example, they would have liked to have been better informed about existing resources or the approach they should use with their relative suffering from Alzheimer’s disease. Lastly, one participant felt that there was a lack of decision-making and said that it was the care provider who ultimately decided on the services.
3.7. Research Question 6. The Plausible Underlying Mechanisms Leading to Outcomes
From the results associated with determinants, strategies, and outcomes, we identified the series of steps through which the strategies might work to address barriers or leverage facilitators or influence participant behavior and contribute to implementation and innovation outcomes. A comparison of the results from Sites A, B, and C allows us to confirm that, for all the dimensions assessed, the conditions observed at Site B were more conducive to achieving better outcomes than those at Sites A and C. Overall, we have identified four main interrelated pathways that, when followed consecutively during deployment, could explain the most positive outcomes. The first two pathways operated at the macro level, while the third acted at the meso level, and the last one was at the micro level. For descriptive purposes, the mechanisms seem to have operated distinctly along the four pathways. In fact, however, they overlapped and depended heavily on what had or had not happened at another level.
The text below provides a justification for each pathway, together with the underlying Theories that might explain how and why many constructs have worked together to produce the various results. The identified “Strategy” and plausible “MoAs” and “BCTs” (in inverted commas and parentheses) are also presented when appropriate. At the end of this section, we also explain some conditions that might have slowed down the adoption process and led to poorer outcomes, especially at Sites A and C. Additional file 11 presents—for each designated strategy—the associated MoAs through which behavior change techniques (BCTs) might be able to influence behaviors and outcomes. Descriptions are provided according to the nomenclature of the heat map tool linking BCTs to MoAs (https://theoryandtechniquetool.humanbehaviourchange.org/tool). Figure 6 uses the IRLM to present the overall logic of what worked well across the three sites as regard specific determinants, strategies, hypothesized mechanisms, and outcomes.
3.7.1. Pathway 1. Engaging Knowledge Users and Relevant Interest Holders in a Partnership Model for the Duration of the Study
Foremost, let’s remember that the decision to implement the OCCIs was made at the level of the provincial health authority, as the OCCIs were seen as a solution to establish more efficient practices and service organization. In parallel, some CLSCs in the province became aware of the OCCIs and determined they might be useful in solving their practice issues and showed interest in serving as a pilot site for eventual OCCI implementation. Translating these complex healthcare interventions—including incorporating new paradigms into contextualized, sustainable clinical models—was also perceived as a major challenge, especially as it required significant investments and efforts to adapt the accompanying RISPA solution. In this way, they preferred to select sites recognized as innovative and able to quickly respond to the technological changes associated with this project.
Based on the principles of collaborative governance [124], the DGAPA/MSSS (the seniors and caregivers directorate) decided to establish a monitoring committee on which interorganizational and intersectoral collaboration would represent the prevailing pattern of behaviors and activities to achieve common objectives. An important feature of this partnership is that it has provided the impetus for bringing together partners and knowledge users from many levels of the health system (macro, meso, and micro) and sectors (academic, educational) (“Develop academic partnerships,” “Work with educational institutions”). It also involved existing governing structures with a track record of successful collaboration in the implementation effort: “Involve executive boards.”
As starting conditions, they involved all these persons as equal partners, allowing them to incorporate their expertise, promote information sharing and collaborative problem-solving, inform the project, and act on the findings: “Promote network weaving.” The collaborative process helped to balance the limitations associated with the top-down and mandated implementation with a bottom-up feedback loop. This usually makes a project more relevant to and more likely to be useful to the knowledge users [125]. Members from the three sites were considered as experts on their own needs and realities (“Capture and share local knowledge”) in which the RSIPA system integrating the OCCIs was implemented [125]. A project manager from the DGAPA with authority and leadership (BCT 9.1.“Credible source”) was assigned to assist and coordinate the various activities of the committee and implementation process in accordance with MSSS directives. This manager also had to ensure that the DGTI (the information technology (IT) directorate) made the necessary RSIPA system corrections as soon as possible to ensure proper functioning at all sites. This person collaborated with an external project officer and research coordinator to ensure the project adhered to ethical standards and scientific principles (“Facilitation”). The committee met weekly for 8 weeks and monthly thereafter with each site to discuss implementation, OCCI-RSIPA components, improvement suggestions, and the correct project sequence, as required. Meetings between the three sites were also held. These various encounters were opportunities for pilot sites to express their ideas, expectations, and concerns to the authorities while receiving advice and support from other sectors (academic, educational, and research perspectives). Their engagement was strongly linked to the possibility of being able to influence the implementation process and adapt the RSIPA solution and the OCCIs to their needs. This mode of functioning promoted a shared understanding of the project, the empowerment of managers, and the openness to exploring mutual gains—(MoAs: “Goals commitment,” “Social influences,” “Beliefs about capabilities,” “Self-efficacy,” and “Behavioral regulation”). Effective communication and collaboration have probably empowered participants at each site with relevant information, leading to an enhanced sense of confidence when preparing themselves and their settings for the implementation.
To support this collaboration, some incentives were also put in place. Each partner (the DGAPA and the DGTI from the MSSS, the CESS, the research team, and the CISSS/CIUSSS pilot sites) adopted a draft agreement describing the different roles and responsibilities (“Obtain formal commitments”). The contract stipulated that each site must create an implementation plan to streamline project implementation. The government also offered financial incentives to motivate providers to deliver clinical innovation and facilitate carrying out the project—“fund “and contract.” In addition to considering the time it takes to learn new behaviors and encouraging efforts that will make clinicians deliver the innovation, they affirmed that the target to reach performance indicators will be reduced during the implementation (“Change liability law”).
Under the TPB/Reasoned Action [126] and Goal-Setting Theory [127], all these actions have fostered good interpersonal relationships, positive general attitudes and beliefs, trust, motivation, and control of decision-makers and managers at the three sites, which has promoted their adhesion and commitment to this project and enabled a primary adoption process at the organizational level [128].
3.7.2. Pathway 2. Providing an IS That Supports Clinical and Management Processes Associated With the OCCIs
In order to be successfully adopted, the RSIPA solution had to include key functionalities linked to the introduction of the OCCIs and operate smoothly and efficiently in clinical environments under real-life conditions. As the Quebec system and the OCCIs are part of an IC context, it was obvious that they also had to ensure organizational interoperability.
The software development of the RSIPA 2016 was based on AGILE methodology using SCRUM practices, which the DGTI was quite familiar with. Basically, the methodology used an incremental, iterative work cadence—known as sprints of about four to six weeks—to respond to required modifications. It provides many advantages, such as rapid iterations with new features being available to end users in each sprint and the ability to adapt to new requests. As for the initial design, the continuing development was also based on PD to involve interest holders and end users such as researchers, managers, and healthcare professionals at the three sites. Through regular meetings and conference calls, group outputs were combined with available resources weighed (time, human, and financial) to prioritize actions. These were sent to the development team for evaluation and integration into future sprints. End users tested each new version and provided feedback on its usability, features, information display, problems encountered, and required improvements. It was crucial to consider user experience during the development and adaptation process to create an IS that would meet users’ needs, thereby increasing its overall acceptability and willingness to be adopted and recommended to colleagues. Many adaptations were made to the RSIPA that enabled achievement of a better fit between this system and clinical contexts (“Promote adaptability”). The contribution of end users in adapting the innovation was planned and consciously nested in process implementation. This process contributed to the reshaping of the innovation while retaining a degree of standardization at the system level to retain the innovation’s core elements that were expected to produce its intended effects (e.g., the process of decision-making). This was crucial to preserve OCCI fidelity.
