Randomized Clinical Study of Laser vs. Cryotherapy in Plantar Warts: Effectiveness and Safety
Abstract
Introduction: Plantar warts are common skin lesions caused by HPV that can generate discomfort and impact quality of life. There are several therapeutic options such as cryotherapy or laser, but more high-quality comparative studies are needed.
Methods: A randomized clinical trial was performed with 44 patients with plantar warts who were assigned 22 to each group. Sessions were applied at 1-week intervals evaluating clinical healing, VAS pain scale, and complications.
Results: Laser removed warts in significantly fewer sessions (mean 3.26) than cryotherapy (mean 4.06) (p = 0.022). There were no differences in safety or pain between groups.
Conclusion: Diode laser demonstrated faster removal of plantar warts than cryotherapy, constituting a promising noninvasive alternative. Further studies are needed to confirm its long-term efficacy and safety profile.
Trial Registration: ClinicalTrials.gov identifier: NCT06228521
1. Introduction
Plantar warts are benign skin lesions caused by human papillomavirus (HPV), which commonly affect pressure areas on the sole of the foot [1]. HPV Types 2, 4, 27, 57, and 60 are the most frequent strains responsible for cutaneous plantar warts [1, 2]. Its prevalence is estimated to be 7%–12% [3] and is more frequent in children and young adults [1], especially between 12 and 16 years of age [3, 4]. It decreases in older adults because of greater immunological resistance. Geographic and socioeconomic factors, such as warm and humid climates and the habit of walking barefoot, can increase the incidence of plantar warts [5]. Plantar warts are highly contagious and easily transmitted in damp places such as locker rooms or swimming pools [1, 6]. Although most resolve spontaneously, they often recur and, in some cases, progress and spread, requiring treatment [7].
Clinically, they manifest as hyperkeratotic lesions of varying color [8], well demarcated, with an irregular surface due to the elongation of epidermal ridges [9]. They are usually asymptomatic, but may cause pain or difficulty in ambulation. They are located in areas of plantar pressure, such as the heels, metatarsal heads, or toes. Diagnosis is usually based on clinical, lateral application, and compression [10], but techniques such as dermoscopy improve diagnostic certainty [11]. Therapeutic options include physical methods (cryotherapy and Light Amplification by Stimulated Emission of Radiation [LASER]) [12–14], chemical agents (salicylic acid, monochloroacetic acid, and trichloroacetic acid) [2, 15, 16], and immunomodulators or antineoplastic agents [6, 17] to eliminate the lesions and associated pain.
Cryotherapy with liquid nitrogen is widely recognized as a first-line treatment for plantar warts, although reported cure rates vary considerably (26%–93%) [12, 18–20]. This variability can be attributed to differences in treatment protocols, such as the duration [21] and frequency of freeze cycles or the method of application, as well as patient-specific factors, including lesion depth, skin thickness, and number and size of warts [12]. These factors influence the efficacy observed in both clinical practice and published studies, thereby explaining the broad range of cure rates reported in the literature. In fact, freeze–thaw cycles are performed with variable duration and intervals depending on the protocol [13, 22].
There are other newer treatments, such as lasers, that appear to be promising alternatives because of their high effectiveness [8, 23, 24]; however, more high-quality comparative studies are needed. The diode laser is a semiconductor laser that produces selective photocoagulation and vaporization of tissues using energy to generate selective heat in specific chromophores of the skin, such as hemoglobin and melanin, causing controlled photothermolysis without damaging surrounding tissues [25–27]. Cryotherapy, which employs extreme cold to freeze and destroy tissues more generally, induces necrosis and a more extensive inflammatory response. Therefore, laser therapy has been proposed as an alternative treatment for plantar warts with promising results [20, 28]. This randomized clinical trial aimed to compare the efficacy and safety of cryotherapy versus diode laser for the treatment of plantar warts through a rigorous evaluation in terms of clinical cure, referred pain, and presence of complications. In this study, we aimed to investigate whether diode laser application demonstrated greater efficacy than cryotherapy in removing simple plantar warts.
