Application Analysis of Self-Intervention in Patients With Cancer Complicated With Diabetes Based on Behavioral Theory
Abstract
Background and Objective: Managing diabetes in cancer patients presents unique challenges, necessitating effective self-intervention strategies. The research aimed to evaluate self-intervention behaviors in diabetic cancer patients. The Information-Motivation-Behavioral Skills (IMB) paradigm serves as the guidance.
Methods: This qualitative cross-sectional investigation was conducted in general hospitals throughout China from March 14 to April 25, 2024. It involved 300 patients diagnosed with cancer and type 2 diabetes, using a structured questionnaire to assess diabetes knowledge, self-management behaviors, family support, and self-efficacy.
Outcomes: The participants had a mean age of 69.14 ± 23.04 years, with a diabetes duration of 23 ± 7.7 years. The research discovered notable variations in medical evaluations and self-management practices (such as retinal examinations and blood pressure checks) (p < 0.05). Family assistance had a mean score of 16.60 ± 7.40 (p = 0.029), and knowledge of diabetes scored 11.40 ± 4.25 (p < 0.001). Additionally, diabetes-related emergencies, skin infections, and heart incidents increased significantly during the year following a cancer diagnosis.
Conclusion: The research highlights the complexity of diabetes treatment for cancer patients and underscores the necessity of focused interventions to enhance self-monitoring and capitalize on family support.
1. Introduction
Cancer, a complex group of malignant diseases, is characterized by uncontrolled proliferation of abnormal cells that invade surrounding tissues and metastasize to distant body parts [1]. With rising incidence and death rates around the globe, cancer poses a serious threat to global health. According to data, approximately 10.3 million people died from cancer, and 19.3 million people were diagnosed with the disease globally from the Global Cancer Observatory (GLOBOCAN) 2020. The most prevalent malignancies are those of the breast, lungs, colon, and prostate. By 2040, it is anticipated that there will be 28.4 million instances of cancer worldwide [2]. Cancer has become a major source of illness and mortality in China, with important public health ramifications. According to 2022 estimates [3], China recorded approximately 2.574 million cancer-related deaths, with 4.825 million new cancer cases diagnosed in the same year.
The intersection of cancer and diabetes presents a unique and challenging landscape for both patients and healthcare providers. Globally, diabetes and cancer are two of the most common chronic illnesses, often occurring together in affected individuals. Recent statistics indicate that approximately 8%–18% of cancer patients also suffer from diabetes, a comorbidity that complicates treatment and prognosis [4]. Given that obesity is a shared risk factor for both disorders and the population is aging, the co-occurrence of these diseases is projected to increase [5, 6]. As the population ages and given that weight gain is an elevated aspect for both disorders, it is anticipated that their co-occurrence will increase [5, 6].
It is crucial to treat diabetes in cancer patients, as fluctuations in blood glucose levels can adversely affect cancer treatment efficacy and increase the risk of complications. Therefore, understanding how these patients engage in self-intervention behaviors is essential for developing targeted interventions that can improve health outcomes [7, 8]. In this context, self-intervention, guided by robust theoretical frameworks, becomes crucial in managing both diseases effectively. According to the Information-Motivation-Behavioral Skills (IMB) model, which was initially created to comprehend behaviors connected to health, behavioral skills, motivation, and knowledge are key factors that influence changes in health behavior and can be helpful in the management of this illness [9].
Because infections at the surgical site were common in gastrointestinal surgeries, antimicrobial prophylaxis was required [10]. It discovered small variations among single- and multiple-dose antibiotics and concluded that these antibiotics are more effective antibiotics. More trials are required for individuals with throat cancer.
Although both illnesses are becoming more common, there is little study that simultaneously addresses self-intervention strategies in patients suffering from both cancer and diabetes. Therefore, the research aimed to examine cancer survival and diabetes patients’ self-intervention behaviors, directed by the IMB model.
2. Methodology
2.1. Study Design and Setting
This research was a descriptive analysis that is cross-sectional conducted at several general hospitals in China from March 14 to April 25, 2024. The study was designed to understand variations in diabetes self-management, family support, self-efficacy, and knowledge among cancer survivors with diabetes.
