Efficacy of Punch Excision Combined With Superficial X-Ray for the Treatment of Keloids: A Single-Center Retrospective Study
Abstract
Background: Keloid management remains a challenge for clinicians. Recently, punch excision and photoelectric technology have demonstrated promising clinical applications for managing keloids; however, few studies have examined the efficacy and safety of punch excision combined with superficial X-ray for treating keloids.
Objective: To investigate the efficacy and safety of punch excision combined with superficial X-ray for treating keloid.
Methods: In this retrospective study, we analyzed the clinical records of 60 patients with keloid scars who underwent punch excision combined with superficial X-ray at our hospital, from April 2020 to April 2023. The Vancouver Scar Scale (VSS) and Patient and Observer Scar Assessment Scale (POSAS) 2.0 Patient Scale serve as the primary assessment tools to evaluate all patients, both prior to the initial treatment and one year after the completion of therapy. SPSS software was used for statistical analysis to assess keloid improvement.
Results: In the 60 patients with keloids, varying degrees of improvement were observed. The VSS and POSAS scores recorded 1 year after treatment were significantly lower than the pretreatment scores (p < 0.001). No severe adverse reactions were observed during treatment.
Conclusion: The combination of punch excision and superficial X-ray demonstrated a notable therapeutic effect on keloids without evident adverse reactions, offering a safe and effective option for patients with keloids.
Trial Registration: Chinese Registry of Clinical Trials: ChiCTR2400094289
1. Introduction
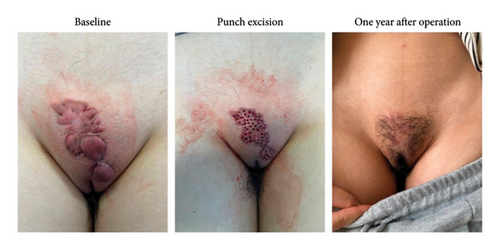
Keloids are benign fibroproliferative skin tumor, with an incidence of 4%–16% [1, 2]. Keloids are more likely to occur at high-tension sites and in those 10–30 years [3, 4]. Clinically, patients with keloids are frequently subjected to itchiness and pain, with the risk of disfigurement potentially leading to anxiety and depression [5]. The management of keloids is a clinical challenge, and there is no universally accepted treatment algorithm. Intralesional triamcinolone is the major first-line therapy for keloids and can be combined with intralesional 5-fluorouracil [6, 7]. Additionally, cryosurgery, pulsed dye laser, and radiation therapy have been successfully used in the treatment of keloids [8, 9]; however, these therapies are not feasible for multifocal keloids, especially those in particular area such as the vulva.
Recently, several studies have demonstrated the efficiency of punch excision combined with cryotherapy, intralesional steroid injection, and single fractional electron beam radiotherapy for the treatment of keloids [10–13]. Herein, we retrospectively analyzed the efficiency and safety of punch excision combined with superficial X-ray in the treatment of keloids, offering a novel therapy option for patients with keloid.
2. Materials and Methods
2.1. Clinical Data and Ethics Approval
Sixty patients diagnosed with keloid using the Darzi criteria who underwent punch excision combined with superficial X-ray at our hospital were enrolled [14], including 18 females and 42 males. The distribution of keloids was as follows: 25 cases on the mandible, 21 on the chest, five on the mons pubis, four on the shoulder and back, two on the ear, two on the arm, and one on the buttocks. The age of the participants ranged from 18 to 49 years, with an average age of 26 years. We evaluated the efficacy of the novel treatment according to pictures recorded pretreatment and 1-year post-treatment in outpatients.
This study was approved by the institutional review board of our institution (2024-KY-066), and the requirement for informed written consent was waived. We certify that this study was conducted by the Declaration of Helsinki.
2.2. Inclusion Criteria
(1) Patients > 18 years, (2) patients diagnosed with keloids that received punch excision combined with superficial X-ray therapy in our hospital between April 2020 and April 2023, and (3) patients with at least 1 year of follow-up and complete clinical data.
