Influencing Factors of Breast Cancer Patients’ Return-to-Work: A Systematic Review and Meta-Analysis
Abstract
Purpose: The purpose of this study is to recapitulate the influencing factors of breast cancer patients’ return-to-work (RTW).
Methods: Pairs of researchers screened and extracted data from included studies independently. Data were analyzed by using Stata 12.0 Software. The odds ratios (ORs) with 95% confidence intervals (CIs) in the study were used to combine the data, and between-study heterogeneity was investigated by using I2 statistics. Sensitivity analyses were carried out through a step-by-step exclusion of the literature. Funnel plots were employed for a quantitative assessment of publication bias in the included literature.
Results: 23 identified studies were eligible for this synthesis. The pooled incidence of RTW was 65.0%. The factors associated with RTW of breast cancer patients were as follows: age, receipt of radiotherapy or not, presence of comorbidities or not, cancer stage, receipt of axillary lymph node dissection or not, surgical modality, having children or not, anxiety symptoms, work patterns, cognitive functioning, and physical functioning.
Conclusion: Addressing the identified barriers and strengthening the facilitators to RTW can further improve the RTW rates of breast cancer patients and then promote early reintegration into society.
Summary
- •
What is already known about the topic?
- ◦
Introduction: Breast cancer is one of the most prevalent malignancies affecting women worldwide. The array of treatments, from surgery to chemotherapy and radiation therapy, leads to physical discomfort, psychological stress, and an extended recovery period for patients.
- ◦
Current Research Status: Numerous studies have delved into the complex factors affecting breast cancer patients’ RTW. However, there were disparities in sample sizes, methodologies, and conclusive findings.
- ◦
Psychosocial and Physical Impact: Some studies emphasized the psychological aspects, such as anxiety and depression, while others focused on the physical conditions and recovery post-treatment.
- ◦
Key Factors: Individual work environment, social support, and cultural differences significantly shape the process of RTW for breast cancer survivors.
- ◦
Research Gap: Although there was a large body of research demonstrating the factors associated with the RTW of breast cancer patients, the results of the current literature suggested that the incidence of RTW varies among breast cancer patients, and the dispersion of factors affecting the RTW of breast cancer patients across different studies has also led to inconclusive or inconsistent findings. This meta-analysis aimed to bridge these gaps by combining existing studies and synthesizing the different influencing factors. The objective is to provide a stronger basis for understanding the complex dynamics involved in the RTW of breast cancer patients.
- •
What does this paper add?
- ◦
This paper provides up-to-date estimates of the pooled incidence of RTW of breast cancer patients, which was 65.0% (95% CI: 55.0%–75.0%). Factors including age, receipt of radiotherapy or not, presence of comorbidities or not, cancer stage, receipt of axillary lymph node dissection or not, surgical modality, having children or not, anxiety symptoms, work patterns, cognitive functioning, and physical functioning are associated with RTW of breast cancer patients.
- ◦
This meta-analysis offers a comprehensive synthesis and critical evaluation of existing research on the factors influencing breast cancer patients’ RTW.
1. Introduction
Breast cancer (BC) is one of the most common malignant tumors, with its incidence steadily increasing at an average rate of 0.5% annually over the past decade. This consistent rise has contributed to a growing number of BC [1–3]. According to the latest statistics from the International Agency for Research on Cancer (IARC) in 2020 [4], BC has emerged as the world’s most prevalent cancer, surpassing lung cancer, with a recorded 2.26 million new cases, accounting for 11.7% of all cancer cases [5, 6].
Studies have indicated a concerning trend where an increasing number of BC patients are being diagnosed at younger ages, with the majority of BC patients of working age at the time of diagnosis [7, 8]. A cross-sectional review of BC patients in the United States reported that the median age of BC patients at diagnosis during 2004–2016 is 61 years, which is younger than retirement age [9]. This phenomenon is even more pronounced in Asian countries, as indicated by the latest WHO data from 2020, which shows that older people account for only about one-third of female BC cases in China (35.3%) and South Korea (29.8%) [10, 11]. Over recent years, advancements in medical technology and treatment modalities have substantially improved survival rates among BC patients. The American Cancer Society’s 2022 update on female BC statistics shows a significant decline in female BC death rates between 1989 and 2020, with a 43% reduction in mortality, which corresponds to approximately 460,000 fewer deaths over this period [1]. As advances in cancer diagnosis and treatment modalities have improved patient survival rates, there is a growing emphasis on researching post-treatment rehabilitation of BC patients [12]. Long-term cancer treatment severely impacts their original work trajectory, and they are 1.37 times more likely to be unemployed after cancer treatment than the general population [13].
Return-to-work (RTW) refers to the process of resuming work responsibilities after leaving work due to injury or illness [14]. For individual cancer patients, RTW helps them return to normal life; for the country and society, RTW can enhance the social labor force and promote economic development [15]. RTW serves as an important indicator of their full recovery [16]. During BC treatment, patients often need to undergo surgeries, radiotherapy, or chemotherapy. Consequently, following the conclusion of their treatment, many patients aspire to reintegrate into the workforce [17]. RTW aids in rebuilding stability in their daily lives and self-identity and positively influences their social interactions and economic status [18, 19].
The concept of RTW was first introduced in the 1960s and initially focused on individuals recovering from work-related injuries or illnesses. Over time, its scope has expanded to include a broader range of individuals, eventually extending to cancer patients [20, 21]. Research on the RTW process for cancer patients, particularly BC survivors, began in developed countries, such as in Europe and the United States. In the 1990s, the United States and Canada made early efforts to create a more supportive work environment for women with postoperative BC, collaborating with various sectors to guide RTW practices [22]. Recent studies have built upon these earlier efforts by recognizing the growing importance of RTW for cancer survivors, particularly as advancements in cancer treatment and survival rates have improved. These studies have shifted the focus from purely physical recovery to include psychosocial factors such as emotional well-being, social support, and the work environment, all of which play critical roles in determining successful RTW outcomes for BC survivors [23, 24].