2.2. Participants
-
Inclusion criteria: Individuals who have been diagnosed with T2DM for at least 20 years and have also been diagnosed with cancer (18 years of age or older). Participants must be able to read and comprehend the questionnaire and provide informed acceptance in their preferred language.
-
Exclusion criteria: An incomplete questionnaire, no diagnosis of diabetes, and an inability to give informed consent due to impaired cognition were among the exclusion criteria.
2.3. Data Collection
The study employed a structured questionnaire consisting of 95 questions. These included 22 questions about general traits, diabetes knowledge (23), attitudes toward self-intervention (14), self-intervention practices (17), self-efficacy (11), and family support (eight). Two professors of adult nursing, one diabetes education nurse, and two endocrinologists validated the questionnaire items that were modified for the research.
Four trained research assistants administered the questionnaire, and following an explanation of the research objectives and procedures, participants gave their informed permission. Participants completed the questionnaire individually, with assistance provided to those who needed help with reading and writing. The process took approximately 25 min per questionnaire, and data were stored securely without any identifiable patient information.
The general characteristics section included 22 questions covering demographic and lifestyle variables such as age, gender, educational attainment, cohabitation status, comorbidities, smoking habits, alcohol intake, and exercise frequency. These questions aimed to capture a holistic view of the participants’ backgrounds and health-related behaviors.
The diabetes knowledge assessment tool was used to evaluate diabetes knowledge, with 34 questions covering basic knowledge, treatment objectives, nutrition, hypoglycemia, complications, and insulin usage. Insulin-related questions were excluded due to a lack of knowledge among some participants. The Cronbach’s α for this research was 0.80, compared to 0.93 for the original tool.
The Diabetes Family Behavior Checklist II, which had two narrative items, eight questions about negative support, and ten questions about positive support, was used to evaluate family help. Positive support items were validated by experts and assessed using the 5-point Likert scale, where 1 denotes “never” and 5 denotes “at least once today.” Cronbach’s α was 0.91 in this research, compared to 0.80 in the original.
The diabetes psychology scale’s validity and reliability are established, with five domains analyzed into four components. Using a 5-point Likert scale, this research included 9 questions on patient autonomy and 4 questions on rigorous glycemic control (“strongly disagree” to “strongly agree”). Cronbach’s α for patient autonomy and glycemic control was 0.80 and 0.72, respectively, with 0.71 and 0.80 in this study.
The nine-item diabetic self-efficacy measuring tool was used to gauge self-efficacy assessing confidence in managing diabetes, blood glucose monitoring, diet, and exercise. A score on the scale ranges from 1 (“not at all confident”) to 10 (“completely confident”), with higher scores indicating a higher level of self-efficacy. In the study, the initial Cronbach’s α values were 0.92 and 0.97.
The 23 items in the diabetic self-intervention evaluation report tool have been verified by professionals, which measured self-intervention behaviors. It used nominal and multiple-response scales, with 13 items analyzed on a 4-point Likert scale, resulting in a Cronbach’s α of 0.91.
The self-efficacy and type 2 diabetes self-intervention assessment’s primary components are summarized in Table 1, which also shows the number of questions and their particular areas of focus. General characteristics, diabetes information, support from relatives, self-esteem, self-intervention actions, and psychological aspects such as patient autonomy and glucose management are all covered in these sections.
| Section | Number of questions | Focus |
|---|---|---|
| General characteristics | 22 | Demographic and lifestyle variables: age, gender, educational attainment, cohabitation status, comorbidities, smoking habits, alcohol intake, exercise frequency. |
| Diabetes knowledge | 23 | Basic diabetes knowledge, treatment objectives, nutrition, hypoglycemia, complications, insulin usage (insulin-related questions excluded). |
| Family support | 10 | Positive and negative family support, including narrative items. |
| Self-efficacy | 11 | Confidence in managing diabetes, blood glucose monitoring, diet, and exercise. |
| Self-intervention activities | 17 | Diabetes self-management behaviors, including adherence to treatment, monitoring, diet, and exercise. |
| Diabetes self-intervention report | 23 | Nominal and multiple-response items on self-intervention behaviors were analyzed on a 4-point Likert scale. |
| Psychological aspects | 4 (glycemic control) and 9 (patient autonomy) | Assessment of patient’s strict glycemic control and autonomy in diabetes management. |
Cancer, including pancreas and breast cancers, can have a variety of effects on diabetes self-care. Pancreatic cancer may affect the creation of insulin, making controlling blood sugar more difficult, while breast cancer treatments can impact intake and activity levels, making diabetes harder to manage. Specific therapy strategies should take these cancer-specific concerns into account.