The DGTI integrated this system across the three pilot sites in such a way that any new assessment or reassessment had to be done in the RSIPA 2016 (“Use data warehousing techniques”). Considering the importance of optimizing service delivery while minimizing interruptions to care during the project, the DGTI “centralized technical assistance” to deliver assistance focusing on implementation issues (BCTs: “Restructuring the physical environment,” “Social support (practical)”; MoAs: “Environment, context & resources,” “Behavioral cueing,” “Social influence”). It should be noted that many initial facilitating conditions were already in place at Site B. This site had been using the RSIPA 2009 for a long time with a good level of implementation. Their familiarity with this system and the possibility to transfer data from the earlier RSIPA 2009 promoted the new system’s acceptability and facilitated use of the OCCIs. Professionals at this site strongly agreed that OCCI content was clear, and they perceived the system to be less complex than did the other sites. The RSIPA 2016 was therefore better accepted at Site B than at Sites A and C.
At Site C, they were using the RSIPA solution with a moderate level of implementation; several professionals were still using the paper version. Despite the highlighted advantages of computerization, some professionals were less comfortable with computers and were afraid of client reactions when using the computer in the home. Just before the start of the study, however, 68 care providers received training on the RSIPA. They appreciated the fact that computerization could save time in the office and increase time with the home-care client. Apart from their concerns about IT support and hardware, they were confident and enthusiastic about starting to work with the new RSIPA.
In summary, under the updated DeLone & McLean (D&M) IS success model [92] and the Unified Theory of Acceptance and Usage of Technology (UTAUT) [105, 114, 115], we can see how several constructs have come together. Participants at Sites B and C had some characteristics that favored use of the RSIPA system. They were initially receptive to this IS, they intended to use it, and they found the RSIPA acceptable. The DGTI used some strategies such as the PD method to understand end-user needs and received their input to improve the IS. The DGTI also provided continuous adaptations that helped to facilitate learning and usability by improving RSIPA functionalities. The fact that Sites B and C started after the trial at Site A was an important facilitator. Site A encountered many problems in the first few months, such as data loss, system instability and slowness, and Internet accessibility, that pushed the centralized technical assistance of the DGTI to resolve these problems and to deliver a lot of assistance specifically on these implementation issues. They have thus improved some functionalities and the system quality of the RSIPA solution (e.g., usability, reliability, and response time). DGTI centralized technical assistance has delivered the necessary support perceived as good service quality. Approximately 6 months later, a meeting was held with the monitoring committee—including representatives from all the sites—to take stock of the situation and specifically discuss RSIPA functionalities. All the improvements made since the beginning and those the DGTI wished to launch were presented. After discussion on each new element, the group had to make “GO/NO GO” decisions; all the proposals were accepted. This was a turning point in the project. As performance expectancy is a strong predictor of intention to use an IS, this meeting energized all the sites. They all confirmed that, with this version of the RSIPA, “they would never go back.” This action strengthened optimism and positive beliefs at all sites about the RSIPA. It also gave them the confidence and motivation to push on and the arguments needed to commit all the professionals to pursue the implementation. After 12 months, all sites appreciated using many functionalities (usability) and the acceptable time to establish the connection to the RSIPA or to the Internet. These factors sustained the use of the RSIPA and therefore the OCCIs since they were intimately linked. This increased the feasibility of the implementation, and, over time, participants perceived the IS’s usefulness (appropriateness), which subsequently increased user satisfaction (acceptability). Generally, the professionals at Site B were strongly in agreement on the usability and usefulness of and satisfaction with almost all RSIPA components and functions. Those at Site C also agreed, but for fewer components; professionals at Site A moderately agreed for some components.
3.7.3. Pathway 3. Building a Conducive Environment With Deliberate Efforts to Increase Buy-In and Engagement
Since the three sites were seen as innovative environments, several enabling factors were already in place when the study was launched to facilitate the adoption process. More importantly, considerable and constant efforts were made throughout the study to increase the probability of successful implementation. Specifically, the context and the innovation characteristics were perceived as relatively favorable at the three sites but more so at Site B, followed by Sites C and A. Managers at Sites B and C were particularly enthusiastic about participating in the study. They saw an added value and considered it was a privilege to be able to experience the project on an experimental basis before the provincial deployment (MoA: “Image” [129]: i.e., the innovation is perceived to enhance one’s image and status in the provincial network). All sites valued the fact that the principles guiding the OCCIs were consistent with their missions and that the areas of responsibilities and authority were already well defined in all the settings. So, in the preimplementation phase, they all perceived that OCCI implementation was feasible, that they were ready, and that their climate implementation would facilitate OCCI introduction [130]. Since the OCCIs commonly conformed to participant attitudes and beliefs, the implementation mandate was not seen as a limitation or constraint at Sites B and C, but rather as an opportunity for engagement, initiatives, and proactive thinking [128]. Nevertheless, managers at Site A adopted more effective and tighter project management throughout the study than Sites B and C.
In general, most of the actions undertaken in this pathway followed the principles linked to the Diffusion of Innovation Theory [121]. Sites have built on their existing working relationships and organizational units to seek consensus around their implementation decision to increase the commitment of all parties. First, they created a local steering committee (clinical, management, and techno-clinical advisors) (“Promote network weaving”), assuring a high level of engagement in problem-solving, decision-making, and change (BCTs: “Restructuring the social environment,” “Problem solving”; “Goal setting (outcome)”; MoA: “Goals,” “Participation,” “Motivation”). During these meetings, they also involved local opinions leaders from the clinical field in the hopes that they will influence colleagues to adopt the OCCIs (MoA: “Mobilizing,” “Inform local opinion leaders”). They used persuasive communication (MoA) to guide individuals toward the attitudes and actions with arguments to engage all relevant directions and arrive at a common understanding of the mandate and its intentions (“Use advisory boards and workgroups”). They also used a problem monitoring system to allow rapid response and to align practices with the implementation goals. Lastly, some members and professionals representing diverse disciplines were selected to discuss issues with the MSSS committee during conference calls (“Facilitation”).
From then on, they prepared an implementation plan with realist timelines focusing on coherent relationships between ends, ways, and means while balancing the available human, material, technological, and financial resources (“Tailor strategies”). When possible, they have broken down the main goals into manageable steps. When the study began, however, only Site A had a formal implementation plan that included a clearly defined communication plan. As Sites B and C decided to implement on a small scale, they did not perceive the need to structure everything that soon; their plans were developed later. In the communication plans, managers tried to use messages designed to raise awareness, strengthen positive beliefs, and weaken negative beliefs to influence participants’ decisions to adopt the OCCIs (MoA: “Belief selection”) (TPB/Reasoned Action) [126]. Lastly, to follow these plans, all sites monitored indicators usually used for MSSS accountability to obtain convincing data demonstrating successful implementation, which later promoted individual motivation (MoA) (“Develop and organize quality monitoring systems”). At the end of the study, we noted rigorous supervision of and a firm commitment to the project at all sites: They succeeded in implementing the OCCIs on schedule. Despite a context marked by uncertainty, managers adhered to the need to trust the skills and adaptability of the champions and opinion leaders in the field.