2. Methods
2.1. Study Design
A simple-blind 5-week randomized controlled trial (RCT) was performed in accordance with the CONSORT guidelines [29]. Two parallel experimental groups of 22 patients each were included to compare the effects of the two treatments. The first experimental group performed CryoIQ at −89°C, and the second group received LASEmaR MINI 980. This study was approved by the Research Ethics Committee of the University Catholic University of Valencia (UCV/2022-2023/080) in accordance with the ethical guidelines of the Helsinki declaration [30]. Data collection was performed between February 1, 2024, and March 31, 2024, in a single-blind design at the Studio di Podologia Secolo Clinic (Italy). All the participants were recruited from the same clinic and provided written informed consent [29, 31].
2.2. Participants
Forty-four patients (22 men and 22 women) with a mean age of 37.89 ± 15.04 years, who met the inclusion criteria of being (i) between 18 and 60 years old and (ii) presenting with simple plantar warts, were recruited. Patients with (i) diabetes, (ii) ischemic diseases, (iii) immunosuppression, or (iv) Raynaud’s syndrome were excluded. Participants were randomly assigned to two treatment groups: LASEmaR group (n = 22) and CryoIQ group (n = 22). There were no statistically significant differences in baseline demographic and clinical variables between the two groups (Table 1). All participants completed the study and analyses, according to their group assignments.
| Variable | All participants (n = 44) | LASEmaR (n = 22) | CryoIQ (n = 22) | p value |
|---|---|---|---|---|
| Age (mean ± SD) | 37.89 ± 15.04 | 39.00 ± 16.72 | 36.77 ± 13.45 | 0.63 |
| (18.0, 28.75) | 14 (31.82%) | 8 (57.14%) | 6 (42.86%) | 0.74 |
| (28.75, 39.5) | 7 (15.91%) | 1 (14.29%) | 6 (85.71%) | 0.09 |
| (39.5, 50.25) | 11 (25%) | 6 (54.55%) | 5 (45.45%) | 1.0 |
| (50.25, 61.0) | 12 (27.27%) | 7 (58.33%) | 5 (41.67%) | 0.73 |
| Height (m) | 167.66 ± 9.09 | 167.23 ± 7.82 | 168.09 ± 10.38 | 0.76 |
| Weight (kg) | 68.68 ± 9.60 | 69.91 ± 8.84 | 67.45 ± 10.37 | 0.40 |
| Body mass index (kg/m2) | 24.43 ± 2.95 | 25.05 ± 3.17 | 23.81 ± 2.65 | 0.17 |
| Sex, n (%) | ||||
| Men | 22 (50%) | 10 (45.45%) | 10 (45.45%) | 1.00 |
| Women | 22 (50%) | 12 (54.55%) | 12 (54.55%) | |
| Location, n (%) | ||||
| Forefoot | 26 (59.09%) | 13 (59.09%) | 13 (59.09%) | 0.82 |
| Midfoot | 3 (6.82%) | 1 (4.55%) | 2 (9.09%) | |
| Rearfoot | 14 (34.09%) | 8 (36.36%) | 7 (31.82%) | |
| Smoking | 4 (9.09%) | 3 (13.64%) | 1 (4.55%) | 0.29 |
| Family background | ||||
| Yes | 17 (38.64%) | 10 (45.45%) | 7 (38.64%) | 0.35 |
| No | 27 (61.36%) | 12 (54.55%) | 15 (68.18%) | |
| Personal antecedents | ||||
| Yes | 15 (34.09%) | 7 (31.82%) | 8 (36.36%) | 0.75 |
| No | 29 (65.91%) | 15 (68.18%) | 14 (63.64%) |
- Note: The chi-square test.
2.3. Sample Size and Randomization
The sample size was estimated using de GPower software (Franz Faul, Universität Kiel, Kiel, Germany), Version 3.1.9.2. There have been no similar studies allowing for the calculation of sample sizes based on reference means and standard deviations (SD). For this, we employed the means of two normal populations, assuming that the SD of both populations are equal to each other, with a value of one unit. We work with a significance of 5%, and we want to have a power of 80% to detect a difference of 0.85 units. We want both the samples to have the same number of observations. We do not expect to observe losses in the samples. We required a minimum of 22 observations for each sample. In total, 44 observations were required. The expected half-width of the confidence interval is 0.60847 units.