To our knowledge, there is currently no updated meta-analysis that comprehensively explores the multifaceted factors that influence RTW outcomes in BC patients. While many individual studies have examined the physical, psychological, and social factors that influence RTW in BC patients, the innovation of this study is the integration of these different factors into a single analysis. This paper considers the combined impact of treatment-related factors, psychosocial factors, and the work environment, with the aim of gaining a more comprehensive understanding of the challenges faced by BC survivors in returning to work.
This study aimed to conduct a meta-analysis to systematically review the existing literature and integrate the various factors affecting BC patients’ RTW to provide a more comprehensive understanding and guidance for facilitating BC patients’ RTW.
2. Methods
2.1. Protocol Registration
The protocol for this review has been registered with PROSPERO under the reference number CRD42023434406 (in Supporting Information (available here)).
2.2. Search Strategy
Eight databases (PubMed, Cochrane Library, EMBASE, CINAHL, Web of Science, China National Knowledge Infrastructure (CNKI), WanFang Data Knowledge Service Platform, and China Science and Technology Journal Database) were applied to search for relevant journal articles from the inception of each database to April 2024. The search words used were a combination of medical subject headings and keywords, such as “breast cancer”, “breast tumor,” “breast neoplasm,” “return-to-work,” “back to work,” “RTW,” “job reentry,” “reemployment,” “resume work,” and “employment status.” The detailed search strategies for each database will be presented in Supporting Information 1.
2.3. Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (a) studies that analyzed a sample of patients with BC; (b) studies that measured RTW in that sample and specified the number or proportion of people who returned to work in the results; (c) language restrictions: Chinese and English; and (d) cross-sectional or cohort studies.
The exclusion criteria were (a) study samples that were mixed and lacked independent information on people with BC; (b) low-quality studies; and (c) lack of extractable effect sizes.
2.4. Study Selection
Duplicates were removed by importing documents using Endnote 20.0 software and using the software’s deduplication function, followed by a two-person (W.L. and J.W.) manual screening for duplicates. After titles and abstracts were screened by two reviewers (W.L. and J.W.) independently, a full-text evaluation based on the eligibility criteria was conducted by the same two reviewers. Any disagreement was resolved by a third review author (H.Y.).
2.5. Data Extraction
Herein, data were extracted by two reviewers based on the predefined criteria. The following variables were considered and recorded in a specific data definition record table: (a) authors; (b) year of publication; (c) country of publication; (d) study type; (e) sample size; (f) a percentage of BC patients who have returned to work in the sample. It should be noted that due to inconsistencies in RTW times between some studies and the fact that some studies did not report the time point chosen, for those studies that did report the time point, we extracted the time within 6–12 months of the patient’s RTW in order to standardize the criteria; and (g) factors influencing the RTW of BC patients, including their ORs and 95% confidence intervals. (All odd ratios mentioned in this study were extracted from the original study. We specifically selected those data that were derived using logistic regression analysis.)
2.6. Methodological Quality Assessment
Two investigators independently assessed the risk of bias in the included studies and cross-checked the results. In instances of disagreement, a third party was consulted to facilitate resolution. Cross-sectional studies were evaluated using the risk of bias criteria recommended by the Agency for Healthcare Research and Quality (AHRQ) [25]. There were 11 entries, each of which was evaluated using “Yes,” “No,” or “Unclear” as criteria, with “Yes” scoring one point and “No” or “Unclear” scoring 0. The total score for each entry was calculated by summing the individual scores, with 0–3 points as low quality, 4 to 7 points as medium quality, and 8 to 11 points as high quality [26]. The Newcastle - Ottawa Scale (NOS) [27] was used to evaluate the cohort study. The NOS is an eight-item scale ranging from 0 to 9. Scores between 0 and 3 indicate low quality, 4 to 6 suggest medium quality, and 7 to 9 signify high quality [28]. After evaluating the quality of the literature, only medium- and high-quality literature was included in the meta-analysis.
2.7. Statistical Analysis and Data Synthesis
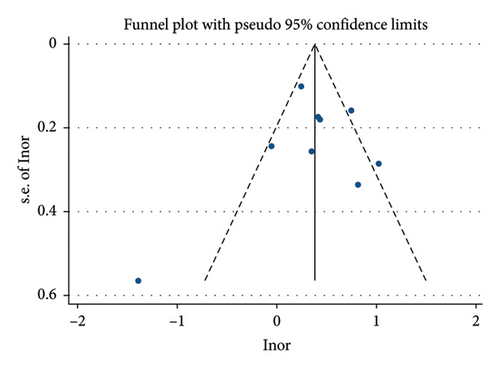
The data were analyzed using Stata 12.0 software. The ORs and 95% CIs from the literature were chosen for data merging. I2 was used to determine the extent of the heterogeneity of the data [29], and I2 ≤ 50% indicated acceptable heterogeneity among studies, using a fixed-effect model for meta-analysis. I2 > 50% suggested substantial heterogeneity, prompting the use of a random-effect model. Sensitivity analyses were performed by using a literature-by-literature exclusion method [30]. (One literature was excluded sequentially, and the remaining literature was subjected to meta-analysis. Any change in the significance of the results indicated instability). Funnel plots were drawn and used to analyze publication bias.