Concerning deployment, Sites B and C adopted a stepwise approach with small steps, obtaining some success, before going to a larger deployment. This strategy (“Stage implementation scale-up”) provided a preliminary proof of concept [131] that promoted early observability of the innovation and confirmed that the OCCIs could be implemented under routine program conditions (BCT: “Graded tasks”; MoAs: “Knowledge,” “Skills,” “Beliefs about Capabilities,” “Reinforcement”). This strengthened positive beliefs and reassured participants that the implementation decision was beneficial (MoA: “Belief selection”), TPB/Reasoned Action [126].
Sites A and B identified, informed, and trained “early adopters,” “champions,” and local opinions leaders to provide “clinical supervision” and “ongoing training” that increased their self-efficacy, motivation, and a sense of ownership in participating in the OCCI/RSIPA implementation (MoA: “Social influence,” “Belief capability”). Since these professionals had already participated in pilot projects, had protected time, and were recognized as voluntary, efficient, and open to change (determinants), they were able to devote themselves to supporting, marketing, and driving through the implementation and to overcoming any indifference or resistance.
In terms of opportunities, each site thought about their existing organizational process, physical structure, and/or equipment. They then planned and sought to provide enough resources in terms of staff, space, materials, and time to best accommodate and encourage professionals to use and adopt the OCCIs (“Provide local technical assistance” and “Change physical structure and equipment”), (BCTs: “Restructuring the physical environment,” “Social support,” “Action planning,” “Adding objects to the environment”; MoAs: “Environment,” “Context and resources,” “Behavioral cues,” “Social influence”). Specifically, Sites B and C considered they received the necessary support in terms of financial resources. At the preimplementation phase, Site A had adequate computer equipment, which it has had for a long time; adequate technological support and clear procedures have been established.
In parallel to the implementation project, an outside formal assessment by a research team—who was responsible for carrying out a study based on a scientific protocol—was an important key to stimulate engagement of local teams in problem-solving, decision-making, and planning change (BCTs: “Goal-setting” and “Action planning”; MoAs: “Goals,” “Behavioral cues,” “Intention,” “Motivation”). This protocol was “a formal implementation blueprint.” In “Conducting local consensus discussions,” each site expressed their needs, perceptions of the innovation attributes, and how it could affect or help their management methods and processes. Discussions helped to clarify the goals and outcomes of the OCCIs and increase awareness about the project, especially about the scope of change (BCTs: “Prompts/cues”; MoAs: “Memory, attention, and decisions”). The specific steps and milestones linked to this assessment were accepted by all sites (“Develop and implement tools for quality monitoring), (BCTs: “Monitoring and feedback of behaviors and outcomes,” “Restructuring the social environment”), and (MoAs: “Environment, context and resources,” “Motivation,” “Feedback process”). The preimplementation phase made it possible to “Assess for readiness and identification of barriers and facilitators.” The identification of determinants at each site provided a common understanding among the participants about what it was required to project implementation and facilitated the development of local implementation plans, including adapted strategies to each context (“Facilitation”), (BCTs: “Social support,” “Problem solving,” “Social support (practical)”; MoAs: “Social influence,” “Beliefs about capabilities,” and “Behavioral regulation”).
3.7.4. Pathway 4. Facilitating Capacity and Relationship Building to Increase Adoption and Embedding the OCCIs in Usual Practice
Based on the UTAUT [105, 115], adoption is positively related to knowledge, attitudes, and attributes of an innovation. At the preimplementation phase, professionals at all sites confirmed that they already had a good level of knowledge and self-efficacy with the usual clinical process and many concepts targeted by the OCCIs (i.e., comprehensive assessment). They were less familiar, however, with certain concepts such as shared decision-making and using the new RSIPA functionalities. Thus, strategies such as “Conduct educational meetings,” “Develop educational materials,” “Distribute educational materials,” “Make training dynamic,” and “Work with academic and educational institutions” were useful in increasing the levels of knowledge, skills, and awareness of the project (BCTs: “Instructions on how to perform behavior,” “Demonstration of behavior,” “Behavioral practices/rehearsal”; “Information on health consequences for clients”; MoAs: “Knowledge,” “Skill,” “Beliefs about capabilities,” “Intention,” “Beliefs about consequences,” and “Attitudes about behaviors”). The training was found to be useful, well-organized, and delivered by experienced trainers. They recognized that the acquisition of new knowledge and skills was adequate for OCCI use. Developing knowledge to develop both procedural and scientific knowledge via education and training increased confidence among professionals to use the OCCIs with their clients and favored OCCI acceptability. Thus, faced with OCCI implementation, participants did not deem the gap with existing practices too significant, and they were confident in their ability to make the change and willing to use them.
Regarding OCCI characteristics, the providers all found OCCI attributes suitable to their contexts, compatible with their clinical process, and offered several advantages in improving care quality. They were receptive to any proposed changes or interventions to improve care management and recognized the importance of improving care quality. They perceived that compatibility increased the expected benefits of the OCCIs, since professionals perceived they would make fewer efforts to integrate them into their usual practices. Sites B and C were also reassured by the partial clinical adaptation of OCCI content during the initial electronic prototype development at Site A. This positive attitude and the perceived behavioral control of the OCCIs facilitated from the outset the buying-in of the OCCIs by managers and professionals at the three sites. Nevertheless, for many reasons that will be explained below, the professionals at Site A perceived fewer advantages of the OCCIs than their counterparts and were less motivated and enthusiastic, which significantly impeded adoption at this site. After the main training, other strategies were applied when the implementation started: “Create a learning collaborative,” “Conduct ongoing training,” “Use train-the-trainer strategies,” “Provide ongoing consultation” (BCTs: “Feedback on behavior,” “Social support (practical),” “Instructions on how perform a behavior,” “Restructuring the social environment,” “Credible source”; MoAs: “Social Influence,” “Motivation,” “Feedback process,” “Attitudes about behavior,” “General attitudes and beliefs,” and “Beliefs about capabilities”). The initial adoption of the OCCIs by champions, opinion leaders, and supervisors acted as a signal, via observation, imitation, and influence on other potential adopters. The principle of subjective norms—i.e., the professionals’ perception that persons important for them (their champions and opinion leaders) think they should perform the behavior in question—was therefore applied (MoA [118]). This also led potential adopters to feel comfortable with the organizational decision [121].
After 6 months, professionals confirmed that in-house training, ongoing training, supervision, and the clinical support for using the OCCIs favored implementing the OCCIs with fidelity. This is the supervisors’ ability to help their colleagues make choices in a gradual way, considering both their progress and capacities, which led the colleagues to commit to the process of change. This created social and regulatory pressures that allowed for shared positive interpretive schemes that motivated their intention to pursue using the OCCIs. At that time, however, some aspects were less positive. Professionals reported not having enough time to use or adjust to the OCCIs and not having received sufficient technological support when necessary. Both managers and professionals recognized that managers demonstrated a great willingness to make OCCI implementation work, but only participants at Site B confirmed that trained professionals demonstrated the same attitude. At Site C, it was felt that OCCI use was not progressing as quickly as expected. These results were discussed during the focus groups. The managers mentioned that they had had significant difficulty resolving these problems, but it seems that, after several months, these elements were put into order. All the sites tracked implementation via monitoring strategies, such as establishing quality monitoring systems or purposely reexamining implementation. These strategies encouraged planned changes (action planning) based on acquiring targeted knowledge (“Facilitate relay of clinical data to providers”) (“Feedback on behaviors and outcomes”; MoAs: “Motivation,” “Feedback process,” “Reinforcement”).
