Comparison of Optimized Stratified Nursing and Routine Nursing in Patients With Hepatocellular Carcinoma: Effects on Mood State, Sleep Quality, and Life Ability
Abstract
Objective: To study the effects of optimized stratified nursing on mood state, sleep quality, and life ability in patients with hepatocellular carcinoma (HCC).
Methods: From December 2022 to December 2023, 57 patients diagnosed with HCC were in the study and control groups. The control group received routine nursing care, while the study group received optimized stratified care based on ordinary nursing care. The mood states, sleep quality, treatment compliance, nursing satisfaction, and quality of life of the patients in both groups before and after the proposed intervention were observed and compared.
Results: After the intervention, both POMS and PSQI scores for the two groups were significantly reduced (p < 0.05), with the study group showing significantly lower scores than the control group (p < 0.001). There was a significant increase in the ADL score for both the study group and the control group (p < 0.05); the study group, however, was significantly higher than the control group (p < 0.001). The patients in the study group had a higher compliance rate (89.47%) compared with the control group’s compliance rate of 73.68% (p < 0.05). Nursing satisfaction in the study group was rated at 87.72%, significantly higher than that in the control group, at 71.93% (p < 0.05).
Conclusion: Optimized stratified nursing can ameliorate the mood state of patients with HCC, increase their treatment compliance and nursing satisfaction, and improve sleep and quality of life.
1. Introduction
Hepatocellular carcinoma (HCC) is a main malignant tumor of liver cell origin that accounts for 90% of all primary liver cancers [1]. It is a highly fatal cancer that causes about 800,000 deaths worldwide each year. According to the Global Cancer Incidence, Mortality, and Prevalence Survey 2020, HCC is the sixth most common malignant tumor and the third most usual cause of malignant tumor-related deaths worldwide [2]. According to the database, the average rate of 5-year survival for patients with HCC is approximately 19.6% and can be as low as 2.5% when the disease has progressed to advanced metastases [3, 4]. The etiology of HCC varies considerably among different populations. Still, the main high-risk factors include Hepatitis B Virus (HBV) or Hepatitis C Virus (HCV), alcoholic liver disease, nonalcoholic fatty liver disease (NAFLD), and other causes of cirrhosis. The HBV infection without regular therapy is the primary factor for the high incidence of HCC in China [5, 6].
Common modalities of treatment for HCC include ablation, hepatectomy, transcatheter arterial chemoembolization (TACE), radiotherapy, liver transplantation (LT), and systemic therapy [7]. While these therapies very much alleviate advanced-stage HCC cases, many patients are diagnosed with HCC in later stages, confounding treatment options and spelling miserable scenarios for patients. Because of these adversities, there is great need for sophisticated nursing strategies to ameliorate patient care and enhance quality of life [8, 9]. However, the ongoing refinements in surgical techniques and targeted immunotherapy have significantly improved the outcomes of HCC. Still, late prognosis remains poor because about 70% of HCC patients experience recurrence and metastasis early in the postoperative period. Beyond the physical conditions caused by HCC, psychological distress is disabling, prompting depression, anxiety, and mood instability, thus negatively influencing compliance and quality of life [10, 11]. Traditional nursing approaches usually do not meet these intricate needs, necessitating a better model that caters specifically to the issues facing HCC patients.
Optimized stratified nursing is a patient-centered method that delivers individualized care according to the patient’s self-care capacity, psychological condition, and clinical presentation. This model aims to enhance nursing efficiency by categorizing patient care settings into various levels. The ensuing effects are patient-oriented interventions that address both physical and psychological demands [12].
Stratified nursing has been associated with improved patient outcomes, better allocation of healthcare resources, and reduced workload for nursing staff [13, 14]. The concept of stratified nursing also ties psychological support, lifestyle guidance, and structured care plans critical and often needed in managing the emotional distress commonly experienced by HCC patients [15]. Today, when some of the more effective hierarchical models are being employed in nursing with the intent of reinforcing the relevance, completeness, and rationality of nursing measures, their wide application is still being made in the nursing care of many diseases, with obvious success and satisfaction of the client [16, 17].
Despite its benefits, the concept of stratified nursing has not been considerably applied in care delivery to oncology patients. This research focuses on assessing the effectiveness of stratified nursing to see if it enhances mood, quality of sleep, and function in patients with HCC. This study is aimed at assessing the effect of stratified nursing on the improvement of patients’ general conditions, adherence to therapy, and general quality of life of HCC patients.