3. Results
3.1. Search Results
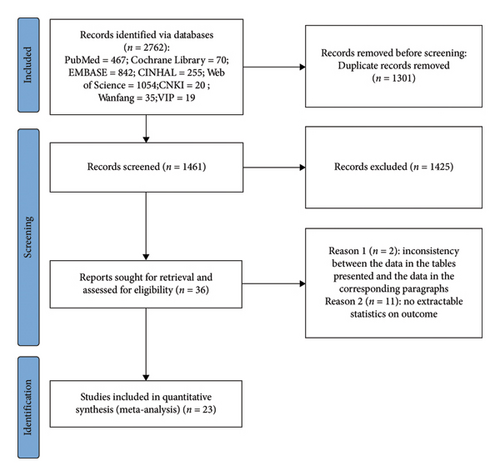
The phases of electronic searches, identification, and screening for eligible studies were depicted in the PRISMA flow diagram (Figure 1). Initially, 2762 studies were obtained through the outlined search strategy, which was conducted from the inception of each database to April 2024. After removing duplicates and screening titles and abstracts, studies were retained for full-text evaluation. Finally, a total of 23 studies were included in this systematic review and meta-analysis. These included 10 cross-sectional studies [31–40] and 13 cohort studies [41–53].
3.2. Basic Characteristics of the Included Literature
Table 1 outlines the basic characteristics of 23 studies conducted across 11 countries, spanning the years 2006–2023: USA (n = 5), Sweden (n = 3), Korea (n = 1), Germany (n = 2), Brazil (n = 1), Malaysia (n = 1), France (n = 5), China (n = 2), Norway (n = 1), the Netherlands (n = 1), and Portugal (n = 1); 10 cross-sectional studies and 13 cohort studies were included, with a sample size of 200–2000 cases and a total of 4384 participants.
| First author | Year | Country | Study type | Sample size | Return to work rate (%) | Risk factors |
|---|---|---|---|---|---|---|
| Reynard | 2006 | USA | Cross-sectional | 395 | 83.79 | ACEFM |
| Aina Johnsson | 2007 | Sweden | Cross-sectional | 222 | 84.23 | GH |
| Eunmi Ahn | 2009 | South Korea | Cross-sectional | 720 | 69.16 | CIMN |
| Aina Johnsson | 2009 | Sweden | Cohort study | 97 | 58.76 | O |
| Victoria Blinder | 2013 | USA | Cohort study | 252 | 78.96 | AFI |
| Elham Hedayati | 2013 | Sweden | Cross-sectional | 44 | 65.90 | JUW |
| Dorothee Noeres | 2013 | Germany | Cohort study | 126 | 77.77 | ADR |
| Luciana C. G. Landeiro | 2018 | Brazil | Cohort study | 111 | 39.63 | HQ |
| TT Su | 2018 | Malaysia | Cross-sectional study | 256 | 40.62 | BKV |
| Kathleen Doyle Lyons | 2019 | USA | Cross-sectional study | 163 | 20.85 | A |
| Martina E. Schmidt | 2019 | Germany | Cross-sectional study | 129 | 78.29 | JQTU |
| Antonio Di Meglio | 2020 | France | Cohort study | 1869 | 78.70 | FHIKMPQ |
| Agnes Dumas | 2020 | France | Cohort study | 1874 | 78.70 | GJIKOPQRS |
| Elsa Caumette | 2021 | France | Cross-sectional study | 3004 | 78.12 | O |
| Min Li | 2021 | China | Cohort study | 396 | 35.60 | C |
| Synne-Kristin Hoffart Bøhn | 2022 | Norway | Cross-sectional study | 845 | 62.72 | DIJNQTW |
| Rongrong Fan | 2021 | China | Cross-sectional study | 415 | 44.57 | BO |
| Fulya Balak | 2008 | Netherlands | Cross-sectional study | 72 | 94.44 | AW |
| Sophie Quinton Fantoni | 2010 | France | Cross-sectional study | 379 | 82.05 | FGV |
| Victoria S. Blinder | 2012 | USA | Cross-sectional study | 275 | 93.81 | FL |
| Isabel Monteiro | 2019 | Portugal | Cohort study | 462 | 35.06 | FGHKMPQ |
| Marc A. Emerson | 2023 | USA | Cohort study | 1649 | 20.01 | CEIR |
| Delphine Hequet | 2022 | France | Cross-sectional study | 969 | 89.68 | GIKPS |
- Note: A: age; B: educational level; C: marriage; D: cohabitation; E: race; F: chemotherapy; G: radiotherapy; H: endocrine; I: comorbidities; J: arm symptoms; K: stage; L: axillary surgery; M: breast surgery; N: adjuvant therapy; O: child; P: anxiety; Q: depression; R: working patterns; S: job type; T: cognitive function; U: physical function; V: social support; W: breast symptoms.
3.3. Results of the Quality Assessment of the Included Literature
The 23 papers included in this study were of medium and high quality. Cross-sectional studies were evaluated according to AHRQ recommendations, with 4 papers of high quality and 6 papers of medium quality, as shown in Table 2. Cohort studies were evaluated based on NOS scores, with 2 papers of high quality and 11 papers of medium quality, as shown in Table 3.
