Evaluating the Efficacy and Safety of Kinesiology Tape Wrapping as Adjunct Therapy for Epidermal Growth Factor Receptor–Induced Paronychia
Abstract
Background: Current therapies for epidermal growth factor receptor inhibitor (EGFRI)–related paronychia demonstrate effectiveness; however, some patients respond poorly and experience recurrent painful granulation tissue, particularly in weight-bearing areas such as the big toes. Based on promising results from our previous pilot study by Hsu and colleagues, novel kinesiology tape wrapping, which physically shields the inflamed periungual tissue from irritation by the nail plate, has emerged as a potentially effective adjunct therapy.
Objectives: This open-label, randomized-controlled, single-center study was aimed to evaluate the efficacy and safety of kinesiology tape wrapping in cancer patients with EGFRI-related paronychia.
Materials and Methods: Eligible participants were assigned to receive either kinesiology tape wrapping in combination with conventional therapies or conventional therapies alone for 12 weeks. Efficacy outcomes, including the reduction of subjective pain assessed by the numerical rating scale (NRS) and the objective single-digit scoring system for paronychia related to oncologic treatments (single-digit SPOT), as well as adverse events (AEs), were recorded at baseline and at Weeks 1, 2, 4, 8, and 12 postenrollment.
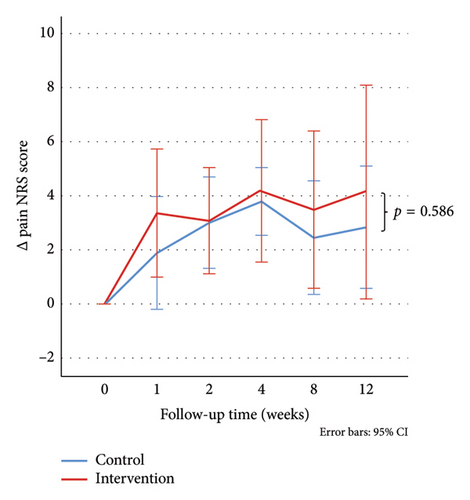
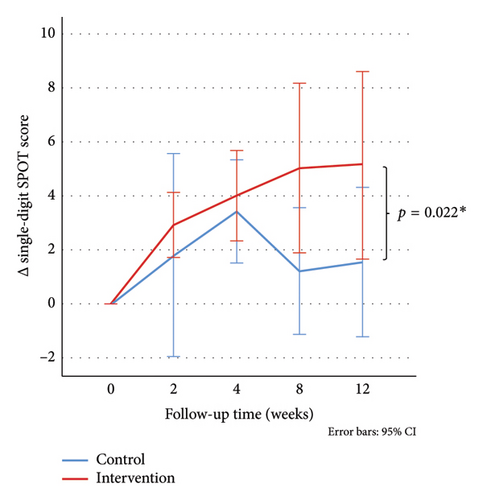
Results: A total of 24 patients were randomized, of which, 22 qualified for analysis. The rate of continuous tape use was 36.3%. At Week 12, pain NRS scores showed no significant differences between groups, while patients treated with continuous or intermittent kinesiology tape wrapping demonstrated notably greater reductions in single-digit SPOT scores compared to those receiving conventional therapy alone (NRS: 3.27 vs. 2.78, p = 0.586; single-digit SPOT: 5.32 vs. 1.52, p = 0.022). No serious AEs were reported.
Conclusion: Kinesiology tape wrapping is an effective and safe adjunct noninvasive therapy that offers additional benefits in managing EGFRI-related paronychia. Further studies with longer follow-ups and improved patient compliance may help fully evaluate its effectiveness in pain reduction.
