Primary Orbital Teratoma With Congenital Anophthalmia in a Neonate: A Rare Case With Histopathological and Radiological Correlation
Abstract
This case report describes a rare instance of primary orbital teratoma with anophthalmia in a neonate. A 6-day-old female presented with a congenital right orbital swelling and absence of visible ocular structures. MRI revealed a large, well-vascularized orbital mass without intracranial extension, accompanied by malformations in the right cerebral hemisphere. Histopathological examination confirmed a benign, mature/mixed teratoma comprising elements from all three germ layers, including neuroectoderm, mesoderm, and endoderm, with no evidence of malignancy. The patient underwent successful orbital exenteration with an implant at 3 weeks of age.
1. Introduction
Orbital teratomas are rare congenital tumors accounting for approximately 1% of orbital masses in children. They originate from pluripotent germ cells and can present as primary or secondary tumors, with primary teratomas arising directly within the orbit and secondary ones extending from intracranial or nasopharyngeal regions [1, 2]. Histologically, these tumors contain tissues from all three germ layers and can be classified as mature, immature, or mixed based on cellular differentiation [3, 4]. While most cases are benign, immature teratomas may exhibit malignant potential [5, 6].
Clinically, orbital teratomas manifest at birth as unilateral orbital swelling, often accompanied by anophthalmia or microphthalmia [7]. Imaging and histopathological evaluation are critical for diagnosis and management. Surgical excision remains the treatment of choice to prevent complications such as vision loss, proptosis, and potential malignancy [8, 9]. This report presents a rare case of a congenital primary orbital teratoma with anophthalmia, detailing its clinical presentation, histopathological findings, and surgical management.
2. Case Report
A 6-day-old female infant was referred to the University Children’s Hospital in Belgrade in February 2019 due to right orbital swelling present since birth. The infant had no other visible anomalies, and her family history was unremarkable. The pregnancy was full term and uneventful, with delivery by cesarean section. At birth, the baby weighed 2390 g, measured 49 cm, and had a head circumference of 32 cm, with an Apgar score of 8. Initial abdominal ultrasonography and laboratory tests were normal. The mother was HIV negative based on standard antenatal screening, and the neonate was not exposed to HIV during pregnancy.
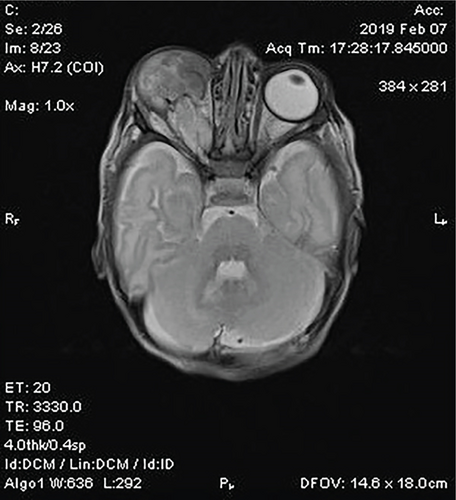
Ophthalmological examination revealed a significant right orbital mass. The eyelids were tightly closed, and the structures of the right eyeball were not visible. The left eye was unremarkable (Figure 1).

MRI of the orbit demonstrated a large, heterogeneous, well-vascularized mass in the right orbit measuring 25 × 17 × 33 mm. The mass caused remodeling of the orbital walls but no infiltration. The right optic nerve was fully developed and partially infiltrated, with a slightly thicker optic tract compared to the left side. Structures of the right eyeball were absent. Additional findings included cerebral malformations in the right hemisphere, such as irregular gyration of the occipital lobe, reduced volume of the lower temporal and parahippocampal gyri, focal cortical dysplasia, and partial agenesis of the corpus callosum. No evidence of intracranial tumor extension was observed (Figure 2).
At 3 weeks of age, the patient underwent an excisional biopsy, performed as an eyelid- and conjunctiva-sparing orbital exenteration with orbital implant placement. The postoperative course was uneventful, and no adjuvant therapy was deemed necessary after histopathological confirmation of the diagnosis.
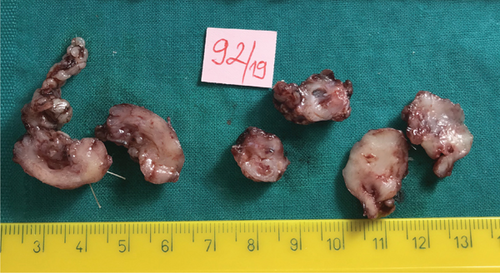
Gross examination revealed three biopsy specimens, the largest measuring 25 × 16 × 17 mm. The cut surface of the specimens appeared gelatinous and whitish (Figure 3).