| Study | 1. Define the source of information (survey and record review) | 2. List inclusion and exclusion criteria for exposed and unexposed subjects (cases and controls) or refer to previous publications | 3. Indicate the time period used for identifying patients | 4. Indicate whether or not subjects were consecutive if not population-based | 5. Indicate if evaluators of subjective components of study were masked to other aspects of the status of the participants | 6. Describe any assessments undertaken for quality assurance purposes (e.g., test/retest of primary outcome measurements) | 7. Explain any patient exclusions from analysis | 8. Describe how confounding was assessed and/or controlled. | 9. If applicable, explain how missing data were handled in the analysis | 10. Summarize the patient response rates and completeness of data collection | 11. Clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or follow-up was obtained | Total scores |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reynard et al. 2006 | ⭐ | ⭐ | ⭐ | ⭐ | — | — | ⭐ | ⭐ | ⭐ | ⭐ | ⭐ | 9 |
| Aina Johnsson et al. 2007 | ⭐ | ⭐ | ⭐ | ⭐ | — | ⭐ | ⭐ | ⭐ | — | ⭐ | — | 8 |
| Eunmi Ahn et al. 2009 | ⭐ | — | ⭐ | ⭐ | — | — | — | ⭐ | — | ⭐ | ⭐ | 6 |
| Elham Hedayati et al. 2013 | ⭐ | ⭐ | — | ⭐ | — | ⭐ | — | ⭐ | ⭐ | ⭐ | ⭐ | 8 |
| Su et al. 2018 | ⭐ | — | — | ⭐ | — | ⭐ | — | ⭐ | ⭐ | ⭐ | — | 6 |
| Kathleen Doyle Lyons et al. 2019 | ⭐ | — | — | ⭐ | — | — | ⭐ | ⭐ | — | ⭐ | — | 5 |
| Martina E. Schmidt et al. 2018 | ⭐ | ⭐ | — | ⭐ | — | — | ⭐ | ⭐ | — | — | — | 5 |
| Synne-Kristin Hoffart Bøhn et al. 2022 | ⭐ | — | ⭐ | ⭐ | ⭐ | ⭐ | — | ⭐ | ⭐ | ⭐ | — | 8 |
| Rongrong Fan et al. 2021 | ⭐ | ⭐ | — | ⭐ | ⭐ | ⭐ | — | ⭐ | — | ⭐ | — | 7 |
| Delphine Hequet et al. 2020 | ⭐ | — | — | ⭐ | — | — | — | ⭐ | — | ⭐ | — | 4 |
| Study | NOS selection domain | NOS comparability domain | NOS outcome domain | Total scores | |||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the exposed cohort | Selection of the noncontrol cohort | Ascertainment of exposure | Demonstration that the outcome of interest was not present at the start of the study | Comparability of cohorts on the basis of the design or analysis | Assessment of the outcome | Was follow-up long enough for outcomes to occur | Adequacy of follow-up of cohorts | ||
| Johnsson et al. 2004 | ⭐ | ⭐ | — | ⭐ | ⭐ | ⭐ | ⭐ | ⭐ | 7 |
| Blinder et al. 2013 | — | — | — | ⭐ | ⭐ | — | ⭐ | ⭐ | 4 |
| Noeres et al. 2013 | ⭐ | ⭐ | — | ⭐ | — | — | ⭐ | ⭐ | 5 |