2.4. Ethical Considerations
The Institutional Review Board of the collaborating hospitals provided ethical clearance for the research. All participants were informed about the goals, methods, possible hazards, and advantages of the study before giving their informed permission. Participants were reassured that their responses would be kept confidential.
2.5. Statistical Analysis
Version 26 of IBM SPSS Statistics was used to analyze the data. A multivariate regression model and descriptive statistical methods were employed for collecting participants’ clinical and demographic details and traits. Independent t-tests and chi-square (χ2) tests were used to compare the groups’ knowledge of diabetes, attitudes toward self-management, family support, self-efficacy, and self-intervention practices. For every statistical test, a significance threshold of p < 0.05 was established.
3. Results
As Table 2 shows, the participants had a mean age of 69.14 ± 23.04 years and a mean diabetes duration of 23 ± 7.7 years. There were 155 women (51.7%) and 145 men (48.3%) among the participants. Regarding education, 178 participants (59.3%) had completed 10 or more years of school. Regarding living arrangements, 60 participants (25.0%) lived alone. The diabetes treatment modalities included oral hypoglycemic agents (OHAs) for 208 participants (69.3%), insulin for 12 participants (4.0%), insulin plus OHA for 44 participants (14.7%), and lifestyle modification alone for 36 participants (12%). Comorbidities were present in 204 participants (68%). Experience in diabetes education was reported by 147 participants (49.0%), while 153 participants (51.0%) had no such experience. Regular exercise was practiced by 136 participants (45.3%), with 164 participants (54.7%) not engaging in regular exercise. Heavy drinking was reported by 21 participants (7%). Diabetes complications were present in 76 participants (25.3%), while 224 participants (74.7%) had no complications. Additionally, current smoking was observed in 32 participants (10.7%).
| Characteristics | Number | Percentage |
|---|---|---|
| Age (mean ± SD) | 69.14 ± 23.04 | |
| Duration of diabetes (mean ± SD) | 23 ± 7.7 | |
| Sex | ||
| Male | 145 | 48.3% |
| Female | 155 | 51.7% |
| Education (years) | ||
| 0–6 | 60 | 20.0% |
| 7–9 | 62 | 20.7% |
| 10 or more | 178 | 59.3% |
| Cohabitants | ||
| Yes | 240 | 75.0% |
| No | 60 | 25.0% |
| Diabetes treatment | ||
| OHA | 208 | 69.3% |
| Insulin | 12 | 4.0% |
| Insulin plus OHA | 44 | 14.7% |
| Only lifestyle modification | 36 | 12% |
| Comorbidity | ||
| Yes | 204 | 68% |
| No | 96 | 32% |
| Experience in diabetes education | ||
| Yes | 147 | 49.0% |
| No | 153 | 51.0% |
| Regular exercise | ||
| Yes | 136 | 45.3% |
| No | 164 | 54.7% |
| Heavy drinking | ||
| Yes | 21 | 7% |
| No | 279 | 93% |
| Complication of diabetes | ||
| Yes | 76 | 25.3% |
| No | 224 | 74.7% |
| Current smoking | ||
| Yes | 32 | 10.7% |
| No | 268 | 89.3% |
In a multivariate regression model, you could examine the influence of several factors, such as the impact of diabetes knowledge, self-efficacy, and family support on the self-management practices of diabetic cancer patient. Where the dependent variable is self-management, and the predictor variables are diabetes knowledge, family support, and self-efficacy.