To ensure internal validity and avoid bias, the participants were randomly assigned to one of the two treatment groups: laser or cryotherapy. A computerized system using a pseudorandom number algorithm generated the randomization sequence, minimizing selection bias, and balancing baseline characteristics between groups to equally distribute potential confounders. An independent investigator, uninvolved in recruitment or evaluation, generated the sequence using Microsoft Excel (Redmond, Washington, USA) and securely stored it in a protected file, periodically reviewing it to ensure strict adherence. Participants were assigned sequentially based on a preestablished randomization order without deviations. To maintain objectivity, treatment procedures were performed by trained investigators following standardized protocols for both methods, with no involvement in recruitment or follow-up evaluations. The study employed a single-blind design in which participants were informed that they would receive one of the two approved treatments for plantar warts but were not told the specific method. Independent evaluators blinded to group assignments conducted posttreatment assessments, avoided treatment sessions, and refrained from discussing treatment specifics with participants to ensure unbiased outcome evaluations. All randomization details, including assignments and sequence integrity, were documented and stored securely for potential audits, ensuring transparency.
2.4. Intervention
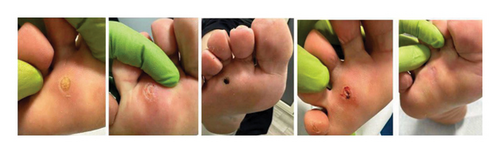
Prior to treatment, superficial debridement of the wart was performed to eliminate the most external and keratinized layers of the lesion. A Number 3 scalpel handle was used with Number 10 scalpel blades. This preparatory procedure allows for greater penetration of the treatment into the target tissue, thus optimizing its effect on the structures present in the wart. The CryoIQ group received cryotherapy by the application of liquid nitrogen using a CryoIQ 25 g/N2O cryopistol device. This technique, also known as cryosurgery, is based on the principle of cellular cryodestruction, caused by extreme tissue cooling. The procedure consisted of a controlled freeze–thaw cycle of the wart lesion, with a standardized duration of 5 s for each phase. During the freezing stage, liquid nitrogen, which is in a cryogenic state at a temperature of −196°C/–320°F, was applied directly to the wart using cryopistol. This device has a delivery system that allows controlled release of a cryogenic agent in the form of a jet or fine spray. The freezing temperature reached by the CryoIQ device is −89°C/–128°F, which is a thermal range sufficient to induce the formation of intracellular ice crystals and thus cause the destruction of the HPV-infected epidermal cells that make up the wart (Figure 1).

The LASEmaR group was treated with a 980-nm wavelength diode laser (LASEmaR MINI 980: 980 nm), a solid-state laser technology widely used in biomedical applications owing to its high efficacy and safety. The irradiation parameters were carefully configured and standardized: an output power of 2.0 W, an exposure time of 5 s, and a laser beam diameter of 1.0 mm were used (Figure 2).
However, both treatments present challenges that can affect their effectiveness. Laser therapy requires technical expertise to avoid variability in results, and its cost may limit accessibility as well as patient sensitivity [28, 32]. Cryotherapy, on the other hand, may present variability in its application and side effects such as pain or depigmentation, in addition to requiring multiple sessions in some cases [12, 13]. To minimize these challenges, a standardized protocol was implemented to ensure controlled and consistent application of both treatments.
2.5. Outcomes Measures
2.5.1. Measurement of Anthropometric Variables
During the first day of the procedure, the patient was interviewed to gather her anthropometric data, and both weight and height were measured using a scale with an incorporated stadiometer. The history of warts in the family members, as well as the possible complications and the follow-up of each of the weekly visits until cure were incorporated into this notebook.
2.5.2. Pain Perception as a Primary Outcome
The use of the Visual Analog Scale (VAS) for pain perception is common in both clinical practice and research to measure pain intensity. This tool consists of a straight line, typically 10 cm (100 mm) in length, although this can vary. The line starts with “No Pain” at the far left (scored as 0) and ends with “Maximum Pain” on the far right (scored as 10). Patients are instructed to indicate the spot on the line that best reflects their current pain level. Measurements were taken weekly throughout the treatment period, coinciding with each patient’s visit. This included an initial assessment before the first session, measurements taken during each session to detect immediate changes in pain perception, and a final assessment at the completion of treatment. The VAS is appreciated for its simplicity and adaptability, allowing it to be easily implemented in a variety of contexts, such as patient assessments in hospitals or pain management study level [33].