| Landeiro et al. 2018 | ⭐ | ⭐ | ⭐ | ⭐ | ⭐ | — | ⭐ | ⭐ | 7 |
| Meglio et al. 2020 | ⭐ | — | ⭐ | ⭐ | — | ⭐ | ⭐ | ⭐ | 6 |
| Dumas et al. 2019 | ⭐ | — | — | ⭐ | — | — | ⭐ | ⭐ | 4 |
| Caumette et al. 2021 | ⭐ | — | — | ⭐ | ⭐ | — | ⭐ | ⭐ | 5 |
| Li et al. | ⭐ | — | ⭐ | ⭐ | ⭐ | — | ⭐ | ⭐ | 6 |
| Balak et al. 2008 | ⭐ | — | ⭐ | ⭐ | ⭐ | ⭐ | ⭐ | — | 6 |
| Fantoni et al. 2010 | ⭐ | — | — | ⭐ | ⭐ | — | ⭐ | ⭐ | 5 |
| Blinder et al. 2012 | ⭐ | — | ⭐ | ⭐ | — | — | ⭐ | ⭐ | 5 |
| Monteiro et al. 2019 | ⭐ | — | ⭐ | ⭐ | ⭐ | — | ⭐ | ⭐ | 6 |
| Emerson et al. 2023 | ⭐ | — | ⭐ | ⭐ | — | — | ⭐ | ⭐ | 5 |
3.4. Meta-Analysis Results
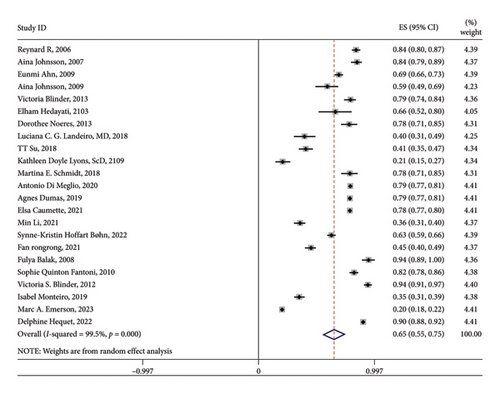
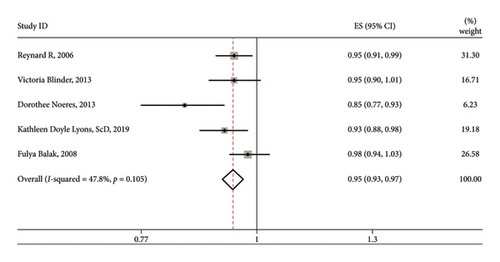
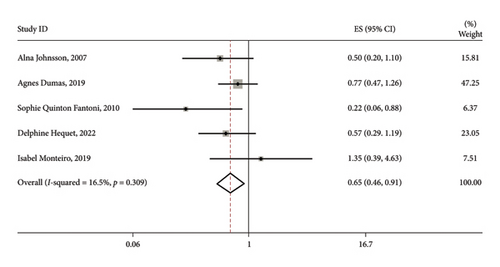
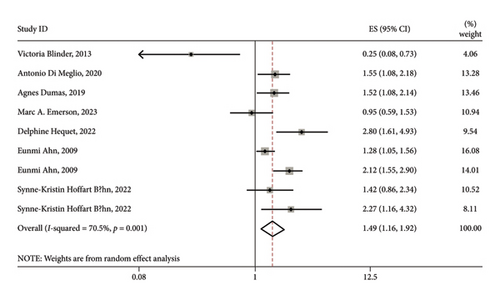
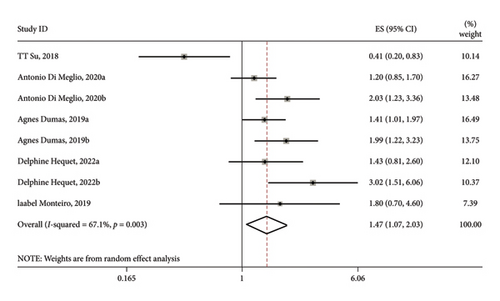
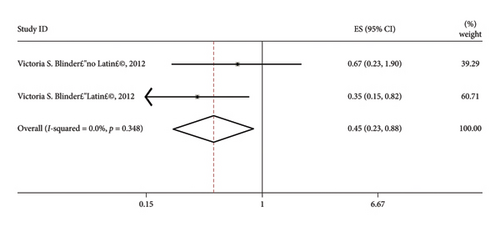
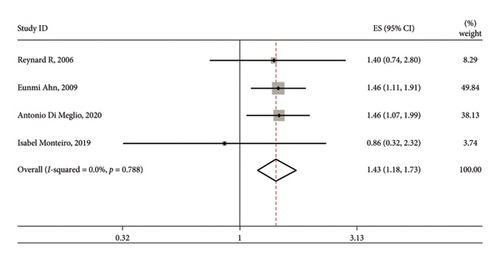
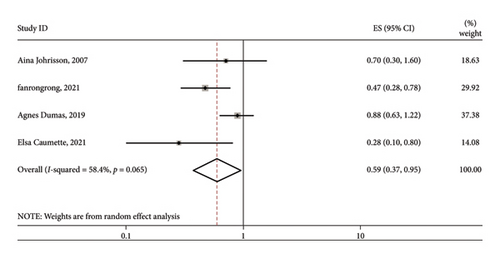
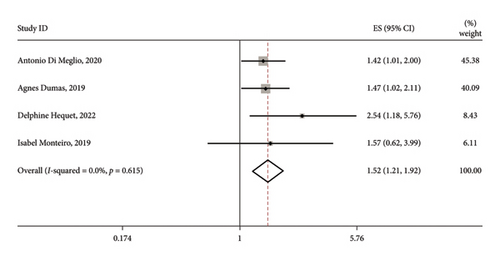
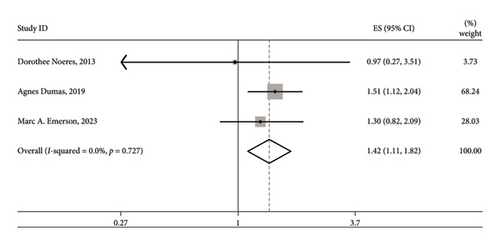
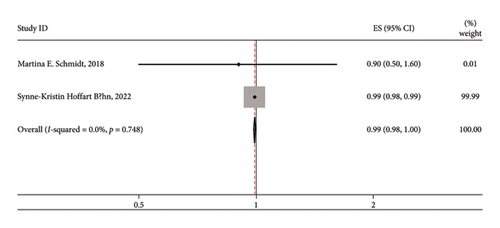
A total of 23 influencing factors were included in this meta-analysis (Table 4). The overall rate of RTW was estimated at 65.0% (95% CI: 55.0%–75.0%) (Figure 2). The results showed that the differences among the combined outcomes of various factors, such as age, chemotherapy and radiotherapy receipt, axillary clearance, surgical modality, anxiety symptoms, work pattern, cognitive function, and physical abilities, were minimal (p > 0.1, I2 ≤ 50%), so a fixed-effect model was used. The meta-analysis revealed significant heterogeneity (p < 0.1, I2 > 50%) across various factors such as education, marital status, cohabitation status, race, receipt of endocrine therapy, presence of comorbidities, experiencing arm symptoms, cancer stage, adjuvant therapy, having children, depression, type of work, social support, and breast-related symptoms. Therefore, a random-effect model was used. The meta-results showed that age, receipt of radiotherapy or not, presence of comorbidities or not, cancer stage, receipt of axillary lymph node dissection or not, surgical modality, having children or not, anxiety symptoms, work patterns, cognitive functioning, and physical functioning were the factors influencing the RTW of BC patients. The summary results of the meta-analysis are shown in Table 4 and Figures 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13.