Table 3 suggests that the level of education, strong family support, increase in self-confidence, and participation in diabetes education programs positively affect individuals’ ability to manage their condition. Factors like age, type of treatment, presence of other diseases, and exercise habits do not seem to exert much influence over self-management outcomes.
| Variable | B | SE | T value | p value | 95% CI (lower, upper) | Self-management (dependent variable) |
|---|---|---|---|---|---|---|
| Age | 0.01 | 0.02 | 0.56 | 0.576 | (−0.03, 0.05) | No significant effect |
| Sex (female = 1) | 0.12 | 0.10 | 1.20 | 0.231 | (−0.07, 0.31) | No significant effect |
| Education (years) | 0.03 | 0.01 | 3.42 | < 0.001∗ | (0.01, 0.05) | Positive effect on self-management |
| Diabetes treatment (OHA) | −0.04 | 0.10 | −0.40 | 0.690 | (−0.23, 0.15) | No significant effect |
| Comorbidity (yes = 1) | −0.08 | 0.08 | −1.00 | 0.318 | (−0.23, 0.07) | No significant effect |
| Family support | 0.15 | 0.05 | 2.89 | 0.004∗ | (0.05, 0.25) | Positive effect on self-management |
| Self-efficacy | 0.20 | 0.07 | 2.86 | 0.005∗ | (0.07, 0.33) | Positive effect on self-management |
| Exercise (yes = 1) | 0.09 | 0.09 | 1.00 | 0.317 | (−0.09, 0.27) | No significant effect |
| Diabetes education (yes = 1) | 0.18 | 0.08 | 2.25 | 0.025∗ | (0.02, 0.33) | Positive effect on self-management |
- ∗means, p value < 0.05.
Table 4 and Figure 1 show the retinal examination blood pressure measurement, the HbA1c test, the microalbumin urea test, and other diabetes-related screening and management indicator test completion rates over 1 year. Among the 300 cancer patients assessed, 221 (73.6%) completed retinal examinations, demonstrating a statistically significant variation (p < 0.001). Blood pressure checks were completed by 283 (94.3%) of the participants, a finding that is statistically significant (p = 0.013). The HbA1c test was completed by 273 (91.0%) of the patients, indicating a statistically significant difference (p < 0.001). Additionally, the microalbumin urea test was completed by 278 (92.7%) of the participants, with a result that is statistically significant (p = 0.001).
| Characteristics | N (%) | x2 or t | p |
|---|---|---|---|
| Retinal examination | 221 (73.6) | 19.045 | < 0.001 |
| Foot examination | 79 (26.3) | 3.643 | 0.159 |
| Lipid battery test | 258 (86.0) | 0.173 | 618 |
| Blood pressure check | 283 (94.3) | 6.258 | 0.013 |
| HbA1c test | 273 (91.0) | 23.635 | < 0.001 |
| Microalbumin urea test | 278 (92.7) | 12.787 | 0.001 |
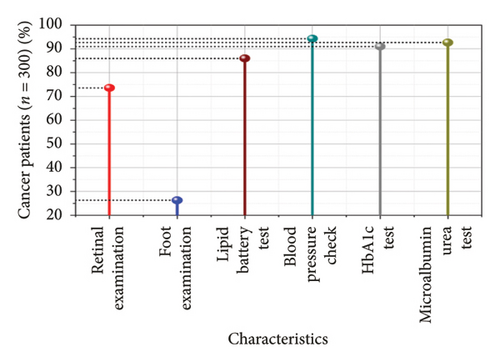
Table 5 illustrates the diabetes-related attitude, knowledge of diabetes, family assistance, and self-efficacy among patients with cancer complicated by diabetes. Regarding motivation, the mean score for the diabetes-related attitude concerning the value of rigorous glucose control was 4.20 ± 0.46 (p < 0.001). In the realm of information, knowledge about diabetes had a mean score of 11.40 ± 4.25, demonstrating statistical significance (p < 0.001). Specific areas like treatment targets and general knowledge scored 0.46 ± 0.58 and 2.86 ± 1.65, respectively (p < 0.001). Hypoglycemia awareness scored 1.39 ± 1.14, significantly different (p < 0.001), while dietary knowledge had a mean of 1.30 ± 1.11, with significance (p = 0.021). Complication awareness was also significant, with a mean score of 4.35 ± 1.78 (p < 0.001). Family assistance, crucial for self-management, had a mean score of 16.60 ± 7.40 and was statistically significant (p = 0.029).