Trial Registration: ClinicalTrials.gov identifier: NCT06411093
1. Introduction
Epidermal growth factor receptor inhibitors (EGFRIs) have emerged as effective antineoplastic agents for various malignancies, including non-small–cell lung cancer (NSCLC) and colorectal cancer [1]. For patients with EGFR-mutant advanced NSCLC, drugs such as gefitinib, erlotinib, afatinib, and dacomitinib are considered first-line treatments, offering higher response rates and delaying disease progression compared to conventional chemotherapy [1]. However, these agents may interfere with normal epithelium differentiation and migration, leading to a range of debilitating cutaneous adverse events (AEs), such as xerosis, acneiform eruption, and paronychia, significantly impacting patients’ quality of life (QoL). Dose reduction or treatment cessation due to severe or intractable AEs may adversely affect cancer treatment outcomes [1–3].
The incidence of paronychia among patients receiving EGFRIs ranges from approximately 3% to 58.1%, with rates and severity varying based on EGFRI type, dosage, and patient ethnicity [3–5]. For instance, dacomitinib demonstrates the highest incidence rate of paronychia (58.1%), followed by afatinib (33%–57%), osimertinib (22%–31%), erlotinib (4%–14%), and gefitinib (3%–14%) [3–7]. Asian populations tend to exhibit higher incidence rates than non-Asians, possibly due to a thinner stratum corneum [6]. The most common affected sites are big toes for their greater weight-bearing role. Different from common chronic paronychia, EGFRI-related paronychia may develop large pyogenic granuloma-like lesions. The granulation tissue can cause severe pain, bleed easily, and significantly impact daily activities [8]. Previous studies have indicated effective management strategies for EGFRI-related paronychia, including daily care practices such as emollient use, avoiding prolonged exposure to soapy water, and minimizing skin trauma. Topical medications such as ultrapotent corticosteroids, antiseptics, antibiotics, and topical beta-blockers are also recommended to reduce inflammation. Additional interventions such as cryotherapy, chemical cauterization with silver nitrate, and electronic cauterization may be necessary in cases of protuberant granulation tissue [1, 3, 8–11]. Despite these therapies, some patients may experience inadequate pain relief and recurrent granulation tissue, necessitating dose reduction and switching or discontinuation of EGFRIs. Although invasive interventions such as surgical partial matricectomy may be a viable option, they may be limited due to pain and the potential for creating additional wounds [12, 13].
To provide a noninvasive, well-tolerated, and sustained treatment option beyond exsiting conventional therapies, we introduced novel kinesiology tape wrapping as an adjunct therapy. In our preliminary study, we applied the tape to shield the inflamed nail folds from the nail plate following chemical cauterization of granulation tissue in four patients with refractory EGFRI-related paronychia. After a 3-week intervention, both pain and granulation tissue were markedly reduced, with a favorable safety profile [14]. Based on these encouraging findings, we here designed an open-label, randomized-controlled study to evaluate the clinical efficacy and safety of using kinesiology tape wrapping as an adjunct therapy to conventional treatments for cancer patients with EGFRI-related paronychia.
2. Materials and Methods
2.1. Study Design
This single-center, open-label, randomized-controlled study spanned a 12-week treatment period and enrolled patients with acute or chronic paronychia associated with EGFRIs. Participants were recruited from the dermatology outpatient clinic or oncology inpatient unit in Kaohsiung Chang Gung Memorial Hospital between March 2023 and December 2023. The study’s procedural details and safety outcomes have been previously reported [14]. The protocol was approved by the Institutional Review Board of Kaohsiung Chang Gung Memorial Hospital and adhered to the principles of the Declaration of Helsinki. Written informed consent was obtained from all participants in the study.
2.2. Eligibility Criteria
Patients aged 20 years or older with acute or chronic paronychia occurring during EGFRI therapy, involving at least one big toe, were eligible for inclusion. Paronychia severity was graded according to the National Cancer Institute’s Common Terminology Criteria for AEs (CTCAE) (Version 5.0 [15]) as Grade 2 or Grade 3. Inclusion criteria required granulation tissue on the big toe suitable for chemical cauterization with silver nitrate. Exclusion criteria encompassed patients with severe ingrown nails, concurrent cutaneous infections, severe nail destruction, or chronic paronychia with periungual fibrosis.