2.5.3. Monitoring Days as a Secondary Outcome
Comprehensive monitoring and evaluation of the clinical progress in wart resolution were performed weekly. Progress in lesion healing was assessed by visual inspection and palpation, recording the stage of remission and the integrity of the surrounding skin. Resolution of the plantar wart was defined as the total absence of clinical signs of the lesion and complete restoration of the normal skin upon close inspection. During weekly follow-up visits, the evolution of the lesion was evaluated, and a decision was made between three options: administering another treatment application, postponing treatment until the next weekly visit, or determining that the wart had completely healed. This approach ensures individualized treatment tailored to each patient [18]. The investigators consulted each other to make a collective decision, ensuring consistency and accuracy of the treatment assessment.
2.5.4. Clinical Reviews as an Exploratory Analysis
To ensure impartiality and minimize any bias, an independent clinical evaluator who was unaware of the assigned treatment was designated to perform periodic follow-up evaluations. In the event that the evaluator determined that the patient was not yet cured, the patient was referred to another evaluator who was aware of the corresponding treatment assignment and then proceeded to administer the treatment again. All possible complications were documented in a centralized database, ensuring a detailed and continuous record as part of the safety monitoring process.
2.6. Statistical Analysis
The data are presented as means and SD after corroborating the normal distribution using the Kolmogorov–Smirnov test (p > 0.05). To assess the effects of the intervention, repeated-measures analysis of variance (ANOVA) was performed. When a statistically significant main effect was detected, post hoc comparisons were performed using Student’s t-test adjusted by Bonferroni correction to identify specific differences between groups. The magnitude of effect sizes was interpreted according to the categories proposed by Hopkins, classifying them as trivial (< 0.20), small (0.20–0.59), moderate (0.60–1.19), large (1.20–1.99), or very large (≥ 2.00) [34]. All computations were performed using JASP (the Netherlands), user-friendly visual software designed to conduct intricate statistical analyses.
3. Results
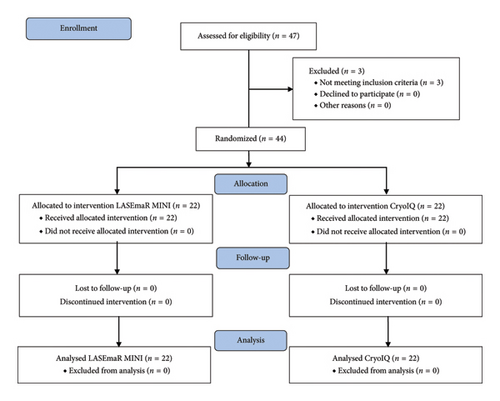
Participants were randomly assigned to two treatment groups: 22 received a diode laser (LASEmaR) (50%) and 22 received liquid nitrogen cryotherapy (CryoIQ) (Figure 3). No statistically significant differences were found in demographic variables (Table 1). All participants completed the study protocol and were included in the statistical analysis according to their randomization group (intention-to-treat analysis). There were no losses to follow-up or dropouts in either group during the study.
3.1. Pain Assessment According to the VAS
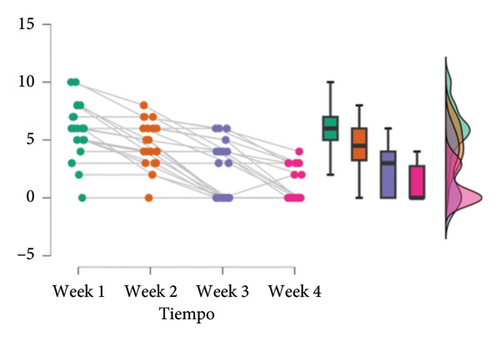
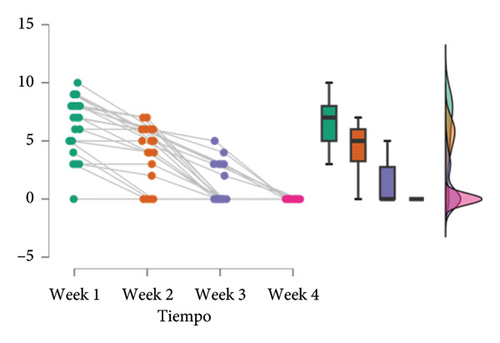
The results obtained in this study are summarized below. At Week 1, the laser treatment group had a mean of 6.27 (SD = 2.53), while the cryotherapy group had a mean of 5.86 (SD = 2.34). During Week 2, a decrease in the means for both groups was observed, being 4.27 (SD = 2.39) for the laser group and 4.59 (SD = 1.97) for the cryotherapy group. At Week 3, the means continued to decrease, with values of 1.05 (SD = 1.65) and 2.45 (SD = 2.42) for the laser and cryotherapy groups, respectively. Finally, at Week 4, the laser group was all cured, while the cryotherapy group presented a mean of 1.05 (SD = 1.46) with one subject, suggesting the persistence of some variability in this group (Figure 4).