At that time, many adaptations were also made in both the RSIPA and the OCCIs that improved system usability. It increased the perception of ease of use, professionals’ ability, and the belief that using these tools enhanced their work. This increased skills and capability, as well as facilitated mastery of the desired behavior. For example, professionals felt they were better and more efficient when meeting clients at home. This outcome increased individual esteem and a sense of accomplishment while fostering social and professional identity (Theory of Reasoned Action, Planned Behavior, Social Cognitive Theory); (MoA: “Attitude toward behavior,” “Perceived behavioral control,” “Outcome expectations,” “Self-efficacy”). Professionals mentioned they have become more confident using the OCCIs correctly and have acquired expertise in the use of technology. They also perceived that both the RSIPA and the OCCIs were useful which increased use and satisfaction (MoAs: Emotion, Attitudes about behaviors, Behavioral regulation). At the same time, professionals worked with their clients to actively share in decision-making and care planning. All professionals perceived several advantages for their home-care clients and using the OCCIs with clients who expressed satisfaction and did not object to computer use during assessment reinforced their perceptions that their actions were meaningful and legitimate (“Prepare patients to be active participants”). It created a positive feedback loop because workers were exposed to the outcome of their actions with clients, which motivated the repetition of their behaviors (MoA: “Reinforcement”). After 12 months, these positive effects on practices that became more observable and tangible for professionals increased OCCI adoption and penetration. They also built optimism and positive belief in the OCCIs. That increased the organizational dynamics, network strength and quality, and communication between healthcare providers. The penetration increased as a process of mutual adjustment between professionals with the OCCIs and their contexts. This process took place until the OCCIs become embedded in the usual clinical process. Over time, as their use was legitimized, the OCCIs became institutionalized in regular clinical processes.
3.7.5. What did Not Work so Well for Some Aspects in Varied Contexts?
Several initial conditions at Site A were detrimental and have determined why the adoption process slowed down considerably, making the results less significant at this site. A large part can be explained by the consequences of forced adoption [128] and the cognitive dissonance theory [132] applied to technology adoption [133]. Heidenreich and Talke [128] explained the negative consequences of forced adoption and illustrated that, under some circumstances, these consequences escalated over time along the adoption process stages of Rogers [121]. Bhattacherjee [133] showed that dissonance (discrepancies [132]) between users’ original expectations and observed performance is captured in the disconfirmation construct. This depicts that negative disconfirmation of initial beliefs about technology characteristics and performance might result in dissatisfaction and discontinuous use intention. Festinger [132], however, also defined dissonance as a motivating force as people are motivated to reduce the aversive arousal produced by inconsistent cognitions. One of many strategies of dissonance reduction (e.g., attitude change, trivialization, denial of responsibility) is the enhancement to approach motivation (e.g., by inducing an action-oriented mindset) to reduce discrepancy [134, 135].
This is, in fact, a long story in this setting. Before the MSSS intended to implement the RSIPA 2016 integrating the OCCIs, this site was no longer using RSIPA 2009, but rather the earlier OCCI prototype, which was adapted by them and integrated into their computer-based patient record (CPR). This prototype had the advantage of being linked to disciplinary assessments, progress notes, and disciplinary plans; it was adopted at all levels from decision-makers to professionals and ensured organizational interoperability. One year later, the arrival of a new government forced them to take on part of the RSIPA and use the planning module named the PSIAS, on a mandatory basis. This module was not really appreciated, but the site was able to continue using their OCCI prototype. Less than 2 years later, the government was replaced. The new health minister expressed his vision of using the RSIPA solution universally in all the long-term homes and healthcare and social services. Moreover, he prohibited the use of any other system in this setting. He also decided to integrate the OCCI prototype into the new RSIPA version with the involvement of the research team and representatives from this site [68]. Participants at this site were very disappointed by this major shift. They had doubts about the RSIPA and were concerned about losing the interoperability benefits provided by the earlier OCCI prototype. They reported that not having OCCIs Phases 4 and 5 available in the system was not helpful because there lacked a mechanism for easily updating plans or indicating that a service had been started or completed. The planning section was not perceived to be user-friendly. Site A participants really experienced a loss and felt that several years would pass before these benefits would be restored, even if slated in future IT development. Because they were very satisfied with their previous system, they reflected very little tension for change. Because of their track record of successful innovation in IT, they finally accepted being a good player and to participate as a pilot site.
Site A was the first to implement the project with all three of its CLSCs taking part. The local involvement and participation were there from the start. They actively participated in the preimplementation phase, including training. Nevertheless, the pressure to quickly implement in the middle of summer vacation came at a bad time, as it was difficult to organize training and produced significantly disenchanted participants. Moreover, decision-makers decided from the outset to deploy on a larger scale, involving professionals with little interest in the project and even those opposed to it. The fact that these individuals lacked motivation created a negative social influence on the group, which required managers to expend considerable energy in convincing them to engage. In addition, there was not adequate financial support to sustain the cost of a larger deployment. Lastly, the technical usability and performance of the RSIPA were problematic. Poor integration of the RSIPA in the usual workflow, new work related to the introduction of the system, errors, and limitations of the systems exacerbated the work burden for professionals. Managers were forced to say “stop using the RSIPA. It doesn’t work.” This led the professionals to have anxious and emotional reactions about using the OCCIs (Social cognitive theory: “Reduced Self-efficacy,” “Affect,” and “Anxiety”). This significantly exacerbated the professionals’ frustration, and the cynicism related to the reinstatement of the RSIPA, which they had not used for some time. Negative social influences (MoA), where professionals perceived that others believed they should not use this new system, have intensified. At this moment, adopters experienced cognitive dissonance because of the conflict between the decision of professionals to use the system despite everything (to act to answer the needs of home care clients) and the low performance observed with interruptions in care, which brought negative disconfirmation. This resulted in dissatisfaction and greatly diminished the intention to use the new system. The managers, faced with these reactions, were forced to retreat because of the perceived lack of control over the project that was necessary to adopt the new technology in so short a time. All these technological problems were not so surprising for a project of this scale and complexity. Nevertheless, the DGAPA and the DGTI had to redouble their efforts to improve the RSIPA solution and convince this site to stay on course.
Despite this painful experience, the implementation team at Site A worked proactively with their local leaders and champions to relieve the cognitive dissonance and restore balance among all participants to ensure clinical engagement [121]. Based on the principle of keep the ball rolling (MoAs: Action-oriented mindset), the process management was iterative and adaptive, with constantly redefining and negotiating goals to make sure they could transcend all technology and organizational problems. After some months, despite some improvements, a mismatch between workflow and RSIPA functionality was still observed. Dissatisfaction was growing because adaptations to the RSIPA to meet practice needs were not delivered quickly enough. Representatives were exasperated by always repeating requests without any changes being made. This led managers and professionals to lose confidence in the project. The perception that the RSIPA, and now the OCCIs, could bring benefits to home-care clients was increasingly negative, especially among professionals. As a result, the professionals became demotivated and maintained a minimum level of commitment. In return, the good news is that many improvements were made after 6 months. The high level of leadership of managers helped them to pursue the implementation process to finally produce some positive results after 12 months. More importantly, the experience at Site A becomes a gateway to facilitate subsequent implementation at Sites B and C.