2.3. Interventions
Patients were randomly assigned to receive either a combination of kinesiology tape wrapping with conventional treatment (intervention group) or conventional treatment alone (control group) over a 3-month period. Simple randomization was performed using the coin toss method. Conventional treatment consisted of chemical cauterization with silver nitrate, with or without topical antiseptics, topical steroids, topical beta-blockers, short-term systemic antibiotics, and systemic corticosteroids. Topical agents were applied once or twice daily to swollen nail folds or granulation tissue. Short-term low-dose oral steroids were prescribed for severe and intolerable EGFRI-related side effects, including acneiform eruption. The frequency of silver nitrate application was coordinated with their routine outpatient visits. The visit was typically scheduled on the same day as the appointment with other specialists, or adjusted based on the severity of the paronychia. The interval between silver nitrate applications ranged from 1 to 8 weeks.
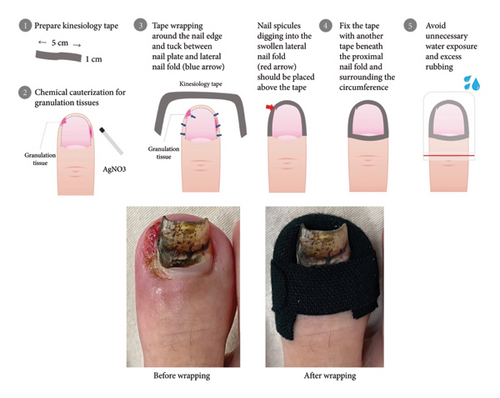
The application procedure for kinesiology tape was standardized as follows (Figure 1): First, the kinesiology tape was cut to the appropriate size, approximately 1 cm wide and 5 cm long, tailored to fit the patient’s nail size. Second, the silver nitrate was applied for chemical cauterization of protruding granulation tissues, ensuring the affected area was dry. Third, the kinesiology tape was carefully placed around the nail edge, tucked between the nail plate and inflamed lateral nail folds to promote separation, ensuring the nail spicules were positioned above the tape. Finally, the tape was secured with an additional piece of tape around the proximal nail fold, encircling the circumference of the big toe. Patients were subsequently instructed on proper care to prevent tape detachment, such as protecting the toe during showers and drying the toe if it became wet. During the tape placement, topical agents were withheld and resumed if the tape dropped off. The majority of applications were performed during outpatient visits. In cases of tape detachment, patients were instructed to either reapply the tape themselves following the provided instructions or wait until their next outpatient visit. The kinesiology tape applications were performed by the same operator (Ying-Hsiang Wang).
2.4. Assessments
We collected patients’ characteristics, including age, gender, primary cancer diagnosis, type of EGFRIs used, duration of EGFRI therapy prior to study enrollment, and details of current or prior treatments for paronychia from medical records. In addition, we recorded the total number of affected digits (fingernails or toenails) with lesions and the CTCAE grading of paronychia at baseline to provide a comparative assessment of initial paronychia severity.
To evaluate treatment response, we employed two outcome measures: (1) the numerical rating scale (NRS) for pain and (2) the scoring system for paronychia related to oncologic treatments (SPOT) (Table 1). The pain NRS score ranged from 0 to 10, with 0 indicating no pain and 10 indicating the most severe pain. The SPOT consisted of four parameters, including redness (R), edema (E), discharge (D), and granulation tissue (G), each rated on a 4-point scale (0–3), with 0 indicating no presence of signs and 3 indicating the most severe manifestation. While the original SPOT score represents the sum of scores of all digits, we apply it to assess the severity of a single digit, the enrolled big toe, in our study. The single-digit SPOT (single-digit SPOT) score ranged from 0 to 12 [16]. Dr. Ting-Jung Hsu and Dr. Ying-Hsiang Wang served as the outcome assessors.