2.3. Exclusion Criteria
(1) Patients who are no longer under follow-up, (2) patients with < 1 year of follow-up, and (3) patients who received additional treatment during the 1-year follow-up period.
3. Methods
3.1. Punch Excision
All 60 patients received intralesional triamcinolone without any improvement prior to the novel treatment. After achieving satisfactory local anesthesia with 1% lidocaine mixed with epinephrine (1:100,000), a 2 mm punch biopsy device was used to perforate the keloid tissue as deeply as feasible, ensuring uniform and dense perforation across the entire keloid surface with an approximate 2.0 mm spacing between each hole [15]. After the punch excision was completed, the wound was covered with sterilized petrolatum gauze of an appropriate size (produced by Zhejiang Zhende Medical Co., Ltd.). Subsequently, it was further covered with a layer of gauze and wrapped with a pressure bandage. On the day after radiotherapy, the wound was cleaned with normal saline, and then covered with sterilized petrolatum gauze again. Thereafter, the dressing was changed every 2–3 days until the wound healed.
3.2. Superficial X-Ray
A superficial X-ray radiotherapy was administered within 24 h of the surgical procedure, targeting the operative area. A single fraction of 5 Gy was administered to all patients. The treated area was irradiated weekly for five sessions with the same single fraction.
3.3. Evaluation Index
Follow-up was conducted through outpatient for a minimum duration of 1 year. Follow-up photographs were obtained during outpatient visits, with the patient’s explicit consent. This study focused on two outcomes. The first was the conditions of keloids, which was assessed by observers using the Vancouver Scar Scale (VSS) at baseline and 1 year postoperatively. Second, patient satisfaction was assessed using the Patient and Observer Scar Assessment Scale (POSAS) 2.0 Patient Scale. The patients were followed up, and their outcomes were evaluated by asking them to rate their self-assessment based on the POSAS 2.0 Patient Scale [16].
The monitoring of adverse reactions primarily focused on the presence of telangiectasia, skin atrophy, pigmentary alterations, purpura, and infection.
3.4. Statistical Methods
Statistical analyses were performed using the Statistical Package for the Social Sciences software. Categorical variables are expressed as the number of cases and percentages (n [%]), which were assessed using the chi-squared test. The Shapiro–Wilk test was used to test whether the samples of the numerical variables conformed to a normal distribution: those that conformed to a normal distribution are expressed as (x ± s) and assessed using the t-test; those that did not conform to a normal distribution are expressed as median (interquartile range) and were assessed using the nonparametric rank-sum test. p value of < 0.05 was considered statistically significant.
4. Results
4.1. Primary Outcome
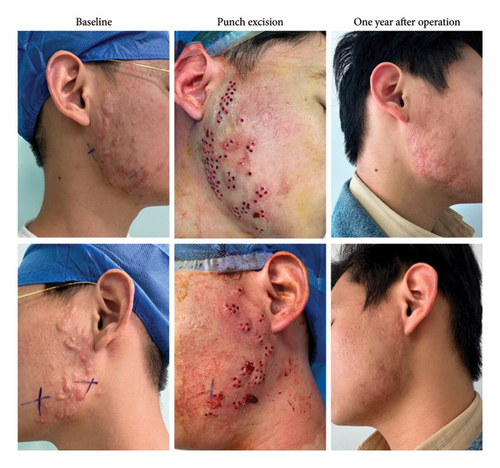
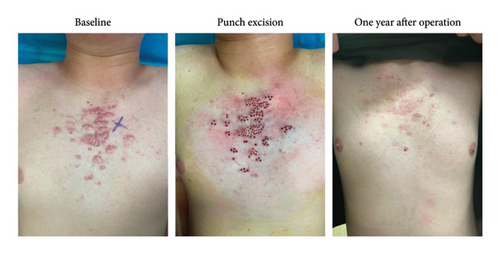
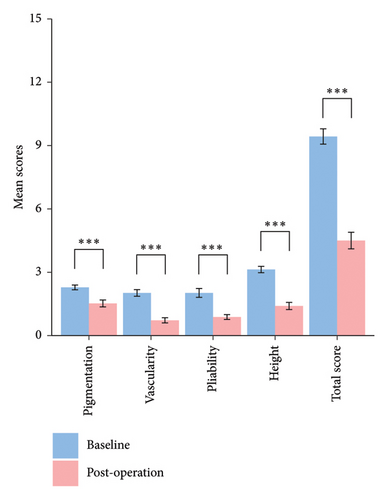
Sixty patients with keloids were included in this study. Varying degrees of improvement were observed in all patients, and the representative baseline, punch excision, and postoperative views are shown in Figures 1, 2, 3. The VSS score was (9.43 ± 1.43) prior to treatment and (4.50 ± 1.55) 1-year post-treatment. The differences in the VSS score between pretreatment and post-treatment were statistically significant (p < 0.001). The exact statistical changes are shown in Table 1, Figure 4 and Supporting Table 1.