| Influencing factors | Literature | Heterogeneity test | Meta-analysis model | OR (95% CI) | p | |
|---|---|---|---|---|---|---|
| p | I2 (%) | |||||
| Age [31, 36, 42, 43, 49] | 5 | 0.105 | 47.80 | Fixed-effect model | 0.95 (0.93, 0.97) | < 0.001 |
| Education [35, 39] | 2 | 0.093 | 64.50 | Random-effect model | 1.10 (0.45, 2.67) | 0.837 |
| Marital status [31, 33, 48, 54] | 4 | < 0.001 | 92.60 | Random-effect model | 0.949 (0.40, 2.20) | 0.881 |
| Cohabitation status [38, 43] | 2 | 0.062 | 71.40 | Random-effect model | 0.87 (0.16, 4.67) | 0.872 |
| Ethnicity [31, 54] | 2 | < 0.001 | 91.80 | Random-effect model | 0.69 (0.20, 2.39) | 0.555 |
| Chemotherapy or not [31, 42, 45, 50–52] | 6 | 0.671 | 0.00 | Fixed-effect model | 0.81 (0.63, 1.05) | 0.113 |
| Radiotherapy or not [32, 40, 46, 50, 52] | 5 | 0.309 | 16.50 | Fixed-effect model | 0.65 (0.46, 0.91) | 0.012 |
| Endocrine therapy or not [32, 44, 45, 52] | 4 | 0.048 | 62.10 | Random-effect model | 0.83 (0.38, 1.83) | 0.649 |
| Comorbidities or not [45, 46] | 2 | 0.001 | 70.50 | Random-effect model | 1.49 (1.16, 1.92) | 0.002 |
| Arm symptoms or not [34, 37, 38, 46] | 4 | 0.002 | 79.30 | Random-effect model | 1.06 (0.99, 1.130) | 0.124 |
| Cancer stage [35, 40, 45, 46, 52] | 5 | 0.003 | 67.10 | Random-effect model | 1.47 (1.07, 2.03) | 0.019 |
| Axillary lymph node dissection [51] | 1 | 0.348 | 0.00 | Fixed-effect model | 0.45 (0.23, 0.88) | 0.019 |
| Surgical modality [31, 33, 45, 52] | 4 | 0.788 | 0.00 | Fixed-effect model | 1.43 (1.18, 1.73) | < 0.001 |
| Adjuvant therapy or not [33, 38] | 2 | 0.005 | 59.30 | Random-effect model | 1.12 (0.88, 1.43) | 0.357 |
| Having children or not [39, 42, 46, 47] | 4 | 0.065 | 58.40 | Random-effect model | 0.59 (0.37, 0.95) | 0.03 |
| Anxiety symptoms [40, 45, 46, 52] | 4 | 0.615 | 0.00 | Fixed-effect model | 1.52 (1.21, 1.92) | < 0.001 |
| Depressive symptoms [37, 38, 44–46, 52] | 6 | < 0.001 | 77.80 | Random-effect model | 1.30 (0.76, 2.22) | 0.342 |
| Work pattern [43, 46, 54] | 3 | 0.727 | 0.00 | Fixed-effect model | 1.42 (1.11, 1.82) | 0.005 |
| Type of work [40, 46] | 2 | 0.024 | 80.30 | Random-effect model | 2.08 (0.51, 8.46) | 0.304 |
| Cognitive functioning [37, 38] | 2 | 0.748 | 0.00 | Fixed-effect model | 0.99 (0.98, 1.00) | < 0.001 |
| Physical functioning [34, 35] | 2 | 0.755 | 0.00 | Fixed-effect model | 0.83 (0.75, 0.92) | < 0.001 |
| Social support [35, 50] | 2 | 0.002 | 89.10 | Random-effect model | 1.16 (0.10, 14.04) | 0.904 |
| Breast-related symptoms [34, 38, 49] | 3 | 0.038 | 64.40 | Random-effect model | 1.01 (0.97, 1.04) | 0.785 |
- Note: The bold values indicate p < 0.05.

3.5. Sensitivity Analysis
In this study, sensitivity analyses were performed on factors with heterogeneity including education level A, marital status B, cohabitation status C, race D, receipt of endocrine therapy E, presence of comorbidities F, presence of arm symptoms G, cancer stage H, adjuvant therapy I, whether children were born J, depressive symptoms K, type of work L, social support M, and breast-related symptoms N. (Capital letters represent the order of the corresponding pictures; see the Figures in Supporting Information 2) Sensitivity analyses of factors including receipt of endocrine therapy, presence of comorbidities, cancer stage, and presence of adjuvant therapy showed little difference between the results after the exclusion of each article and the original results, indicating the stability of the results. Sensitivity analyses involving the factor “whether having children” significantly impacted the RTW outcomes of BC patients, showing a large difference in the variation of results upon removing Agnes Dumas’s study [46]. This may be related to the large sample size of this study (n = 1874).
3.6. Publication Bias
In this study, we conducted a publication bias analysis focusing on comorbidities, and the results showed asymmetry in the funnel plots, suggesting potential publication bias (Figure 14).
4. Discussion
Our study reviewed 23 studies assessing the RTW outcomes of previously employed BC survivors. The results of the meta-analysis showed that the factors affecting the RTW of BC survivors could be classified into the following categories: socio-demographic, disease status, treatment-related, psychological/emotional status, and job-related factors.
4.1. Socio-Demographic Factors
The present study showed that among the socio-demographic factors, the age of BC survivors and whether they have children or not are important factors associated with RTW. Younger age and having children increase the likelihood of RTW than older BC patients, consistent with previous studies [23, 37]. This tendency can be attributed to their superior physical capabilities, increased energy levels, existing employment history, and accumulated knowledge prior to their cancer diagnosis [55]. In contrast, older patients are more likely to have complications due to the gradual deterioration of their physical functioning, impacting their social engagement and work capacity. This can be attributed to their retired status or lack of inclination to work [56], alongside greater economic stability at this stage of life [57]. Therefore, it is necessary to focus on patients of working age, analyze their difficulties and obstacles to returning to work, and develop individualized interventions to help them RTW. Having children often motivates patients to RTW, possibly due to a sense of familial duty and the desire to contribute to the family’s financial well-being [58]. This aligns with the study by Porro et al. [59] but contrary to the findings of Caumette et al. [60], Johnsson et al. [32], and Lee et al. [61]. The differences could be due to variations in cultural contexts, sample characteristics, and methodologies used across studies. Additionally, economic stability and healthcare systems in different countries could also account for these discrepancies. This combined result stands out as the only diverse finding among the significant factors in this study. For future analyses, it is crucial to broaden the scope by incorporating studies from various countries and cultural backgrounds. Factors such as the number and age of children, as well as economic situations, should be considered. Lee’s findings, for example, showed that many patients would give up returning to work because of the need to care for their children at a young age [61]. In the future, consideration can be given to supporting patients who have recently given birth by offering flexible work options such as telecommuting and adjustable work hours. This will help them effectively manage both their family responsibilities and work commitments. The support of their spouses is also an aspect that needs to be taken into account.