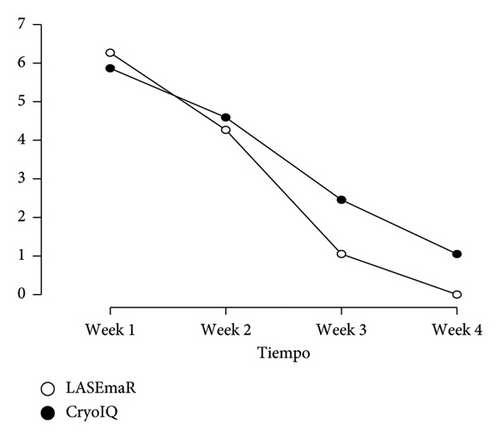
Importantly, although both groups exhibited a decreasing trend in means over the weeks, the reported SD provided valuable information on the variability of the data in each group and week. These findings provide an overview of the evolution of treatments over time and lay the groundwork for future research and further analysis.
There was a significant effect of the time factor (F(3, 126) = 129.93, p < 0.001, η2 = 0.54), as shown in Table 2. This result indicates that the means of the scores differed significantly between different measurement times, with a large effect size (η2 = 0.54). The second row shows no significant interaction between time and treatment (F(3, 126) = 3.33, p = 0.02, η2 = 0.01). This suggests that the effect of time did not differ significantly between the two treatment groups. There was a significant main effect of the time factor, suggesting that scores changed significantly across the different measurement times, but there was no significant interaction between time and treatment, implying that the effect of time did not differ between the treatment groups.
| Case | Sum of de squares | gl | Medium square | F | p | η2 |
|---|---|---|---|---|---|---|
| Time | 836.61a | 3a | 278.87a | 129.93a | < 0.001a | 0.54 |
| Time ∗ treatment | 21.45a | 3a | 7.15a | 3.33a | 0.02a | 0.01 |
| Residuals | 270.43 | 126 | 2.15 |
- Note: Sum of squares Type III.
- aMauchly’s sphericity contrast indicates that the assumption of sphericity is not met (p < 0.05).
The GEE model, adjusted for covariates such as age and sex, showed that the initial mean pain score (Week 1) was 7.74 points (p < 0.001) in the reference group treated with LASEmaR (treatment 0, male sex, average age). No significant differences were observed in the initial pain scores between treatments (coefficient = -1.14, p = 0.228) or gender (coefficient = -0.1666, p = 0.746). However, age showed a marginally significant trend (coefficient = 0.0329, p = 0.060), suggesting that older patients might report slightly higher pain, although the effect size was small. Pain significantly decreased over time for both treatments (coefficient = -2.44, p < 0.001), with a significant interaction between treatment and time (coefficient = 0.7335, p = 0.017), indicating that the group treated with CryoIQ experienced a faster reduction in pain compared to LASEmaR (Figure 5). The effect size for pain reduction over time was large, with an average decrease of 2.44 points per week, while the treatment–time interaction showed a moderate effect size (coefficient = 0.7335), highlighting a clinical difference in the rate of pain relief (Figure 6). Adjustment for covariates confirmed that factors such as age had a minimal impact on pain scores, and sex did not show a significant influence. These findings reinforce the efficacy of both treatments in reducing pain over time, although CryoIQ may be preferred for patients seeking faster initial pain relief. This analysis emphasized the importance of tailoring therapeutic options based on patient characteristics and expected pain trajectories.
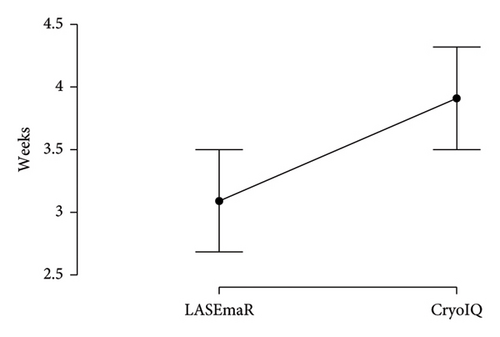
The mean number of treatment sessions required until complete plantar wart removal was significantly lower in the LASEmaR diode laser group (3.09 ± 0.92 sessions) compared to the CryoIQ cryotherapy group (3.91 ± 0.92 sessions), as revealed by the Mann–Whitney U test (p = 0.02). The effect size for this comparison was medium, with a biserial rank correlation value of −0.40 (95% CI: −0.65 to −0.08).