| Vancouver scar scale | Baseline | Postoperation | Statistical difference | ||
|---|---|---|---|---|---|
| Mean scores | SD | Mean scores | SD | p | |
| Pigmentation | 2.28 | 0.45 | 1.52 | 0.65 | < 0.001 |
| Vascularity | 2.02 | 0.62 | 0.72 | 0.49 | < 0.001 |
| Pliability | 2.02 | 0.83 | 0.88 | 0.45 | < 0.001 |
| Height | 3.13 | 0.60 | 1.40 | 0.67 | < 0.001 |
| Total score | 9.43 | 1.43 | 4.50 | 1.55 | < 0.001 |
4.2. Secondary Outcome
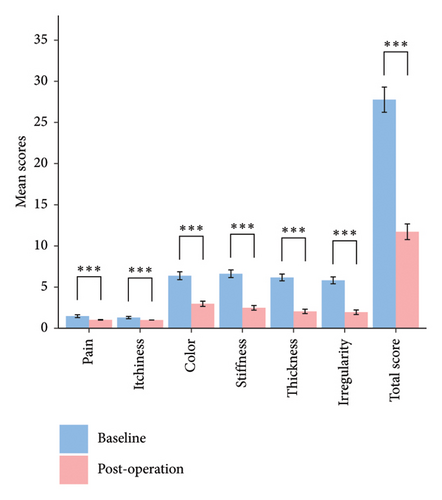
The combination therapy resulted in a statistically significant improvement in most item scores on the POSAS 2.0 scale, including pain, itchiness, color, stiffness, thickness, and irregularity of the patient scale (p < 0.001). The exact statistical changes are summarized in Table 2, Figure 5 and Supporting Table 2.
| POSAS 2.0 patient scale | Baseline | Postoperation | Statistical difference | ||
|---|---|---|---|---|---|
| Mean scores | SD | Mean scores | SD | p | |
| Pain | 1.47 | 0.68 | 1.02 | 0.13 | < 0.001 |
| Itchiness | 1.30 | 0.56 | 1.00 | 0.00 | < 0.001 |
| Color | 6.38 | 1.90 | 2.97 | 1.25 | < 0.001 |
| Stiffness | 6.62 | 1.83 | 2.48 | 1.13 | < 0.001 |
| Thickness | 6.17 | 1.62 | 2.05 | 1.03 | < 0.001 |
| Irregularity | 5.82 | 1.64 | 1.95 | 1.10 | < 0.001 |
| Total score | 27.77 | 6.05 | 11.72 | 3.76 | < 0.001 |
4.3. Adverse Reactions
No significant adverse effects were observed in all 60 patients, with most minor adverse reactions presenting as hyperpigmentation (three patients) and skin atrophy (two patients).
5. Discussion
Keloids are fibroproliferative disorders that may arise after deep cutaneous injury [17]. While the exact mechanism of keloids remains unclear, researchers have increasingly realized the role of chronic inflammation and mechanical forces in the development of keloids [18, 19]. Conventional therapeutic modalities, including cryotherapy and intralesional steroid injection, primarily serve to alleviate inflammatory processes, whereas surgical excision can reduce local skin tension to facilitate the desired therapeutic outcome.