Site C also took some time at the beginning of the study to adopt the OCCIs, but for different reasons. This site had been using the RSIPA solution before the study with a moderate to high level of implementation (74.5%), but several professionals were still working in paper mode. This site was disappointed with the system because, even after many months, the OCCIs had not yet been computerized in English even though a large part of their clientele and their workers were English-speaking. Having to work in both languages increased their mental workload and made them less effective at conducting home assessments. Like Site B, this site also started out small. In contrast, it targeted professionals who were simply told that they would be involved in the project. Overall, the site was in favor of the RSIPA and the OCCIs, but the IT infrastructure was inadequate, and it took some time for the professionals to have access to computers.
4. Discussion
The OCCIs are a computerized care-pathways system that proactively seeks to support and coordinate evidence-based care centered around the needs of older people in their own home environments. Grounded in well-recognized frameworks, models, or taxonomies [97, 100–102, 112, 113], we were able through this study to prospectively discern various determinants, strategies, mechanisms, and outcomes related to their implementation in three home-care settings. Through this process, we captured insights into what has and has not worked when implementing innovation to improve clinical integration of care. We observed that components of implementation interacted progressively over a sequence of phases with constant efforts on multiple levels of health and social care (i.e., macro, meso, and micro). In this way, the OCCIs were gradually incorporated into routine practice, albeit at varying rates. Positive implementation and innovation outcomes were thus noted, though to differing degrees depending on the contexts examined. Using the IRLM, we were able to synthesize and report our findings in one comprehensive picture.
When it came to determinants, we saw some of the same barriers and facilitators that were found in studies on IC, even though the settings were different in terms of where they happened (local, regional, or national) [16, 19, 136–138]. These barriers included insufficient information sharing between organizations, limited resources and support, insufficient funding, and difficulties in tailoring services to the needs of patients. Supportive factors included the presence of a collaborative governance with clear communication, a flexible implementation plan with a stepwise approach, distributed leadership throughout all levels of the system, previous experience and practice with the change process, a good level of knowledge through professional training, the involvement of a local champion, a multidisciplinary team culture, a monitoring system with feedback loops, and alignment between the innovation and the system.
Among the perceived advantages of the OCCIs, we noted the use of a common language across several disciplines with standardized tools, a comprehensive assessment focusing on the client’s needs and risk factors, a system that supports shared decision-making with clients and their caregivers, an evidence-based care planning process customized with priorities elicited by the client, and follow-up with variance analysis. In return, even though the OCCIs were perceived as advantageous compared to past practices and well aligned with the individuals’ and organizational goals and values, completion time negatively affected their acceptability. The time-consuming barriers were frequently reported using the CGA [49, 71]. In terms of information quality, participants found that OCCI information improved access to up-to-date client information, but the amount of information was sometimes considered excessive for some clinical situations. Some participants wondered if some sections of the assessment could be abridged, particularly when a referred person has just been discharged from the hospital. Nonetheless, nobody questioned using the OCCIs for home-care clients, but both the professionals and their clients emphasize that the process is too long and detracts from their satisfaction. A lower level of satisfaction must be considered, since it can also lead to a decline in OCCI use over time, as pointed out by DeLone and McLean [92]. Apart from offering more time, no site has tried to provide a solution to get around this difficulty. Stijnen et al. [139] suggest that the application of CGAs on a large scale should be scrutinized, as the comprehensive evaluation is likely more appropriate for individuals with two or more chronic conditions but with a moderate level of disability. This would mitigate the deterioration of functional status in these individuals. In terms of effectiveness, Iliffe and Orrell [140] suggested identifying common unmet needs through a short, targeted assessment or a two-step process instead of a full but lengthy multidimensional assessment for all older adults. Many screening tools have been specifically created to help identify vulnerable patients most likely to benefit from a full CGA [141]. The clinical process could possibly also be adapted. For example, portions of the geriatric assessment could be conducted over several visits. One avenue might be to initially target functional status and some areas that seem to have an impact on the clinical situation while completing other aspects during other visits. At first glance, considering the insufficient resources in our home-care services, it seems desirable to better target the clientele who could benefit from a comprehensive assessment or to use a two-step approach [142].
Another barrier is the fact that the number of assessments and care plans in long-term home-support service programs are among MSSS performance targets. This may have acted as a catalyst to promote the OCCI establishment, but it also caused anxiety and stress for all participants in meeting these targets during the project. Despite the MSSS reassuring the sites that a decrease would be of no consequence, it remained a constant concern for all participants. We believe that there should be a constructive discussion on the use of these indicators, as they compromise OCCI acceptability and will probably affect their sustainability over time. A prior study showed that this mechanism influenced clinical reasoning and altered the delivery of assessment and follow-up services [33]. Various studies also reported that IC systems focus too heavily on system effects rather than on the benefits for their clientele [143–146]. CGAs, with their process, do not exist only to create documentation and provide data for statistical purposes or performance indicators but mainly to sustain professionals in comprehensively understanding client needs and in adequately managing the clinical situation [147, 148]. Shifting to indicators beyond volume, such as the attainment of individualized care goals or variance analysis—both of which are already present in the OCCIs—could fulfill monitoring management objectives while being more relevant for clinicians. Other promising approaches, such as patient-reported outcome measures (PROMs)—which elicit patients’ views (e.g., perceptions of their symptoms or their functional status) or patient-reported experience measures (PREMs)—which measure their perceptions of services provided—are also certainly more salient in a context of person-centered care [100, 101]. PROMs were introduced in many countries to evaluate healthcare effectiveness at different levels of the health system, from the individual to the service and system levels [149, 150]. In an IC system, PROMs and PREMs might also allow for better communication and shared decision-making between patients and providers (see ACI, https://aci.health.nsw.gov.au/__data/assets/pdf_file/0007/918385/ACI-Proms-Prems-report.pdf, [151] and https://ssaquebec.ca/wp-content/uploads/2023/04/PREMs-PROMs-complete-toolkit-1-1.pdf [152, 153]). Lastly, they are in accordance with the value-based healthcare system, an approach centered on patients’ needs in which the patient is directly involved in decisions regarding his own health and where the goal is better health outcomes—as also promoted by the OCCIs [154].