| Scoring system for paronychia related to oncologic treatments (SPOT) | ||||
|---|---|---|---|---|
| Score | Redness (R) | Edema (E) | Discharge (D) | Granulation tissue (G) |
| 0 Absence | No erythema | No edema | No discharge | No granulation tissue |
| 1 Mild | Mild pink to light erythematous change | Mild swelling involving partial periungual tissue | Minimal wet and shiny texture from the lesion site | Minimal granulation tissue |
| 2 Moderate | More prominent erythematous change | More prominent swelling involving almost complete periungual tissue | Visible oozing discharge from the lesion site | Slightly protruding or vegetative granulation tissue |
| 3 Severe | Dark red to violaceous change | Deformed outline of the finger/toe due to severe swelling | Abundant discharge from the lesion site | Tumorous or nodular granulation tissue |
Data collection involved clinical examination and photography conducted at baseline and subsequently at 1, 2, 4, 8, and 12 weeks poststudy entry, either at the hospital or remotely via patient-submitted photos and phone contact if in-person visits were not possible. For practical reasons and to accommodate patient schedules, data collected within 1 week before or after the scheduled visits were considered acceptable. AEs were documented during each assessment.
Patients who became lost to follow-up or underwent a change in therapy to an alternative anticancer regimen such as chemotherapy during the study period were considered withdrawn from the study. Data collected up to the point of withdrawal were included in the final outcome analysis.
2.5. Statistical Analysis
In the descriptive analysis, continuous variables were presented as mean ± standard deviation, while categorical variables were presented as counts and percentages. Equality between the intervention and control groups was assessed using the Fisher’s exact test and the Mann–Whitney test. Differences in measured outcomes at each follow-up time point throughout the study and comparisons between the two groups were analyzed using generalized estimating equations (GEEs). Statistical analyses were performed using Statistical Package for the Social Sciences 25.0 software (IBM Corp., Armonk, NY), with statistical significance defined as a two-tailed p value of < 0.05 for all tests.
3. Results
3.1. Patient Characteristics
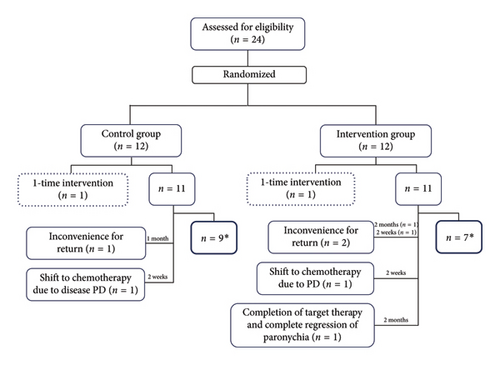
A total of 24 patients were included in the study, with 12 patients randomized into the intervention group and 12 into the control group. The overall study completion rate was 66.7% (n = 16). Each group had one patient who underwent only a single treatment and did not return for follow-up due to intolerable pain and inconvenience, respectively; thus, they were excluded from the results’ analysis. No patients discontinued early due to treatment-related AEs. The reasons for early study discontinuation included inconvenience for return (n = 3), shifting to chemotherapy (n = 2), and completion of EGFRI therapy within the study period (n = 1). Finally, nine patients in the intervention group and seven patients in the control group who continued EGFRI therapy completed 3 months of study treatment and follow-up (Figure 2).
Demographics and disease severity at baseline were similar between the two groups (Table 2). The majority of patients were elderly, with a median age of 70 years (range 40–87), and there was a female predominance with a ratio of 1.75:1. The primary diagnosis was lung adenocarcinoma (n = 20, 90.0%), followed by adenocarcinoma of the colon (n = 2) and lung squamous cell carcinoma (n = 1). EGFRIs used included mainly afatinib (n = 16), and others included dacomitinib (n = 2), osimertinib (n = 1), erlotinib (n = 1), cetuximab (n = 1), and panitumumab (n = 1). One patient in the intervention group transitioned to osimertinib 1 month after study entry due to intolerance to multiple AEs caused by afatinib (CTCAE Grade 2–3 diarrhea, Grade 2 acneiform eruption, and Grade 3 paronychia). In addition, one patient in each group experienced short-term discontinuation or dose adjustment of their EGFRI (less than 1 month) due to intolerable AEs (CTCAE Grade 3 vasculitis in the intervention group and CTCAE Grade 3 paronychia in the control group).