| Features | Mean ± Sd | x2 | p |
|---|---|---|---|
| Inspiration | |||
| Diabetes-related attitude (0–10) | |||
| The value of rigorous glucose control | 4.20 ± 0.46 | 1.819 | < 0.001 |
| Autonomy of the patient | 4.10 ± 0.58 | 1.917 | 0.079 |
| Family assistance (10–30) | 16.60 ± 7.40 | 3.867 | 0.029 |
| Information | |||
| Knowledge (0 ∼ 20) | 11.40 ± 4.25 | 7.263 | < 0.001 |
| Treatment target | 0.46 ± 0.58 | 6.950 | < 0.001 |
| General knowledge | 2.86 ± 1.650 | 6.854 | < 0.001 |
| Hypoglycemia | 1.39 ± 1.14 | 3.570 | < 0.001 |
| Diet | 1.30 ± 1.11 | 4.358 | 0.021 |
| Complication | 4.35 ± 1.78 | 3.845 | < 0.001 |
| Behavioral skills | |||
| Behavioral skills | 47.39 ± 18.88 | 1.786 | 0.069 |
In terms of blood glucose examinations, 133 participants (44.3%) rarely monitored their levels, while 87 (29%) did so occasionally, and 80 (26.7%) frequently, with no significant statistical difference (p = 0.169). Foot exams were conducted frequently by 177 participants (59%), occasionally by 83 (27.7%), and not at any time by 40 (13.3%), showing a statistically significant difference (p < 0.001). Regarding meal-skipping behavior, 223 participants (74.3%) infrequently skipped meals, 12 (4%) did so occasionally, and 65 (21.7%) frequently, with no significant difference (p = 0.058). The presence of diabetes identification tags was noted in 125 participants (41.7%), while 175 (58.3%) did not have them, with no significant difference (p = 0.484). The results related to fatty meal consumption, glucometer use, and overeating were not statistically significant (Table 6 and Figure 2).
| Characteristics | Class | Number (%) | t or x2 | p |
|---|---|---|---|---|
| What is your frequency of blood glucose examinations? | Rarely | 133 (44.3) | 5.789 | 0.169 |
| Occasionally | 87 (29) | |||
| Frequently | 80 (26.7) | |||
| What is the frequency of your foot exams? | Not at any time | 40 (13.3) | 17.143 | < 0.001 |
| Occasionally | 83 (27.7) | |||
| Frequently | 177 (59) | |||
| How frequently do you skip meals? | Infrequently | 223 (74.3) | 6.081 | 0.058 |
| Occasionally | 12 (4) | |||
| Frequently | 65 (21.7) | |||
| Do you have a tag identifying your diabetes? | Yes | 125 (41.7) | 0.925 | 0.484 |
| No | 175 (58.3) | |||
| Do you eat fatty meals frequently? | Infrequently | 185 (61.7) | 0.076 | 0.957 |
| Occasionally | 75 (25) | |||
| Frequently | 40 (13.3) | |||
| Do you check your blood glucose with a glucometer? | Yes | 130 | 0.457 | 0.183 |
| No | 170 | |||
| Do you overeat frequently? | Infrequently | 225 (75) | 6.819 | 0.062 |
| Occasionally | 50 (16.7) | |||
| Frequently | 25 (8.3) | |||
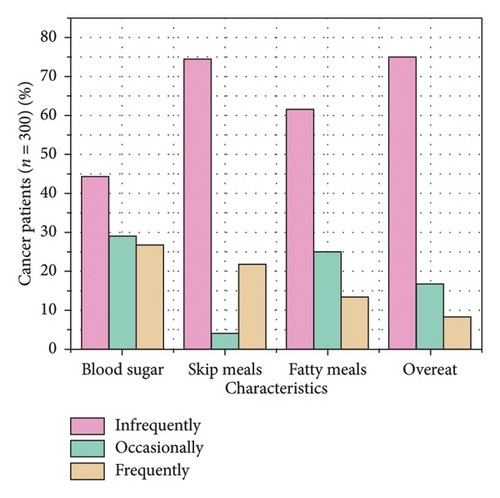
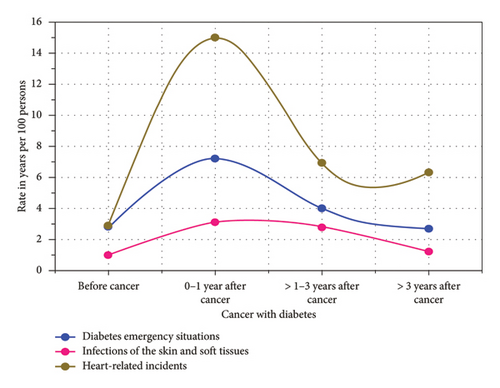
Table 7 and Figure 3 illustrate the rates of significant health outcomes, specifically diabetes emergencies, soft tissue and skin infections, and heart-related incidents, among patients with cancer complicated by diabetes, presented per 100 person-years. Initially, before cancer diagnosis, the rates were relatively low, with diabetes emergencies at 2.8, skin and soft tissue infections at 1.0, and heart-related incidents at 2.9. However, in the first year following a cancer diagnosis, these rates significantly increased to 7.2, 3.1, and 15.0, respectively. In the subsequent period of one to 3 years after cancer, the rates decreased to 4.0 for diabetes emergencies, 2.8 for infections, and 6.9 for heart-related events. More than 3 years post-cancer, the rates further decreased to 2.7, 1.2, and 6.3.