One other contingency was linked to the RSIPA solution in which the OCCIs were embedded. The lack of fluidity in moving from one section to another (e.g., from assessment to care plan) and the complexity of using certain technology features—including drop-down menus and the care plan section—were noted. Matching the clinical process with the usual navigation in an HIS is not a simple task and compromises the acceptance and satisfaction of end users. Like all other HISs [147], the RSIPA was built with an orderly linear work process in which each section follows a prescribed set of items in a specific order and in which it is not always easy to move quickly from one section to another without completing the whole section or to go from one part to another and back again easily. This explains the use of workarounds such as hardcopy acting as a temporary memory aid of ideas when navigating through the RSIPA. This strategy was documented in other studies [155–157]. This tactic can also disrupt the efficient information flow and communication if the data are not transferred to the HIS [158]. In contrast to the HIS process, clinical judgment is based on an iterative process of sensing, proving, and reformulating goals according to home-care client needs, their caregivers, the clinical circumstances, and the environment. Some findings suggest that HERs could potentially yield care that is higher in quality and more cost-effective by efficiently supporting healthcare providers in their work. At the same time, they can interfere with communication and clinical judgment instead of fostering them [133, 144, 145]. Moreover, professionals from different disciplines use different mental models and specific clinical judgments that can generate differences in end-user needs when using the technology [147]. Despite these limits, a good strategy has been to involve end users, which has been highlighted as very important in many studies to help ensure that the RSIPA met end-user needs and workflows, as well as promoting acceptance among participants [159]. It made it possible over time to incrementally develop a system adapted to end users and to reduce the gap between RSIPA functionality and OCCI components and clinical workflow. It resulted in a system with better functionalities in terms of usability and usefulness that helped enhance system quality, system use, and end-user satisfaction. Usability and usefulness have commonly been identified as critical features of HIS implementation [160]. Many studies also reported the importance of information quality [160]. On this topic, participants agreed that the OCCIs assured that the information in the client’s record was of better quality and more relevant to planning services.
In fact, despite continuous improvements made throughout the study, the RSIPA required further improvement, especially regarding navigation and the care planning module, which has been widely criticized. The challenge is to continue improving the solution while the final phases of the tools have not been completed. In principle, the development of the last phases was slated to begin during the project, but given the numerous requests for system adaptations, the DGTI never managed to do so. In fact, the biggest complaint during the project was the slowness in obtaining the desired changes, which greatly undermined acceptance at Site A. Since Phases 4 and 5 had not been fully completed, it was not possible to aggregate the data to support managers for the allocation of resources and prioritization of services or identifying home-care clients who are most in need of care. This is also another feature that was highly anticipated by our managers, which also limits the possibilities for benchmarking and evidence-based decision-making across sectors or organizations.
Given the information available, we are not in a position to comment on the causes of these delays or whether the technological development model is at issue. The AGILE SCRUM methodology is currently the most applied technological project management approach. It offers many advantages, but it is also recognized as being more suitable for small teams than for larger and more complex projects, as numerous iterations are needed to complete the desired functionalities [148, 161]. In this process, the OCCIs were delivered in small functional parts to check functionality, manage risks, and get early feedback from customers and end users in order to increase the productivity, quality, and value of the software developed [162]. Focusing on working software is also the primary measure of progress. But just because an HIS works, that does not mean that it can be easily integrated into a clinical workflow, as stated above. Accordingly, despite the excellent collaboration between the parties, we sometimes had the feeling that the main emphasis was on processes for meeting requirements and responding to changes rather than following a plan for further development and focusing on good design based on user needs [78].
In addition to the complexity of developing an RSIPA solution able to assimilate the clinical process, we also observed how the RSIPA relied on organizational, structural, technological, and human factors to be successful [159, 163]. One important issue was that there were not any shared IT systems with the secondary care level, which contributed to the restricted level of completion of interdisciplinary and intersectoral care plans [160]. In population-based care management, functional structures and strategies, like referral procedures or service agreements, can enhance horizontal and vertical integration. However, the lack of technical interoperability across care levels may hinder the management of chronic diseases in older individuals with complex conditions. These compatibility issues with other levels of care or systems are not uncommon, as also reported in many countries using other tools, such as the interRAI software [49]. It was expected that the OCCIs would work best in an integrated services network if they had a strong shared IS that everyone involved in caring for the target population could access. Despite the MSSS and DGTI’s initial desire, this did not happen before the study’s end. Previous studies on IC have frequently reported this significant difficulty [20, 23, 136, 164]. To truly promote the integration of services, our system must also implement IT infrastructure that will facilitate access to the continuum of care and make sure that each person will always receive the right care at the right time in the right place [144].
Providing technical support, adequate time for involvement, and getting professionals to use the RSIPA was also vital [160, 165]. Service quality is strongly associated with system implementation and adoption [166]. When end users have support to mitigate technological issues and they have confidence in using the technology, they are more likely to use a system. This was not always the case for Sites B and C, which might explain why they were not inclined to deploy more widely before at least 12 months had passed. As reported elsewhere [136, 138, 167], we also noted many organizational barriers that were not within our control or even that of the sites. These barriers included staff shortages, heavy workloads, insufficient time to perform usual work duties, limited available services, operating with existing organizational budgets, and the presence of provincial policies that impeded changes in practice. Heavy workloads and insufficient time to complete tasks cause moral distress and reduce professional autonomy, which are important factors for staff retention [168]. To support integrative care, a long-term plan with well-protected support and secured funding, as well as payment options that include incentives for high-quality care for those who need it the most, must be provided [23, 169]. Our findings may reflect the real-life implementation challenges facing resource constrained public healthcare settings. Even so, it is surprising that almost all attempts to reform health and social care systems ran into similar problems. Policymakers consistently overlook these problems, despite their acknowledged existence.
No matter what, the most important fact to highlight is how, despite many issues, the strategies used with the various mechanisms as well as the power of the right and committed individuals have facilitated OCCI use, penetration, and sustainability even after 24 months. In this respect, we discerned 40 strategies across all settings that either reduced barriers or leveraged enablers. Almost all were planned at the outset of the study, and very few were modified along the way. According to the ERIC matching tool, the selected strategies were most frequently chosen based on the determinants observed. Most of them were also commonly recommended in other implementation studies [19, 170–172].
Challenges with the technological aspects at Site A confirmed the necessity to make a system available on a small trial basis before committing to fully adopting it. That would allow end users to experiment with the new technology and resolve ex ante problems associated with the innovation [173]. Moreover, our findings show that these technological risks could be managed through sound project management and strong leadership, as observed in other studies [166]. We observed how the collaborative approach described in the first causal pathway demanded a shift away from command-and-control management within centralized bureaucracies to novel forms of collaboration across different levels and boundaries that promoted trust and the desire to carry on despite the obstacles. In examining strategies and mechanisms in other causal pathways, we can also testify as to how significant constant efforts—including devoted resources at multiple levels and appropriate training and supervision—were fundamental to ensuring that the implementation worked and that the OCCIs were institutionalized. We can certainly corroborate how the implementation of a complex innovation in daily practice is much more than the simple adoption and diffusion of innovations [174] and how it is strongly rested on appropriated resources and a continuous and iterative process corresponding to making it happen (i.e., a planned and active process with sustained support intended to increase the rate and level of adoption) [175].
In the evaluation of implementation outcomes, we observed that the mechanisms acted at some point to produce moderate (Site A) to high levels (Site B, then Site C) of feasibility, appropriateness, acceptability, and fidelity of using either the RSIPA or the OCCIs. Fidelity was partly achieved because the professionals were constrained to complete certain sections before going on. This can reduce user satisfaction, but it helps to preserve the “active ingredients” of the OCCIs (e.g., the process of shared decision-making). The level of acceptability has also gradually increased because the adaptations made over time to the RSIPA solution and the OCCIs have favored a better alignment between innovation and usual practice. Over time, the increased acceptance of the innovation resulted in a better experience, providing an instrumental basis for individual intention to use the system instead of relying only on social influence [115].