| Demographic and baseline clinical data | Control group (n = 11) | Intervention group (n = 11) | Overall (n = 22) | p value |
|---|---|---|---|---|
| Age (median, range, years) | 71 (40–87) | 69 (51–80) | 70 (40–87) | 0.392 |
| Gender | ||||
| Male | 2 | 6 | 8 | 0.183 |
| Female | 9 | 5 | 14 | — |
| Primary cancer | ||||
| Lung adenocarcinoma | 11 | 8 | 19 | 0.214 |
| Lung squamous cell carcinoma | 0 | 1 | 1 | — |
| Colon cancer | 0 | 2 | 2 | — |
| Anticancer treatment during the study period | ||||
| Afatinib | 9 | 6 | 15 | 0.361 |
| Dacomitinib | 2 | 0 | 2 | — |
| Osimertinib | 0 | 1 | 1 | — |
| Afatinib/osimertinib | 0 | 1 | 1 | — |
| Erlotinib | 0 | 1 | 1 | — |
| Cetuximab | 0 | 1 | 1 | — |
| Panitumumab | 0 | 1 | 1 | — |
| Short-term discontinuation or dose adjustment of EGFRI due to intolerable adverse events | 1 | 1 | 2 | — |
| Change to another EGFRI due to intolerable adverse events | 0 | 1 | 1 | — |
| Shift to chemotherapy due to disease progression | 1 | 1 | 2 | — |
| Duration of target therapy previously (median, range, months) | 7 (1–58) | 15.5 (3–110) | 10.5 (1–110) | 0.511 |
| Severity of paronychia | ||||
| CTCAE grade (n) | ||||
| Grade 2 | 8 | 8 | 16 | 1.000 |
| Grade 3 | 3 | 3 | 6 | — |
| Total number of fingers and toes with paronychia (mean) | 7.7 | 5.9 | 6.8 | 0.233 |
| Single-digit SPOT of enrolled big toe (mean) | 10.3 | 8.2 | 9.2 | 0.066 |
| NRS of enrolled big toe (mean) | 7.1 | 5.0 | 6.1 | 0.086 |
| Previous treatment (n) | ||||
| None | 3 | 0 | 3 | — |
| Topical steroid | 3 | 3 | 6 | — |
| Topical antiseptics | 6 | 11 | 17 | — |
| Topical beta-blockers | 5 | 6 | 11 | — |
| Oral antibiotics | 7 | 8 | 15 | — |
| AgNO3 chemical cauterization | 6 | 10 | 16 | — |
The overall median duration of continued EGFRI use prior to entry was 10.5 months (range: 1–110). All patients had at least CTCAE Grade 2 paronychia, with a mean involvement of 6.8 affected fingers or toes. The pain NRS and single-digit SPOT score of the studied big toe showed no baseline difference (7.7 vs. 5.9, p = 0.086; 10.3 vs. 8.2, p = 0.066).
3.2. Efficacy
In terms of pain as measured by the NRS, both the intervention and control groups demonstrated significant improvement from baseline at every follow-up time point, and the reduction in pain NRS showed an increasing trend (Table 3). Specifically, at Week 12, the average reduction in pain NRS was 3.27 (p = 0.01) in the intervention group and 2.78 (p < 0.01) in the control group. Although the intervention group exhibited a greater reduction in pain NRS compared to the control group at each follow-up time point, the difference was not statistically significant (p = 0.586) (Figure 3(a)). In terms of the single-digit SPOT score, the intervention group demonstrated significant improvement from baseline at every follow-up time point, with the reduction in single-digit SPOT score showing an increasing trend. Conversely, the control group showed significant improvement only at Week 4. The average reduction in single-digit SPOT score at Week 12 was 5.32 (p < 0.01) in the intervention group and 1.53 (p = 0.172) in the control group. Importantly, the difference in the reduction of single-digit SPOT scores between the two groups was statistically significant (p = 0.022) (Figure 3(b)).