This retrospective study was conducted to investigate the clinical efficacy and safety of an innovative therapeutic modification, punch excision combined with superficial X-ray, for the treatment of keloids. Sixty patients were enrolled according to the inclusion and exclusion criteria, including patients with keloids at a variety of sites, including the mandible (25 cases), chest (21 cases), vulva (five cases), back and shoulder (four cases), arms (two cases), ear (two cases), and buttocks (one case). All the patients showed varying degrees of improvement without severe adverse reactions.
Based on the currently accepted pathogenesis of keloids, the presumed mechanisms of this novel therapy contribute to several key aspects. First, punch excision is an effective and minimally invasive technique for the removal of substantial quantities of keloid tissue. The formation of a local mesh structure following punch excision holds the potential to notably alleviate and disperse local skin tension, thereby diminishing the likelihood of recurrence [4]. Additionally, punch excision can preserve a portion of the skin tissue, it contains important components such as skin appendages (hair follicles, sebaceous glands, and sweat glands) and viable fibroblasts. The former can act as a source of stem cells, differentiating into various cell types needed for wound repair [20]. The latter can secrete extracellular matrix components, facilitating rapid wound recovery in the subsequent stages [21]. Moreover, the local mesh-like structure formed after punch excision can improve blood circulation in the wound area, bringing more nutrients and immune cells to the wound site, which is conducive to rapid wound recovery, shortening the risk of secondary infection, and reducing the duration of inflammation [22]. Finally, given the limited penetration depth of superficial X-ray irradiation, punch excision favors the penetration of X-ray to induce fibroblast apoptosis, ultimately yielding a synergistic therapeutic effect [23].
While this study provided valuable insights, it had some limitations. Firstly, as a retrospective study, our investigation was confined to assessing the overall clinical efficacy of punch excision combined with superficial X-ray for the treatment of keloids. A comparative analysis of the potential variations in treatment response among keloids located at different sites has not yet been undertaken. Secondly, our study only included clinical data from the pretreatment phase and a 1-year follow-up period, posing challenges in accurately determining the precise recurrence rate of treatment. Furthermore, achieving complete penetration of the affected tissue solely through punch excision can be demanding in cases of keloids with greater thickness. Conventional surgical excision remains the primary therapeutic approach; however, we postulate that punch excision could serve as a viable adjunctive treatment to surgical excision, particularly in patients who have experienced recurrence following surgical intervention and those in the early stages of recurrence. Additionally, due to limited data, this study only evaluated the efficacy and safety data of punch excision combined with superficial X-ray treatment in a real-world clinical setting. A prospective controlled study is needed to further compare its efficacy with that of traditional surgical excision combined with X-ray.
In this study, hyperpigmentation (three patients) and skin atrophy (two patients) were most common adverse reactions. The activation of melanocytes caused by X-ray, individual differences among patients (such as those with darker skin tones), and the irradiated areas (the front of the chest and the mandible) are related to the occurrence of the former [24, 25]. The latter is a typical manifestation of radiation dermatitis, which is related to the excessive degradation of skin fibroblasts and collagen caused by X-rays [24]. It can be avoided by controlling the total irradiation dose.
Overall, this study demonstrates that punch excision combined with superficial X-ray is an effective and safe option for keloid treatment. This novel treatment is less painful and more acceptable to patients than punch excision combined with drug injection or cryotherapy. Additionally, this approach is less invasive, facilitates quicker healing, and is less technically demanding than traditional surgical excision, making it a convenient option for clinical use.
6. Conclusion
The combination of punch excision and superficial X-ray demonstrated a notable therapeutic effect on keloids without evident adverse reactions, thus offering a safe and effective option for patients with keloids.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
No funding was received for this research.
Acknowledgments
We would like to thank Editage (https://www.editage.cn) for English language editing.
Supporting Information
Additional supporting information can be found online in the Supporting Information section.
Open Research
Data Availability Statement
The data that supports the findings of this study are available in the Supporting Information of this article.