The evolution of the penetration rate confirmed that it took a certain time (i.e., 12 months after planning) and several active strategies to promote implementation success and for this complex innovation to be truly adopted and produce the expected clinical outcomes [121]. But it also showed that it is possible to support the effective implementation of an innovation during this time frame if the innovation is tailored to each situation and each site comes up with its own implementation plan based on its own unique circumstances. However, this may be less true when it comes to simultaneously improving a technological solution. Notwithstanding, the degree of success might depend on how you look at it. In a certain way, some might perceive that the high penetration rate at Site A might represent greater success than the other two sites. At this site, despite the initial barriers (e.g., frustration, moral distress) and a lower level of perceived usability and usefulness, the presence of other determinants (e.g., a high level of perceived knowledge, skills, self-efficacy, acquired confidence through past technology projects, participant resilience) with the use of a wide variety of strategies (e.g., frequent adaptations and system upgrades, optimizations leading to better usability, a high level of leadership, ongoing clinical and technology support) seems to have been effective to address and encourage the professionals to use the OCCIs over time. The initial moderate level of satisfaction might also be attributed to the pressure of the large-scale deployment. Indeed, professionals felt they had less time than the other sites to learn to use the OCCIs. On the other hand, if the other criteria for success are considered (e.g., satisfaction, appropriateness, feasibility), Site B would qualitatively appear to have had a more successful implementation than the other two sites. From the outset, the experience progressed more satisfactorily at this site. In the case of Sites B and C, it should be remembered that they started after many adaptations to the RSIPA and the OCCIs. Moreover, they adopted a stepwise approach with small steps that gave the most motivated professionals (mostly champions and opinion leaders) time to adjust to the change and to buy into the innovation.
Overall, we confirmed that the OCCIs reached the population they initially targeted. Home-care clients had moderate and high levels of disability in a proportion of 75%–90%. As expected, using the OCCIs, there were a larger number of needs identified in many areas, including psychosocial situation and important risk factors such as malnutrition and risk of falling, which are important conditions that have often been overlooked in the past [39–42]. In this way, the OCCIs have provided a way to assess and support individuals at high risk and requiring complex care. Conversely, there appeared to be some mismatch between needs, preferences, and care goals. Due to the lack of a complete range of services, some professionals have mentioned that care plans were sometimes developed based on the availability of resources instead of user preferences, despite the latter being a prerequisite for creating an optimal offer of health care and social services for older people and their caregivers. Considering the preferences of older people for home care, it seems that an increase toward the home care mode of care delivery accompanied by a targeting toward individuals with moderate care needs could cover more needs in home care and reduce total long-term care costs for our government [176].
With regard to innovation outcomes, initial results at 6 months demonstrated that managers indeed appreciated OCCI benefits, which was less the case among professionals. Nevertheless, the results improved significantly after 12 months, since a good level of acceptability and fidelity was finally achieved, and professionals probably had a better chance of benefiting from the OCCIs’ clinical relevance. As stated in the UTAUT model [105], our findings also confirmed that if people find technology useful and easy to use and if these people benefit from a positive social influence and the support of others, they are more likely to use it over time. Later, the use of OCCIs gave professionals the opportunity to provide individualized care tailored to the priorities of client needs and thus more in line with their desired practice. The benefits across all dimensions were thus perceived positively by both managers and professionals, although slightly lower for the professionals. In addition, some benefits confirmed by home-care clients when assessing patient experience corroborate the positive perceptions. The clients at all sites had a high level of general satisfaction with health care and services. As anticipated by OCCI implementation, clients felt they could choose what care and services they needed and felt their choices were respected; they received all the information they wanted and got the help they needed. Equally, as confirmed by other studies [177–179], home-care clients expressed how important it was for them to decide which needs should be prioritized and to be involved in making decisions about their care.
4.1. Strengths and Limitations
The use of a comparative multiple case study provided a detailed and in-depth understanding of how such a complex innovation can be implemented in actual public health and social care systems. Our cases are representative of diverse CISSSs across the Quebec system and can be generalized to settings with similar contexts. At the same time, they were also illustrative of innovative settings and were selected for their potential to respond quickly to the technological changes associated with this project. In this way, their innovation capacity and other associated traits might not be present elsewhere. That limits generalizability in a traditional sense since additional strategies should probably be considered in other contexts. Some strengths include the use of well-known frameworks, models, and many solid theoretical bases in implementation studies. Using them to guide data collection and reporting was of great value in rapidly identifying, organizing constructs with predefined codes, analyzing the results, and supporting their interpretation.
Double-coding transcripts and the frequent meetings between the research team members were also helpful in refining the codebook and establishing a consensus on coding and interpretations throughout the entire process, especially in the cross-case comparison analysis. This helped achieve a comprehensive, concordant, systematic exploration of our data to enhance categorization consistency and increase finding reliability. The triangulation of data using several methods, the use of relevant sources (high- and mid-level leaders, implementation facilitators, implementation team members, and various healthcare professionals), accompanied by data collection at various organizational levels, was conducive to the emergence of the various facets of the subject under study. That also contributed to the credibility of the results.
There are also some boundaries to consider. Due to the study’s nature, we did not control the selection of study participants. At Site A, all the employees—including late adopters at the three CLSCs—were involved from the beginning. In contrast, Sites B and C selected mostly “champions” for their implementation processes, which might have introduced bias as they were not representative of all the professionals practicing at these sites. Furthermore, we had a small number of participants at these sites. We also counted on the administrative data to estimate OCCI fidelity, but we had not foreseen that some functions (e.g., lack of clear links between assessment, care plans, and services provided) would not be available in the system to give an accurate picture of the activities carried out. For the moment, this study mainly considered the first three OCCI phases. While the completion of the five phases seemed necessary to reach all OCCI goals, it has also been suggested to question how the overall package can be kept simple while maintaining a reasonable expectation of success. The match between innovation complexity and an organization’s capacity is essential. Simplifying the innovation as much as possible (e.g., by implementing one piece after the other) could facilitate implementation [131].
Lastly, as the members of the research team were also the initial designers of the OCCIs, they were probably biased toward their success. When interpreting the results, they were perhaps more inclined to identify areas for improvement and lessons learned rather than areas of weakness. To judge how site participants and home-care clients perceived innovation outcomes, we used questionnaires with adequate psychometric properties that had been used previously in our context of integrated home-care services [103, 108]. The innovation outcomes were also only partly analyzed considering the short time frame, the available financial resources, and the concerns expressed by the decision-makers.
5. Conclusion
This study has provided a broad and in-depth understanding of how the implementation of computerized care pathways has played out in real life. Our findings demonstrate how the implementation success of an innovation depends on many mechanisms with corresponding strategies adjusted to specific contexts. Without a real understanding of the context, it would have been very difficult to elucidate the mechanisms at work in this project. As Coldwell [180] stated, each context is dynamic (i.e., changing over time), agentic (i.e., factors may themselves act independently of the project to lead changes), relational (i.e., factors acting in concert or against project functioning), historically located (covers a process over a longer time than the project), immanent (i.e., the intrinsic part of participants’ responses to the innovation), and complex (leading to changes that arise out of complex change processes at different system levels that interact with the innovation). In this way, our findings provide valuable and relevant insights for conducting further projects. Through a theory-based and holistic approach, this study identified some mechanisms with their associated strategies to promote OCCI use in the clinical context of Quebec home-care services. At the same time, the results underline how important it is for each organization to be objectively aware of its own situation at a very early stage before launching an implementation.