| Outcomes | Time (weeks) | △pain NRS | △single-digit SPOT score | ||
|---|---|---|---|---|---|
| Mean | p value | Mean | p value | ||
| Control group | 0 | 0 | — | 0 | |
| 1 | 2.14 | 0.006∗ | — | — | |
| 2 | 3.07 | 0.001∗ | 1.97 | 0.091 | |
| 4 | 3.71 | 0.001∗ | 3.07 | 0.001∗ | |
| 8 | 2.32 | 0.006∗ | 1.16 | 0.211 | |
| 12 | 2.78 | 0.003∗ | 1.52 | 0.172 | |
| Intervention group | 0 | 0 | — | 0 | |
| 1 | 3.30 | 0.001∗ | — | — | |
| 2 | 3.09 | 0.001∗ | 2.91 | 0.001∗ | |
| 4 | 3.74 | 0.001∗ | 3.87 | 0.001∗ | |
| 8 | 3.20 | 0.006∗ | 5.06 | 0.001∗ | |
| 12 | 3.27 | 0.010∗ | 5.32 | 0.001∗ | |
3.3. Safety
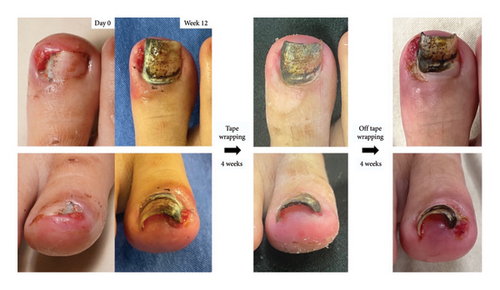
During the study period, no serious AEs were observed among the two groups. The most common side effect of kinesiology tape wrapping was skin irritation (90.9%), which included erythema and scaling, without pain or itching (Figures 4, 5, 6, and 7).


4. Discussion
This trial demonstrates that kinesiology tape wrapping, used in conjunction with conventional therapy, could offer additional therapeutic benefits for patients with EGFRI-related paronychia. Continuous or intermittent application of kinesiology tape wrapping over a 3-month period resulted in a mean reduction of 3.27 points in subjective pain assessed using the NRS, and a mean reduction of 5.32 points in the objective single-digit SPOT score. The difference between the intervention and control groups was statistically significant for the single-digit SPOT score (p < 0.05) but not for the pain NRS (p = 0.586). As shown in Figure 3(a), the intervention group experienced a more noticeable improvement in the first week, which appeared to be sustained throughout the observation period. The application of kinesiology tape may have facilitated separation between inflamed periungual tissue and painful nail contact points, potentially contributing to earlier pain relief and stabilization of symptoms. In contrast, the control group receiving only conventional therapy showed pain relief but continued to experience recurring granulation tissue, with a more tapering of improvement noted by Week 8 (Figures 3(a), 3(b)). The absence of a statistically significant difference in pain scores may be due in part to the limited follow-up duration. A longer observation period may help fully assess the treatment’s impact on pain.
In the control group, a higher proportion of patients received second-generation EGFRIs, including afatinib and dacomitinib, compared to the intervention group. While different EGFRIs are associated with varying incidences and severities of paronychia, our inclusion criteria consistently required at least CTCAE Grade 2 paronychia with granulation tissue on the big toe, minimizing discrepancies between groups. As shown in Table 1, the severity of paronychia did not differ significantly between the groups. Furthermore, two patients in the control group with severe granulation tissue, who rigorously adhered to kinesiology tape wrapping poststudy, reported significant pain relief by Week 2 and near-complete regression of granulation tissue by Week 4, suggesting a potential additional therapeutic benefit of kinesiology tape wrapping (Figure 4).