4.2. Factors Related to Disease Status
In this study, the stage of cancer and comorbidities emerged as significant disease-related factors influencing RTW among BC survivors. Patients diagnosed with early-stage BC are more likely to RTW than those with advanced BC. Cancer treatment duration and intensity vary based on the stage. Early-stage cancers often require shorter treatments, primarily surgical, aimed at tumor removal. In contrast, advanced stages necessitate longer, comprehensive approaches due to the need for combined therapies such as chemotherapy and radiotherapy, which bring about more adverse effects, demanding extended recovery periods [62, 63]. The side effects of these treatments can affect recovery, potentially impacting a patient’s ability to work during this time [64]. Patients with more advanced cancers often face greater physical burdens and recovery challenges. Treatment may take a greater toll on the body, leading to a prolonged and more challenging recovery process [65]. Also, people with more advanced cancer may face greater psychological burdens and emotional distress [66]. This may include uncertainty about the future and concern about the effectiveness of treatment. Psychological factors can lead patients to approach their RTW cautiously, often requiring additional time to address emotional challenges. The results found that the presence of comorbidities can prevent BC patients from returning to work. BC-related comorbidities such as fatigue, pain, and lymphedema are important factors affecting patients’ RTW [22]. The present studies showed that patients with one or more comorbidities are more difficult to RTW than those without comorbidities [67, 68]. The presence of comorbidities may lead to instability or deterioration of the patient’s physical condition, which may affect the patient’s ability to work. Patients may need more time to recover and adjust to life, thus delaying or adjusting plans to RTW [69, 70]. Besides, comorbidities may increase the psychological burden on patients, including emotional problems such as anxiety and depression [71, 72]. These mental health issues may affect the patient’s interest and confidence in work and reduce their motivation to RTW [73, 74]. When evaluating a BC patient’s RTW, a thorough assessment of how comorbidities affect their physical and mental health, along with the challenges they present in adapting to work, helps to better grasp the role of these additional health conditions in the decision-making process. The impact of these factors may vary with individual patients, and each patient’s decision is influenced by a combination of factors.
4.3. Factors Related to Treatment
This study revealed significant correlations between a patient’s RTW and specific treatment factors, such as receiving radiotherapy, undergoing axillary lymph node dissection, and the type of surgery (breast-conserving or mastectomy). Patients who have radiotherapy treatment or axillary lymph node dissection or mastectomy are more likely to RTW, a result that is consistent with previous studies [23, 56, 75]. The reason for this is that these treatments help to control the progression of BC and improve the health of the patient [76]. When treatment succeeds and patients experience improved health, their likelihood of returning to work increases [77]. It also needs to be taken into account that after successfully undergoing these treatments, patients may experience increased confidence and a more positive mindset [78]. This positive mindset may contribute to their earlier return to normal life, including the RTW [79]. It is important to note that BC treatment encompasses a range of approaches, and individual variations along with specific circumstances can significantly influence treatment and recovery outcomes. It is crucial to highlight that our study results only represent a trend. Indeed, each patient’s recovery and RTW may vary depending on a variety of factors. For example, some studies [80, 81] reported that undergoing lymph node dissection surgery results in an increased likelihood of upper limb disability affecting the patient’s RTW. More studies should be included in future analyses.
4.4. Factors Related to Physical and Mental Status
In this study, anxiety levels, cognitive function, and physical well-being emerged as crucial factors influencing the RTW among BC survivors, highlighting their significance in both physical and mental aspects. A diagnosis of anxiety symptoms can make it harder for a patient to RTW. Anxiety adds to the psychological load, making it tough to handle the stresses and challenges of the job [82, 83]. This may lead to resistance to work and affect their willingness and ability to RTW. Attention also needs to be paid to the provision of psychological support services to help patients to overcome anxiety and improve their self-confidence, so that they can RTW with greater confidence. The results of this study show a positive correlation between cognitive function and RTW. Previous studies [84, 85] have shown that approximately 34% of BC patients who undergo cancer treatment experience cognitive dysfunction. This is strongly associated with reduced ability to work, including memory issues impacting timely task completion, significantly influencing their ability to RTW [34]. Improved cognitive function leads to enhanced learning and memory capabilities. In the work environment, it is necessary to constantly learn new information and adapt to new work requirements, and enhanced cognitive function facilitates a smoother adjustment to new job demands, expediting the RTW [86]. In the rehabilitation treatment of BC patients, attention should be paid to the provision of enhanced cognitive function training, including professional cognitive rehabilitation programs, to help patients improve their cognitive abilities in learning, memory, decision-making, and other aspects. Currently, there are relevant exercise studies [87, 88] showing that it can promote cognitive recovery to a certain extent, mainly through internet-based cognitive forging games, including speed training, memory training, reasoning training, imagery training, and storytelling. The better the physical functioning, the greater the likelihood of RTW in this study. Improving physical functioning enhances a patient’s capacity to perform tasks at work and adapt to the work environment more effectively [89]. Enhanced physical functioning may increase productivity and reduce the physical burden of being at work, thus facilitating the likelihood of RTW [90]. Good physical functioning may also be seen by employers as a sign of the patient’s recovery, indicating that the patient can perform the job [91]. This may increase the employer’s confidence in the patient’s ability and make it easier for him/her to integrate into the work team [92].
4.5. Factors Related to Job Characteristics
This study revealed that the employment status of BC survivors, whether they worked part-time or full-time prior to their illness, is a significant factor influencing their RTW outcomes. Besides, patients who work part-time before diagnosis have more difficulty returning to work. Firstly, different work patterns often correspond to different occupational requirements and skills, and patients may have chosen to work part-time based on their current life situation and ability level [93]. Cancer patients may need more time to adapt to the skills and occupational requirements needed for their original job [92]. Secondly, patients opting for part-time work may rely more on social support networks, be it from employers, coworkers, or other interested parties, potentially impacting the stability of their recovery process [94]. Establishing a social support network in part-time versus full-time work settings differs, requiring time for patients to build new support systems. It is important to note that this study demonstrates only general trends, yet the specifics may be affected by several factors such as individual patient differences, the degree of rehabilitation, and the specific work environment.