2. Materials and Methods
2.1. General Information About Patients
Between December 2022 and December 2023, a total of 114 patients with HCC were enrolled to define a control or experimental group, of which 57 were assigned to each. Control group: 32 males and 25 females, ages 40–71 (median age: 48.47 years, SD ± 4.35). Tumor staging distribution: 39 cases in stages I-II and 18 cases in stages III-N. Tumor sizes: < 3 cm, 35 cases and ≥ 3 cm, 22 cases. Study group: 34 males and 23 females, ages 38–72 (median age: 48.62 years, SD ± 4.19). Tumor stage distribution: 38 cases in stages I-II and 19 in stages III-N. Tumor sizes: < 3 cm, 36 cases and ≥ 3 cm, 21 cases. There were no statistically significant differences in baseline characteristics between the groups (p > 0.05).
2.2. Inclusion and Exclusion Criteria
Patients involved in the study were diagnosed as HCC within the criteria of the Norms for diagnosis and treatment of primary liver cancer (2017 edition). Eligible patients had to be between 18 and 75 years old with signed informed consent. Patients with severe heart or kidney dysfunction, other malignancies, immune system dysfunction, or bleeding disorders were excluded. In addition, patients with severe infections, possible psychiatric problems, severe handicaps of one or more limbs, or a hearing or speech impairment interfering with the assessments were also excluded.
2.3. Methods
-
Control group: control patients were treated with routine nursing care involving general health education, psychological counseling, and assistance for relatives. Psychological techniques included simple relaxation techniques and referral to the physician for greater support. Family members were counseled before discharge to aid them in patient communication, thus minimizing potential negative emotions.
-
Study group: patients from the test group received optimized stratified nursing care routinely. Such care consists of systematic grading of care levels based on self-care status, psychological state, and severity of illness.
In the classification system, patients in serious conditions who could not care for themselves received tertiary care, including all-encompassing nursing supervision and advanced psychological support. Secondary care was dedicated to patients with moderate self-care capability; this incorporated regular nursing interventions and tailored psychological support. Patients in relatively stable condition and capable of self-management received primary care, which consisted of self-management education and lifestyle counseling offered in general.
2.3.1. Psychological and Sleep Management
Patients in the control group were given standard nursing care amalgamation of basic psychological counseling, relaxation strategies, and referrals for medical attention situations where there was psychological distress or sleep insufficiencies. In contrast, patients in the study group were offered interventions specific to their psychological assessment scores. Those with moderate distress received personalized counseling, guided relaxation training, and structured education in sleep hygiene. Those in severe distress received a structured program in psychological support and were referred to specialized mental health professionals if warranted.
2.4. Observation Indicators
- 1.
Mood state: the POMS assessed the patients’ psychological state. There were 5 subscales of negative emotions, and the total score of the five items was the total. A higher score means a worse mood state.
- 2.
Sleep quality: the Pittsburgh Sleep Quality Index (PSQI) was used to evaluate the sleep quality of patients, with a total of 18 items and a total score of 21 points. If the score is > 8 points, there is a sleep disorder. And the higher the score, the worse the sleep quality.
- 3.
Daily living ability: the Activity of Daily Living Scale (ADL) was used to assess the patients’ daily living ability. The full score was 100; the higher the score, the better the quality of life.
- 4.
Treatment compliance: the Frankl Compliance Scale (FCS) was used to evaluate the treatment compliance of patients, including regular medication, reasonable diet, and other items. The full score was four points. A higher score means better compliance. The score 3–4 was classified as high compliance, 2 as general compliance, and 0 and 1 as poor compliance. Compliance rate (%) = (high + general)/total cases × 100%.
- 5.
Nursing satisfaction: the Likert Scale was used to conduct the satisfaction survey; the total score is 5 points; 5 points are satisfied, 2–4 points are general, and 2 points and below are dissatisfied. Total satisfaction (%) = (satisfaction + general) cases/total cases × 100%.
2.5. Statistical Methods
All statistical analyses were performed using SPSS 27.0 software. Shapiro–Wilk’s normality test was used to assess the normality of continuous variables. Results for normally distributed data were expressed as the mean ± standard deviation ( ± s) and analyzed using the t-test. In contrast, nonnormally distributed data were reported as the median (interquartile range, IQR) and analyzed using the Mann–Whitney U test. Categorical data were expressed in percentages and compared using the chi-square test (χ2). A p value of < 0.05 was regarded as statistically significant.
3. Results
3.1. Results of Mood States
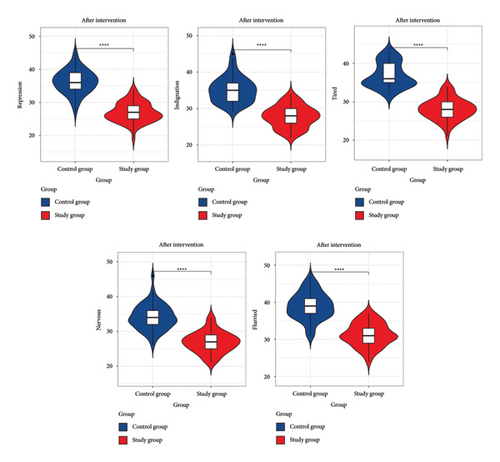
As shown in Table 1 and Figure 1, POMS scores in both groups declined significantly after the intervention (p < 0.05), with the study group being lower than that of the control group (p < 0.001). Note: compared with this group before the intervention, ∗p < 0.05.