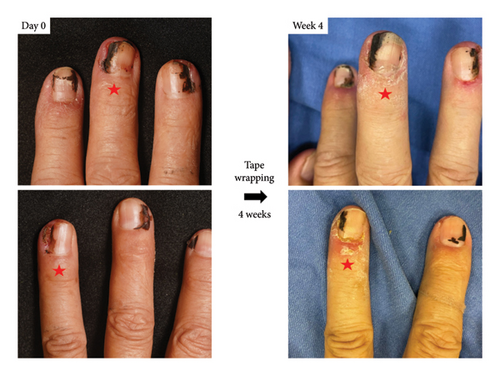
Our observations further indicated that three out of four patients with mild granulation tissue (G = 1) achieved complete resolution with kinesiology tape wrapping. Notably, two of these patients experienced notable efficacy, achieving complete remission by Week 2 and Week 4, respectively, with no recurrence during the subsequent follow-ups (Figure 5). This suggests that early intervention with tape wrapping in cases of mild granulation tissue may increase the likelihood of achieving complete remission in a shorter timeframe and reduce the risk of disease progression.
In the intervention group, a patient with severe granulation tissue maintained high compliance, ensuring continuous application of the tape in the correct position for 12 weeks and experiencing rapid pain resolution by Week 2. However, improvement in the granulation tissue was slower, with mild residual granulation tissue persisting after more than 4 weeks of tape wrapping following study completion. Progressive changes indicative of an ingrown nail were observed on the lateral aspect of the big toe (Figure 6). Similarly, in the previously mentioned two patients in the control group, who showed improvement after 4 weeks of kinesiology tape wrapping poststudy, recurrence with ingrown nail changes was noted 4 weeks after discontinuation (Figure 4).
Previous studies have suggested that the mechanism underlying EGFRI-related paronychia is multifaceted, involving impaired keratinocyte migration and proliferation, increased expression of inflammatory mediators, and weakened immune barriers [1, 17–19]. These factors result in a thinner, more fragile epidermis and reduced periungual tissue protection against the nail plate. Consequently, repetitive irritation leads to reactive capillary proliferation and the formation of painful granulation tissue, with ulcerative wounds becoming susceptible to secondary infections [19]. Moreover, EGFRIs also impact nail plate growth and integrity, leading to brittle or broken nails. Inflammation may be exacerbated if a broken nail penetrates the periungual tissue.
In our investigation, the efficacy of tape wrapping in creating a barrier between the nail plate and periungual tissue appears to reduce repetitive mechanical irritation and associated periungual inflammation. This method can be applied not only to the big toes but also to other digits, which also showed clinical improvement (Figure 7). We selected the big toe for the study design to ensure standardized comparison. However, in cases of severe granulation tissue accompanied by structural deformities of ingrown nail changes, as illustrated in Figures 4 and 6, the utility of kinesiology tape for achieving complete resolution may be limited. This limitation likely stems from biomechanical stresses, particularly in the big toe, which bears significant weight during normal gait phases. Specifically, the big toe bears twice the load of the other toes, accounting for approximately 40%–60% of body weight during the stance phase of gait, and up to 80% of body weight during the toe-off phase of normal walking [20]. The mechanical support provided by kinesiology tape may be insufficient to counteract these forces on the fragile periungual tissue, leading to ingrown nail changes and chronic refractory paronychia. Nevertheless, kinesiology tape remains valuable for maintaining disease control, as demonstrated by the absence of disease progression during an additional 4-week tape-wrapping management in Figure 6. Adjunctive interventions, such as orthonyxia or partial nail avulsion, may be beneficial for achieving complete remission. However, several factors must be considered, including patient preferences, financial limitations associated with orthonyxia, and the risk of chronic wound development. Further studies are needed to validate this combined approach in the management of EGFRI-related chronic refractory paronychia.