| Cancer with diabetes | The rate in years per 100 persons |
|---|---|
| Before cancer | |
| Diabetes emergency situations | 2.8 |
| Infections of the skin and soft tissues | 1.0 |
| Heart-related incidents | 2.9 |
| 0-1 year after cancer | |
| Diabetes emergency situations | 7.2 |
| Infections of the skin and soft tissues | 3.1 |
| Heart-related incidents | 15.0 |
| > 1–3 years after cancer | |
| Diabetes emergency situations | 4 |
| Infections of the skin and soft tissues | 2.8 |
| Heart-related incidents | 6.9 |
| > 3 years after cancer | |
| Diabetes emergency situations | 2.7 |
| Infections of the skin and soft tissues | 1.2 |
| Heart-related incidents | 6.3 |
4. Discussion
The present research’s examination of insulin resistance handling methods correlates using present literature that shows the value of routine medical exams. For example, regular HbA1c level tracking drastically improved controlling diabetes outcomes for individuals with multiple illnesses, according to the research by Rodríguez-Gutiérrez et al [11]. Higher completion rates for cardiac checks and retinal exams support findings by Kuo et al. and Belew et al., which demonstrated that the more frequently patients with diabetes underwent these evaluations, the more stable their condition became [12, 13]. The relationship between these studies highlights the significance of healthcare monitoring for diabetes management, especially for patients with co-occurring conditions such as cancer.
Significant satisfaction rates for diabetes-related testing were reported in the current study, indicating that a cancer environment may increase patient motivation to follow health management guidelines. This contrasts with the findings by Ko and Lee. According to their research, diabetes awareness, glucose control comprehension, and family support were all lower among cancer survivors. In contrast with individuals with diabetes alone and those without cancer, cancer survivors have particular psychological and emotional difficulties that increase their knowledge and pressure regarding their health, which could account for the variations in results. This emphasizes the necessity of individualized approaches taking into account the unique situations and driving forces of various patient populations [14].
To enhance adherence to self-management and promote the family’s and individual’s health, supportive family members can help individuals with food preparation, notification of medications, glucose tracking, and physical activity [15]. The importance of family for managing diabetes was a different significant outcome of the research. The advantages of family support align with studies by Hu et al. and Wong et al., which discovered that medication adherence was enhanced by family engagement in diabetes management and promoted diabetes self-management [16, 17].