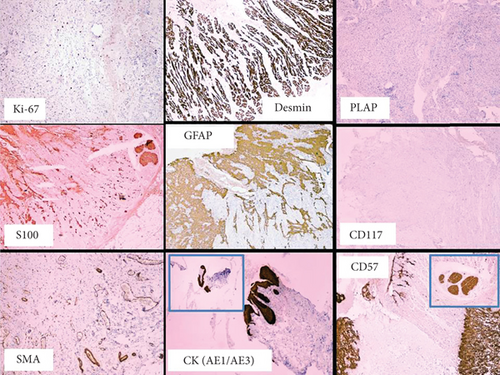
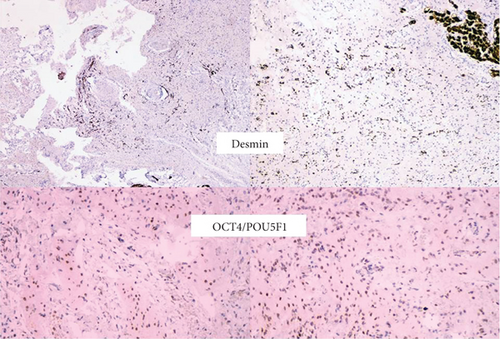
Microscopically, the tumor was not encapsulated and consisted of mature stromal elements derived from all three germ layers: neuroectoderm (brain tissue, nerves, choroid plexus, and ependyma), mesoderm (connective tissue, fat, and striated muscle), and endoderm (gastrointestinal and respiratory epithelium). Immature stromal and glial components were also present, but no cellular atypia or mitotic activity was observed. Ocular structures, surface ectoderm components, or malignant features were not identified (Figures 4 and 5).
Based on the clinical, imaging, and histopathological findings, a diagnosis of congenital, primary orbital, benign, mature/mixed teratoma with anophthalmia and no intracranial extension was established.
3. Discussion
Orbital teratomas are rare congenital tumors that present diagnostic and therapeutic challenges due to their complex histopathological features and potential associations with craniofacial anomalies. These tumors arise from misdirected or ectopic primordial germ cells or pluripotent stem cells that differentiate into tissues from all three germ layers: ectoderm, mesoderm, and endoderm [1, 2]. Teratomas are classified as mature, immature, or mixed based on the degree of tissue differentiation and can exhibit a benign or malignant clinical course [3–12].
Mature orbital teratomas, like the one in this case, are typically benign and well-differentiated, comprising a variety of tissue types, such as brain tissue, adipose tissue, and epithelium. Immature teratomas, on the other hand, contain immature neuroepithelial elements and may demonstrate a higher risk for malignancy [3, 5]. The grading of immature teratomas, based on the extent of immature neuroepithelial tissue, aids in determining the prognosis and the need for additional therapeutic interventions [5, 6].
The management of orbital teratomas relies on early and complete surgical excision to preserve function and prevent potential complications, such as compression of adjacent structures or malignant transformation [3, 4, 7, 8, 10]. In this case, the successful orbital exenteration performed at 3 weeks of age resulted in the complete tumor removal without recurrence or the need for adjuvant therapy. Postoperative outcomes were favorable, underscoring the importance of early diagnosis and intervention in such cases.
The immunohistochemical findings in this case demonstrated positive staining for mesodermal markers, such as desmin and SMA, along with the embryonic stem cell marker OCT4/POU5F1, confirming the diagnosis of a mature teratoma. These findings align with previously reported cases, highlighting the role of immunohistochemistry in supporting histopathological evaluation, although it is not diagnostic on its own [2, 6].
To date, only one other case of a mature primary benign orbital teratoma associated with anophthalmia has been reported, in a 7-year-old girl with a history of an orbital mass since birth [4]. The current case adds to the limited literature, emphasizing the rarity of such tumors and the need for meticulous clinical, radiological, and histopathological evaluation to ensure accurate diagnosis and optimal management.
While orbital teratomas have not been directly associated with perinatal HIV exposure, studies suggest that HIV-exposed but uninfected neonates may have altered immune profiles, potentially increasing their vulnerability to various neoplasms. Vertical transmission of HIV and maternal immunosuppression have been linked to higher risks of malignancies in early childhood, including rare tumors [13, 14]. In our case, the mother tested HIV negative during pregnancy, and the neonate was not HIV exposed. Nevertheless, it remains crucial to consider maternal HIV status in the comprehensive evaluation of congenital tumors.
4. Conclusion
This case highlights the clinical presentation, imaging characteristics, and histopathological features of a rare primary orbital teratoma with anophthalmia in a neonate. Early surgical excision remains the cornerstone of treatment, yielding favorable outcomes and preventing complications. Comprehensive histopathological analysis, supported by immunohistochemistry, is essential for accurate diagnosis and classification of these rare tumors. This report contributes to the limited body of literature on orbital teratomas and underscores the importance of multidisciplinary management in achieving optimal patient outcomes.
Ethics Statement
Informed consent was obtained from the patient’s parent, and assent was secured from the patient for participation in this case study, including the online open-access publication of images and related details. This report did not contain any personal information or patient identifiers.
Disclosure
The authors have nothing to report.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
D.M.R. performed the ophthalmologic evaluation, participated in the pathological examination and clinical decision-making, and supervised the manuscript preparation and the final review. D.D.V. wrote the original draft of the manuscript, conducted the literature review, and coordinated the interdisciplinary management of the case. M.K. performed the surgical procedure, participated in the clinical follow-up of the patient, and contributed to data collection.
Funding
No funding was received for this manuscript.
Acknowledgments
The authors have nothing to report.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.