Kinesiology tapes, which are thin, waterproof, flexible, and hypoallergenic, can adhere firmly to the skin for days while leaving minimal adhesive residue upon removal. Their tensile strength from lengthwise stretching and minimal joint restriction contributes to their widespread use in the management of sports injuries [21]. Rather than focusing on their tensile properties, we selected the kinesiology tape for its ability to create a robust separation between the inflamed nail folds and the nail plate. Furthermore, kinesiology tapes are easily accessible and can be purchased at pharmacies or online. Compared to conventional taping methods, our approach avoids crossing the distal phalangeal joint and imposes minimal restrictions on daily activities such as walking, cycling, or simple exercises. This allows the tape to adhere firmly to the nail border for a relatively longer period, reducing the need for frequent replacement and potentially enhancing patient adherence. The average duration of continuous tape placement ranged from 1 to 3 weeks, influenced by factors such as patient age and self-care ability. Skin irritation was the most common complication (90.9%), including asymptomatic erythema and scaling, with severity influenced by the duration of tape application and personal skin conditions. All irritation events resolved within a few days after tape removal. The use of moisturizers was sufficient to alleviate symptoms, without the need for other pharmacotherapeutic agents. No serious AEs were observed during the study period, indicating the safety of kinesiology tape placement.
Study limitations include its single-center design, small sample size, and short follow-up duration, which may have impacted the accurate detection of between-group differences. The open-label design also introduces the possibility of performance and observer bias. The distance from the hospital hindered some patients from attending scheduled follow-ups, resulting in missing data (22.2%). In addition, the majority of patients were elderly, with 72.7% of the cohort over 60, posing challenges in managing kinesiology tape placement at home and contributing to suboptimal adherence, resulting in a low rate of continuous tape use (n = 4/11), which may also attenuate the observed effect. To improve adherence in future clinical applications, standardized protocols that include step-by-step visual guides or hands-on instruction for patients or their caregivers, with support from clinical staff as needed may help the learning. We also developed an instructional video, which can be reviewed at home (Supporting Information 1). Studies with larger cohorts, extended follow-up periods, rigorous monitoring strategies, and blinded assessments will help to mitigate these biases.
5. Conclusion
In conclusion, our findings demonstrate that kinesiology tape wrapping, in conjunction with conventional therapy, effectively reduces pain and severity in EGFRI-related paronychia with a good safety profile. Also, its hypoallergenic waterproof and flexible properties allow for sustained use without restricting joint mobility or requiring frequent replacement, offering greater comfort and convenience for patients. This investigation provides a valuable treatment option for first-line pulmonologists, oncologists, and dermatologists in managing EGFRI-related paronychia.
Ethics Statement
The study was approved by Chang Gung Medical Foundation’s Institutional Review Board (202001747A3). All participants gave written informed consent to participate in the research and publish the results.
Consent
Please see the Ethics Statement.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
All authors contributed to the study conception and design. Investigation and data curation were performed by Ying-Hsiang Wang and Ting-Jung Hsu. Statistical analysis was conducted by Ying-Hsiang Wang in collaboration with the Biostatistics Center at Kaohsiung Chang Gung Memorial Hospital. The first draft of the manuscript was written by Ying-Hsiang Wang and all authors contributed to the critical revision and editing of previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
No funding was received for this manuscript.
Acknowledgments
We would like to express our appreciation to the patients and their families, Dr. Lai-San Wong for referring patients to participate in this study, the Biostatistics Center at Kaohsiung Chang Gung Memorial Hospital for their invaluable assistance with the statistical work, and James Waddell for his English consulting and proofreading assistance.
Supporting Information
Supporting Information 1: Instructional video demonstrating the step-by-step procedure for kinesiology tape wrapping in the management of epidermal growth factor receptor inhibitor (EGFRI)–related paronychia.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.