Based on the results of this study and our collaboration, the MSSS has developed an implementation kit to propel the provincial deployment of the OCCIs. All home-care services have been using them consistently since 2019. Recently, some improvements have been made to enhance the care plans and a brief version of the assessment that can be conducted initially before the comprehensive assessment is now available. The nature of the need, whether short-term or long-term, as well as the clinician’s judgment, guides the choice of evaluation (short form or comprehensive) to be conducted with the home-care client [181].
In addition, given the difficulty of developing the last phase of the OCCI with an interoperable solution in the RSIPA, the MSSS has decided to computerize a new version of the OCCIs toward a unique digital health record (DHR). The deployment of this DHR will first be implemented in two initially selected establishments by the end of 2025, before being extended to the entire Quebec based on the lessons learned. The implementation of the DHR will allow for a unique provincial DHR. It will make a person’s health history available throughout Quebec to all authorized professionals. In this way, for secondary care professionals, especially those in hospitals, the OCCIs will provide an opportunity to improve coordination with home and community care. In addition to allowing simultaneous consultation by these professionals for all levels of care, it will enable the client to access their own medical record and to keep track of their appointments [182]. When this new system becomes available, more specific investigations can be conducted to adequately evaluate the innovation outcomes and the long-term effects on the provincial level [183–185].
Nomenclature
-
- ADLs
-
- Activities of daily living
-
- BCT
-
- Behavioral change techniques
-
- BCTT
-
- Behavioral change technique taxonomy
-
- CESS
-
- Centre d’expertise en santé de Sherbrooke
-
- CISSSs
-
- Health and Social Service Centres (French acronym: CISSS for Centre intégré de santé et de services sociaux)
-
- CIUSSSs
-
- Integrated University Health and Social Service Centres (French acronym: CIUSSS for Centre intégré universitaire de santé et de services sociaux)
-
- CFIR
-
- Consolidated Framework for Implementation Research
-
- CGA
-
- Comprehensive geriatric assessment
-
- CH
-
- Hospital center (French acronym: CH for center hospitalier)
-
- CHSLD
-
- Residential and long-term care center (French acronym: CHSLD for Centre d’hébergement de soins de longue durée)
-
- CLSC
-
- Local community service center (French acronym: CLSC for Centres locaux de santé communautaires)
-
- CPEJ
-
- Child and youth protection center (French acronym: CPEJ for Centre de protection de l’enfance et de la jeunesse)
-
- CPR
-
- Computer-based patient record
-
- CR
-
- Rehabilitation center (French acronym: CR for centre de réhabilitation)
-
- DGAPA
-
- Seniors and caregivers directorate of the ministry (French acronym: DGAPA for Direction générale des aînés et des proches aidants)
-
- DGTI
-
- Information technology branch of the ministry (French acronym: DGTI for Direction générale des technologies de l’information)
-
- ERIC
-
- Expert recommendations for implementation of change
-
- HIS
-
- Health information system
-
- IADLs
-
- Instrumental activities of daily living
-
- IC
-
- Integrated care
-
- ICPs
-
- Integrated care pathways
-
- ICT
-
- Information and communication technology
-
- IRLM
-
- Implementation research logic model
-
- IT
-
- Information technology
-
- IS
-
- Information system
-
- MoAs
-
- Mechanisms of action
-
- MSSS
-
- Ministry of Health and Social Services (French acronym: MSSS for Ministère de la Santé et des Services sociaux)
-
- OCCIs
-
- Care pathways (CPs) (French acronym: OCCIs for Outils de Cheminements Clinique Informatisés)
-
- OEMC
-
- Assessment tool (French acronym: OEMC for Outil d’évaluation multiclientèle)
-
- PD
-
- Participatory design
-
- PREM
-
- Patient-reported experience measures
-
- PROM
-
- Patient-reported outcome measures
-
- PSIAS
-
- Planning tool (French acronym for planification des services individualisés et d’allocation de services)
-
- RSIPA
-
- Clinical and management computerized solution (French acronym for Réseau de services intégrés pour les personnes adultes)
-
- SMAF
-
- Functional autonomy measuring system (French acronym: SMAF for Système de mesure de l’autonomie fonctionnelle)
-
- TIDieR
-
- Template for intervention, description, and replication
-
- UTAUT
-
- Unified theory of acceptance and usage of technology
Ethics Statement
The study was approved by the Integrated Health and Social Services Centre (CISSS) Chaudière-Appalaches Research Ethics Board (MP-23-2016-343, MP-2016-016), which acts as the main evaluator for the multicenter research project. The decision of this main Ethics Board also applies to the two other centers. All participants provided written informed consent prior to the individual interviews or questionnaire.
Disclosure
The views expressed in this publication are those of the authors. The funding source had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
Nicole Dubuc is the guarantor of this article. All authors participated in the initiation and development of the study design. They also collected the data and conducted qualitative and cross-case analysis. Afiwa N’Bouke performed statistical analysis. Cinthia Corbin performed analysis of qualitative data. Nicole Dubuc drafted the manuscript; Nicole Dubuc, Afiwa N’Bouke, Cinthia Corbin, and Nathalie Delli Colli contributed to the subsequent drafts and the final version. All authors read and approved the final manuscript and agree to be accountable for all aspects of the work.
Funding
The data collection for this work was conducted within a project financed by the Ministry of Health and Social Services (MSSS) and recognized by the Fonds de recherche du Québec—Santé (FRQS) under Grant Nos. 59354 and 56263.
Acknowledgments
We express our gratitude to all the managers and healthcare professionals who volunteered their time for participation in this study. We would like to acknowledge the collaboration of Isabelle Labrecque and the other MSSS team members, Joanne Guilbeault, former CESS managing director and clinical specialists, with whom they interact and helped with the formal OCCI training.
Supporting Information
Additional file 1_TIDierR OCCI.docx. Description of the OCCIs integrated in the RSIPA system with TIDieR checklist. Additional file 2_2tables_Characteristics of participants.docx. Additional file 3_Influence of determinants.docx. Influence of determinants at each site. Additional file 4_Adaptations provided to RSIPA or to the OCCIs.docx. Adaptations provided to the RSIPA or to the OCCIs according to phases 1-2-3. Additional File 5_Strategies_ERIC with CFIR.docx. Implementation strategies used at the three sites. Additional file 6_3tables_Implementation Outcomes.docx. Implementation Outcomes perceived by Managers and Health-Care Professionals. Additional file 7_Reach_OCCI process and characteristics of home care clients.docx. Reach: Characteristics of home care clients assessed from baseline to 18 months and the OCCI clinical process. Additional file 8_2 tables_OCCI process and fidelity.docx. OCCI process and fidelity. Additional file 9_2tables_The OCCIs outcomes perceived by managers and health care prof.docx. The OCCIs outcomes perceived by managers and healthcare professionals. Additional file 10_5tables_The OCCIs outcomes perceived by clients.docx. OCCI outcomes perceived by home-care clients and their caregivers. Additional file 11_Strategies_ERIC with BCT-MoAs.docx. Strategies with mechanisms of action (MoAs) and BCTs.
Open Research
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due participant confidentiality but are available from the corresponding author upon reasonable request. Please note that the data collected are only available in French.