3.2. Adverse Effects
Only one complication was recorded in one patient who experienced considerable pain, despite normal dermal signs.
4. Discussion
The results showed that laser allowed the warts to be removed in fewer sessions compared to cryotherapy (3.09 ± 0.92) and cryotherapy (3.91 ± 0.92). However, both therapeutic modalities were similar in terms of the safety and pain associated with the procedure. Cryotherapy is considered a first-line option for the treatment of cutaneous warts [7, 13, 15, 19–21]. In our study, liquid nitrogen cryotherapy achieved complete removal of all plantar warts (mean, 3.91 sessions). This cure rate is in agreement with previous systematic reviews reporting overall cure rates of 45%–77% [6, 12, 14, 18–20]. On the other hand, laser therapy has emerged as a promising alternative for different dermatologic lesions, including viral warts [24]. Several previous studies have shown positive results with diode lasers for plantar warts [35], but these were case series without a control group [12, 18–20]. Our clinical trial provides strong quantitative evidence, showing that the diode laser (980 nm) allows the removal of plantar warts in significantly fewer sessions than cryotherapy. One possible explanation for the faster speed of the laser is its selective mechanism of action [25].
Unlike cryotherapy, which causes nonspecific destruction of all layers of the skin, laser therapy targets the blood vessels irrigating the wart by being absorbed by oxyhemoglobin, thereby preserving adjacent healthy tissue [25, 36]. These findings align with those of previous studies that have highlighted the efficacy of diode lasers in reducing the number of treatment sessions required for plantar wart removal [18, 28, 32]. However, while earlier research has suggested that diode lasers may be less painful due to their selective action and the absence of freezing [20, 28], our results did not find statistically significant differences in pain scores between the two groups. This discrepancy may be attributable to differences in pain assessment methods, patient characteristics, and treatment protocols across the studies. These observations underscore the importance of future research to clarify such discrepancies and to validate these results in larger and more diverse populations. These findings have several important clinical implications. The moderate effect size (correlation of −0.40) observed in the reduction of sessions with the diode laser highlights its efficiency, requiring fewer patient visits than cryotherapy, similar to the Hemmatlan study [18]. This can improve treatment adherence and reduce costs and logistical burden for both patients and healthcare providers. Furthermore, the large effect size for pain reduction over time (η2 = 0.54) reinforces the overall effectiveness of both treatments in alleviating discomfort, while the absence of a significant interaction between treatment type and time (η2 = 0.01) suggests that pain reduction occurs similarly in both methods. These results allow clinicians to focus on other factors such as cost, duration, and patient preferences when tailoring treatment strategies.
In terms of safety, neither treatment caused serious complications, although there was a slight increase in pain in one patient in the LASEmaR group similar to other studies [18]. Previous studies had reported frequent adverse effects with cryotherapy such as pain, blistering, or postinflammatory depigmentation. For its part, the diode laser has demonstrated a good safety profile in other dermatologic applications [12, 18–20]. The present study observed a low incidence of complications, which is consistent with these findings. Cryotherapy has been associated with adverse effects due to extensive tissue damage, despite having fewer complications than electrodessication [37], whereas diode laser treatments are generally safer [18], with minimal side effects such as transient discomfort or mild redness. The standardized protocols and careful monitoring in our study likely contributed to minimizing the risks of both treatments, further supporting their safety profiles. Both treatments significantly reduced pain over time, although cryotherapy showed more pronounced initial relief, which could be relevant for patients seeking an immediate decrease in discomfort. However, no statistically significant differences in pain scores on the VAS were found between the two groups. Although there was a slight trend toward lower pain scores in the laser-treated group, this difference was not statistically significant. Previous studies suggest that lasers may be less painful because they do not involve skin freezing [23, 24, 35]; however, our findings do not allow definitive conclusions to be drawn in this regard, highlighting the need for larger studies to explore this aspect.