In addition, the elevated prevalence of unfavorable health consequences, like diabetes crises and heart-related events after a cancer diagnosis, underscores the heightened health hazards encountered by this demographic. This finding aligns with Oh et al.’s research [17], which demonstrated that patients with comorbid cancer and diabetes have a significantly higher likelihood of developing cardiovascular disease [18]. According to an investigation by Zhu and Qu [18], diabetes-related complications are made worse by the detection and therapy of cancer. Cancer-induced physical strain and altered metabolism are most likely responsible for this. These results highlight the need for integrated healthcare strategies that address cancer and diabetic treatment holistically [19]. Girnyi et al. [20] suggested that mixed prehabilitation therapy could serve as an effective treatment approach for GI cancer patients undergoing surgery. It was able to identify this method of treatment as a potential contributor to improved recovery and less hospital time. Nevertheless, the scientists still lack complete comprehension of the interactions of the components, the role of immune nutrition, and the necessity for larger studies to perfect the protocols and to create standard outcome measures. 80,193 intestinal cancer patients from 8 European and Asian nations were analyzed, and the results showed that T2DM was 14.8% common among individuals with cancer. There were major variations among the countries, in gastrointestinal and rectal tumors creating the highest prevalence [21].
Diabetes management in patients with cancer is a very complex issue, requiring self-intervention behaviors, family support, and education to significantly improve self-management outcomes. Through the application of a multivariate regression model complemented by independent t-tests, chi-square (χ2) analyses, and descriptive statistics, this study identifies key predictors of self-care behaviors. This approach resolves the prevailing limitation in previous research, which failed to comprehensively integrate psychological, social, and behavioral determinants into the analytical framework. The suggested model makes sure that the interventions are personalized to the specific needs of the individual; thus, it is not only the medical treatment that is being considered but also factors such as self-efficacy and family support. Moreover, while the research examines outcomes like foot exams, diabetes knowledge, and situations, it also touches on routine management gaps and underscores the need for targeted educational programs, which in effect enhance long-term patient care. Healthcare professionals may create caregiver education programs, offer family-focused interventions, and encourage family members to actively participate in treatment plans to bring family support into diabetes care. Providing caregivers with tools like emotional support and insulin resistance treatment instruction can enhance results and promote team-based care.
5. Conclusion
This research assessed the self-management of diabetes, family support, self-efficacy, and knowledge about T2DM in cancer survivors. A total of 300 patients were enrolled, and a systematic questionnaire was employed to gather demographic data, knowledge of diabetes, self-management practices, family support, and self-efficacy. According to the multivariate regression analysis, improved self-management behaviors were found to be significantly associated with higher education, strong family support, and self-learned knowledge through participation in education programs themselves, while age, type of treatment received, comorbidities, and exercise habits did not show any notable effects. The key findings revealed that while a high percentage of participants received essential diabetes preventive screenings—such as retinal exams and HbA1c tests—foot examinations were less consistently requested. Family support and knowledge about diabetes were highly correlated with better self-management outcomes. This is a significant reflection of the need for education and family involvement in managing diabetes in cancer patients.
6. Limitations and Future Scope
- •
The cross-sectional research design does not support making any cause-and-effect statements or longitudinal changes. Targeting a general hospital in China does not generalize well for all cancer-diabetes patients. Further, using self-reported data may cause bias generally through recall or social desirability issues.
- •
Future research could see longitudinal designs applied to the long-term effects of self-intervention behaviors and changes over time. The research should engage broader populations from different regional areas to increase generalizability. Further research may assess specific intervention strategies for enhancing patient outcomes such as reduced complications.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
Min Jiang: conceptualization, methodology, writing – original draft, and project administration. Yunlan Jiang: investigation, resources, and supervision. Xianglong Li: software, validation, and writing – review and editing. Heng Duan: data curation, formal analysis, methodology, and writing – review and editing. Jing Shi: funding acquisition, methodology, supervision, writing – review and editing, writing – original draft, and project administration.
Funding
This work was supported by the Construction of a Clinical Practice Evaluation System for the Master of Traditional Chinese Medicine Nursing Degree Based on Mini-Clinical Practice Evaluation, No. 2023YB32, funded by a research project on the reform of postgraduate education and teaching of Chengdu University of Traditional Chinese Medicine in 2023.
Acknowledgments
Our sincere gratitude goes out to everyone who contributed their time, effort, and expertise to make this study a success.
Open Research
Data Availability Statement
All data are included in the manuscript and uploaded files.