| Index | Control group (n = 57) | Study group (n = 57) | t | p | |
|---|---|---|---|---|---|
| Repression | Before intervention | 46.37 ± 4.28 | 45.36 ± 4.13 | 1.268 | 0.207 |
| After intervention | 36.26 ± 3.60 ∗ | 26.95 ± 2.97 ∗ | 15.082 | < 0.001 | |
| Indignation | Before intervention | 45.42 ± 4.55 | 45.44 ± 4.46 | 0.021 | 0.983 |
| After intervention | 35.12 ± 3.52 ∗ | 27.77 ± 2.93 ∗ | 12.130 | < 0.001 | |
| Tired | Before intervention | 57.29 ± 5.04 | 57.40 ± 5.05 | 0.111 | 0.912 |
| After intervention | 36.89 ± 3.22 ∗ | 28.11 ± 2.73 ∗ | 15.713 | < 0.001 | |
| Nervous | Before intervention | 48.05 ± 4.94 | 47.98 ± 4.64 | 0.078 | 0.938 |
| After intervention | 34.09 ± 3.66 ∗ | 26.89 ± 2.99 ∗ | 11.486 | < 0.001 | |
| Flurried | Before intervention | 57.12 ± 5.38 | 57.16 ± 5.32 | 0.035 | 0.972 |
| After intervention | 39.00 ± 3.67 ∗ | 31.25 ± 3.12 ∗ | 12.158 | < 0.001 | |
- ∗p < 0.05, before intervention vs. after intervention.
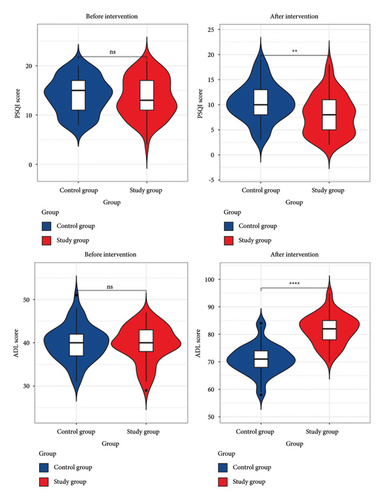
3.2. Results of Sleep Quality and ADL
As demonstrated in Table 2 and Figure 2, the PSQI scores decreased significantly after intervention in both groups (p < 0.05), with the study group again being lower than the control group (p < 0.001). This was in contrast to the ADL scores that increased significantly in both groups (p < 0.05), with the ADL score of the study group being higher than that of the control group (p < 0.001).
| Index | Control group (n = 57) | Study group (n = 57) | t | p | |
|---|---|---|---|---|---|
| PSQI score | Before intervention | 13.98 ± 3.61 | 13.58 ± 4.01 | 0.565 | 0.574 |
| After intervention | 10.45 ± 3.69 ∗ | 8.00 ± 3.95 ∗ | 3.431 | < 0.001 | |
| ADL score | Before intervention | 39.93 ± 4.13 | 39.72 ± 4.14 | 0.272 | 0.786 |
| After intervention | 70.82 ± 5.32 ∗ | 81.75 ± 5.38 ∗ | 10.908 | < 0.001 | |
- ∗p < 0.05, before intervention vs. after intervention.
3.3. Results of Treatment Compliance
Compliance was higher in the study group compared with the control, 89.47% vs. 73.68%, respectively (p < 0.05), as shown in Table 3.
| Index | Control group (n = 57) | Study group (n = 57) | χ2 | p |
|---|---|---|---|---|
| High [n (%)] | 16 (28.07%) | 23 (40.35%) | ||
| General [n (%)] | 26 (45.61%) | 28 (49.12%) | ||
| Poor [n (%)] | 15 (26.32%) | 6 (10.53%) | ||
| Compliance rate [n (%)] | 42 (73.68%) | 51 (89.47%) | 4.728 | 0.030 |
3.4. Comparison of Nursing Satisfaction
Results showed that the satisfaction rate of the study group was 87.72%, which was significantly higher than that of the control group (71.93%, p < 0.05), according to Table 4.