Future multicenter trials with larger sample sizes and extended follow-up periods are essential to validate these preliminary findings and to assess the long-term recurrence rates of plantar warts. In addition, future research should explore the efficacy of the treatment in subgroups, such as children and immunocompromised patients, as well as evaluate the potential of combining treatments. If the superiority of diode laser treatment is confirmed, clinical practice can be redefined by establishing the laser as a first-line noninvasive alternative, significantly reducing treatment duration, enhancing patient satisfaction, and prompting revisions to current treatment protocols for plantar warts.
4.1. Limitations
Although the sample size of the study was statistically adequate (44 participants), a larger sample size could have provided a clearer and more robust picture of the differences between treatments and a better representation of the general population. Additionally, the use of multiple statistical comparisons increases the risk of Type I errors, where significant differences are detected that do not actually exist. To address this, we applied Bonferroni adjustment, which is a conservative method to control for the overall error. Our key findings, such as the significant difference in the number of sessions required between treatments, remained robust after this adjustment. However, this approach may reduce the sensitivity of detecting subtle but clinically relevant differences, such as pain score variations. Future studies with larger sample sizes may provide greater statistical power and validate these findings. Moreover, these limitations in the study design may hinder the generalization of findings to broader populations and diverse clinical contexts, potentially limiting their applicability and relevance in various scenarios.
5. Conclusion
In conclusion, this randomized clinical trial demonstrated that diode laser treatment effectively removed plantar warts in fewer sessions than cryotherapy, highlighting its potential as a promising noninvasive alternative for recalcitrant lesions. These results are in line with the study objectives and highlight the selective mechanism of action of diode lasers, which may offer precision and efficacy advantages over traditional methods. Both treatments showed comparable safety and pain profiles, suggesting that diode lasers could be integrated into clinical practice as a viable option for the treatment of plantar warts. Multicenter studies with larger populations should be conducted to validate these results and assess their long-term safety and recurrence rates. These findings provide valuable insights into dermatological practice and pave the way for future research into innovative treatment modalities.
5.1. Randomization
To ensure the internal validity of the study and avoid bias, participants were randomly assigned to one of the two treatment groups: laser or cryotherapy. For this purpose, a computerized randomization system that generates randomization sequences using a pseudorandom number algorithm was used. This computer randomization approach is widely used in clinical trials, as it minimizes selection bias and balances known and unknown baseline characteristics between groups, thus ensuring an equal distribution of potential confounders. The randomization sequence was generated by an independent investigator not involved in the recruitment or evaluation of participants using Microsoft Excel. The assignment of participants to treatment groups was performed in a strictly sequential manner, following the order previously established by the randomized sequence generated. The randomization sequence was securely stored by the independent investigator in a protected file and was periodically reviewed to ensure strict adherence to the allocation process throughout the study. This ensured that all participants were assigned in accordance with the randomized sequence without deviations. Treatment procedures were carried out by trained investigators following standardized protocols for both laser and cryotherapy. These investigators were not involved in recruitment or posttreatment evaluations to maintain objectivity and consistency. To implement the single-blind design, participants were informed only that they would receive one of the two approved treatments for plantar warts, without revealing the specific method. Independent evaluators, blinded to the group assignments, conducted all posttreatment follow-up assessments. These evaluators were not present during treatment sessions and were instructed to avoid discussing treatment specifics with participants, ensuring unbiased assessment of outcomes. All randomization details, including participant assignments and sequence integrity, were documented and stored securely for potential audit and verification, ensuring transparency in the process.
Ethics Statement
All participants provided written informed consent prior to inclusion in the study. The study protocol was reviewed and approved by the Research Ethics Committee of the University of Valencia “San Vicente Mártir” (UCV/2022-2023/080), in compliance with the ethical principles of the Declaration of Helsinki.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
All authors were involved in the data interpretation and critical review of all manuscript drafts. They have also approved the final draft for submission and are accountable for the work’s integrity.
Funding
The authors would like to thank the University of Valencia “San Vicente Mártir” for the funding and support provided for the payment of the open access publication fee.
Acknowledgments
The authors would like to thank the University of Valencia “San Vicente Mártir” for the funding and support provided for the payment of the open access publication fee.
Open Research
Data Availability Statement
The data supporting the findings of this study are available at Mendeley Data and can be accessed using the following link: https://data.mendeley.com/preview/tx6pt4jfsn. These datasets have been deposited and are openly accessible for verification and further research. For any additional inquiries regarding the data, please contact the corresponding author of the manuscript.