4.6. Other Factors
Although the results of this meta-analysis showed that the p values in the combined results of possible influences such as education, marital status, and type of work were greater than 0.05, this does not mean that these factors are meaningless in the process of returning to work for BC patients. Firstly, the p value is not the only criterion for assessing the strength of the variable’s impact on the outcome [95]. Factors that do not reach statistical significance can still influence patients’ RTW, especially considering individual differences and cultural backgrounds. For example, one study [54] showed that patients with higher levels of education chose to RTW, and another study [96] showed that those in high-paying occupations, such as professional technicians, tended to RTW more quickly. Secondly, factors such as the education level, marital status, and type of work may play different roles in different contexts and groups. For example, in Emerson’s study [97], blacks and whites, irrespective of their life statuses, demonstrated varied RTW results. There is also a need to take into account factors such as the heterogeneity of the study sample and the potential lack of control variables, the effects of which may not have been fully included in the analyses, leading to statistically insignificant results. Future studies can further explore the potential impact of these factors on the RTW of BC patients through a more refined design and more comprehensive data collection. This will help to provide a more comprehensive understanding of the multidimensional factors involved in the work reintegration of BC patients and provide a more nuanced reference for the development of individualized rehabilitation plans.
5. Limitations
The present meta-analysis faced several limitations, and the results need to be interpreted with caution:
Firstly, the limited number of studies included in the analysis restricted the ability to perform in-depth exploration and subgroup analyses of certain factors. Consequently, the robustness and generalizability of the results were constrained by the number of studies. Subgroup analyses were not used in this study to explore changes in RTW rates and their correlates over time due to the inconsistency of some studies regarding the timing of measurements and the lack of reported data on different time points for categorization. Future studies should consider these factors to more accurately understand the dynamics of the RTW process.
Secondly, the insufficient number of studies did not allow for a comprehensive analysis of bias, including funnel plot analysis. This meant that we were unable to fully assess the risk of possible publication bias and selective reporting of results. BC patients may face different cultural contexts, healthcare systems, and social support structures in different countries and regions, and these differences may influence the decision-making factors related to RTW. Therefore, the generalization of study findings may be limited in cross-cultural contexts. Specifically, studies from low-income and middle-income countries, as well as certain regions in Asia, were excluded due to methodological issues and data limitations. This exclusion may affect the generalizability of the findings to these regions.
Additionally, language bias is another limitation that could influence the results of this meta-analysis. While this study included studies from both English and Chinese databases, there remains a potential bias toward the inclusion of studies published in these two languages. Studies published in other languages, particularly those from regions with limited English or Chinese publication, were not included due to language barriers and database limitations. This may lead to an overrepresentation of studies from English- and Chinese-speaking countries, which could limit the global applicability of the findings. Future research should aim to include studies published in a wider range of languages to mitigate this potential bias.
Moreover, the absence of psychological databases such as PsycINFO, which contains studies focused on the psychological aspects of RTW, is another limitation. Including such databases would improve the comprehensiveness of the sample by incorporating studies on psychological factors, which are crucial in determining RTW outcomes. The exclusion of these resources may limit the scope of this meta-analysis, and future research should aim to integrate psychological and social factors by consulting such databases for a more complete understanding of RTW in BC patients.
Finally, the interpretation of the results requires more caution due to the heterogeneity of the included studies, including differences in samples and study designs. Heterogeneity that is not fully explained may have implications for the interpretation of results. Although every effort was made to include available control variables, certain potential confounders that were not accounted for may still exist and may have some impact on the internal validity of the results.
In summary, although this study provides initial insights into the factors that contribute to the RTW of BC patients, caution needs to be taken when interpreting the results. These limitations should be seen as an opportunity for future research to address gaps and further enhance the understanding of this field in a more comprehensive and reliable manner.
6. Conclusion
The results of this meta-analysis provide insights into the factors influencing the RTW of BC survivors. RTW depends on a combination and interaction of socio-demographic factors, factors related to disease status, factors related to treatment, factors related to physical and mental status, and factors related to job characteristics. The complexity and potential for interactions among the various variables add to the challenges for healthcare providers in promoting vocational rehabilitation services for BC patients, emphasizing the need to adequately consider patients’ vocational rehabilitation needs in BC treatment planning. While certain factors such as education level, marital status, and type of job showed p values greater than 0.05, it is important to note that this does not mean that they are not meaningless. Future studies should increase the sample size and incorporate a more diverse range of cultural factors to enhance the external validity of the study. In-depth research in this area will contribute to the development of more personalized and comprehensive rehabilitation programs for BC patients, as well as provide more tailored support for their vocational reintegration.
Ethics Statement
This study is a systematic review and meta-analysis that focuses on aggregating and analyzing the results of previously published studies. The meta-analysis was exempted from ethical review as it directly used data from the published literature rather than directly involving study participants or subjects, and strict adherence to academic ethics and data use policies was ensured in our study.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
All authors contributed to the study conception and design. The contribution of every author is as follows:
Wen Li: conceptualization; data curation; formal analysis; investigation; methodology; software; validation; visualization; writing – original draft; and writing – review and editing.
Jingcheng Wen: conceptualization; data curation; formal analysis; investigation; methodology; software; validation; visualization; writing – original draft; and writing – review and editing.
Dong Pang: conceptualization; project administration; supervision; writing – original draft; and writing – review and editing.
Yuhan Lu: conceptualization; project administration; supervision; and writing – review and editing.
Hongli Li: data curation; software; validation; writing – original draft; and writing – review and editing.
Hong Yang: conceptualization; project administration; supervision; and writing – review and editing.
All authors read and approved the final manuscript. Wen Li and Jingcheng Wen are co-first authors and have contributed equally to the article.
Funding
This work was supported by the Science Foundation of Peking University Cancer Hospital PY202336.
Supporting Information
Additional supporting information can be found online in the Supporting Information section.
Open Research
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.