| Index | Control group (n = 57) | Study group (n = 57) | χ2 | p |
|---|---|---|---|---|
| Satisfied [n (%)] | 17 (29.82%) | 24 (42.11%) | ||
| General satisfied [n (%)] | 24 (42.11%) | 26 (45.61%) | ||
| Dissatisfied [n (%)] | 16 (28.07%) | 7 (12.28%) | ||
| Satisfaction rate [n (%)] | 41 (71.93%) | 50 (87.72%) | 4.412 | 0.036 |
4. Discussion
Hepatic cell carcinoma is a type of primary liver cancer that has high mortality in most cases. Recent general use of antiviral drugs has essentially improved the quality of life and prolonged the lifetime in patients with hepatitis and cirrhosis; this decreased the incidence of HCC [18]. Since alcohol long-term consumption or lipid metabolism disorders initiated by economic development are causing a steady climb in HCC incidence, there is continuing concern about its prevention and treatment [19] whereas the standard modes of therapy for the disease include surgery, chemotherapy, and radiotherapy, and while new drugs are being introduced and new therapies set into practice, HCC has not satisfactorily improved prognosis outcomes for its patients [20]. Furthermore, HCC affects great turbulence in the life of the patient, and such distress on the patient easily leads to negative emotions and psychological states. The adherent nature of the patient may be reduced, leading to inferior therapeutic efficacy [21]. That is why some relevant interventions should be done for those patients. Traditional nursing care often fails to provide timely communication, comprehensive psychological support, and adequate health education. This impairs the patient’s quality of survival and prognosis [22]. Optimized stratified nursing covers a range of differentiated needs among patients at various levels and carries out nursing care to meet those needs. This increases the focused nature of nursing and lessens the burdens upon nursing staff while reducing the financial loads imposed on patients [23, 24]. Our study’s findings indicate that optimized stratified care has improved mood, as measured by the deprivation of POMS scores from those of the study group compared with that of the control group (p < 0.001). These successful individualized nursing strategies targeting psychological needs (e.g., counseling focused on patients and tailored interaction procedures) can reduce negative emotions, including depression, tension, and anxiety and allow better treatment outcomes. Other studies have emphasized psychological support similarly to improve mood and emotional wellbeing among cancer patients [25, 26]. Furthermore, our study also indicated that changes in mood state positively affected sleep patterns since patients in the study group were noted to have lower PSQI scores (p < 0.001). These findings correspond with earlier evidence that sleep patterns greatly contribute to emotional stability [27].
Clean and quiet inpatient environments, timely psychological counseling, and moderate exercise are likely responsible for childhood recovery. Other studies also confirm that this minimizes sleep disturbance problems and fosters recovery ability for patients in clinical settings [28, 29]. Optimized stratified care also greatly improved the patient’s daily living activities (p < 0.001), as differed from those high ADL scores in the study group. Structured care plans on physical activity and individualized health education will support patients with physical functioning and confidence to do other daily tasks again. Recent interventions like those cited above have benefited chronic disease patients’ recovery and functional outcomes [30, 31]. In addition, our study found the treatment-adhesion rate of the study group to be significantly higher than that of the control group (89.47% vs. 73.68%; p < 0.05). Improved treatment compliance may have occurred due to increased communication, active participation of family members, and regular checks on patients’ physical and psychological states. Previous studies have highlighted that personalized nursing care is a great motivator in promoting adherence to the treatment regime, especially in oncology settings [32]. The satisfaction rate was also significantly higher in the study group (87.72% vs. 71.93%, p < 0.05), thus underlining patient-centered care as a key to building trust and confidence in healthcare services. Such targeted nursing interventions that cater to patient’s medical and emotional needs were found to bring about a positive experience for patients, which also agree with findings on comparable nursing care models [33]. While our study sheds light on the positive sides of timely nursing, it is well worth mentioning that being descriptive in nature puts a limit yet again on the causal perspective in any case of an intervention toward an outcome in this particular case: longitudinal studies or randomized controlled trials can elucidate causative inferences of the findings therein. Furthermore, the glaring omission in this study on some potential mediators, especially systemic inflammation and socioeconomic variables, prevents the brilliance of the research from actually coming out. Future studies should address the role of these covariates to adequately explore the rich interactions among mood, adherence patterns, and health outcomes in HCC patients.
5. Conclusion
A well-stratified nursing intervention model substantially impacted patients with HCC, improving their mood state, treatment compliance, sleep quality, and overall quality of life. It seeks to address psychological and physical needs in a personalized way, making it a good candidate for enhancing clinical outcomes. Its promotion into practice, especially in oncology care, is recommended. It will be beneficial if future studies can define the long-term benefits further and consider other mediating factors that could lead to further refinements in their applicability.
Ethics Statement
All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Ethics Committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, approves this study. Written informed consent was obtained.
Consent
Informed consent was obtained from all individual participants included in the study.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
Luhong Hu: guarantor of integrity of the entire study.
Lisi Zhu: study concepts, study design, clinical studies, data acquisition, data analysis, statistical analysis, manuscript preparation, manuscript editing, and manuscript review.
Rongrong Li: definition of intellectual content and literature research.
Funding
The authors have nothing to report.
Open Research
Data Availability Statement
The simulation experiment data used to support the findings of this study are available from the corresponding author upon reasonable request.




