In-Hospital Outcomes of Hip Arthroplasty for Femoral Neck Fractures in Young Adult Patients: A Nationwide Study
Abstract
Introduction: Femoral neck fractures (FNFs) in young adults are relatively uncommon but pose significant clinical and surgical challenges. Hip arthroplasty is rarely used as a treatment option in this population but has seen rising use over the previous decade. This study seeks to compare hip arthroplasty outcomes among young adult patients in the United States admitted with FNF by evaluating hip hemiarthroplasty (HHA) and total hip arthroplasty (THA).
Materials and Methods: Using the National Inpatient Sample (NIS) data, adult patients less than 50 years old who underwent HHA or THA from 2016 to 2020 were analyzed. Both groups’ postoperative length of stay (pLOS), total hospital charges, and prosthesis-related complications (PRCs), including mechanical loosening (ML), prosthesis dislocation (PD), and periprosthetic fracture (PPF), were analyzed and compared.
Results: Out of 174,776,205 hospitalizations between 2016 and 2020, 15,590 young adult patients had FNF, and 2970 patients (2.18%) underwent hip arthroplasty (1195 HHAs and 1775 THAs). After controlling for demographic, clinical and hospital characteristics, HHA was associated with a 22.4% longer pLOS compared to THA [rate ratio: 1.224, 95% CI: 1.183 to 1.266; p < 0.001]. Patients in the HHA group also had higher odds of PPF (aOR: 9.06, 95% CI: 4.21, 19.48; p < 0.001). Conversely, patients in the THA group had higher odds of PD (aOR: 6.00, 95% CI: 1.78, 20.24; p = 0.004). There was no statistically significant difference in total hospital charges between the groups [cost ratio: 1.03, 95% CI: 0.995 to 1.075; p = 0.092].
Conclusion: Among young adults with FNF undergoing hip arthroplasty, HHA is associated with a longer postoperative hospital stay and higher risk of PPF as a major early complication, while THA is associated with a higher risk of PD. Financial burden is comparable for both procedure groups. When hip arthroplasty is a preferred treatment for FNFs, individual patient factors are important considerations that should guide the choice of procedure.
1. Introduction
Femoral neck fractures (FNFs) in young adults < 50 years are relatively rare fractures that often result from high-velocity trauma and may be a part of poly-trauma, with multiple fractures, including the ipsilateral femur [1, 2]. FNF patterns in the elderly differ from FNF patterns in young adults. Due to poor bone quality and low-energy injury mechanisms in elderly patients, a subcapital or mid-cervical FNF pattern is more common. Young adults typically have a basi-cervical, vertically oriented FNF pattern because of better bone quality and a higher energy mechanism [3, 4].
Over 330,000 hip fractures, half of which are FNFs, occur annually in the United States (U.S.) and are projected to double by 2050 [1, 5, 6]. Only 2%-3% of all FNFs occur in young adults [3]. Of all young adults with FNFs, only about 4% are treated with hip arthroplasty [7]. However, recent study findings indicate a rising use of hip arthroplasty, especially total hip arthroplasty (THA), among young adult patients in their 40s [8].
Depending on injury type, operative options for FNF include in situ fixation, closed or open reduction and internal fixation (CRIF and ORIF), hip hemiarthroplasty (HHA), and THA [1]. Due to concerns with functional outcomes and implant longevity, HHA and THA are typically avoided as first-line operations in young patients, and the consensus favors internal fixation, which salvages the femoral head [9, 10]. However, femoral head-preserving surgeries come with complications (such as nonunion, malunion, avascular necrosis, surgical site infection, and implant failure) affecting 5%–20% of patients and necessitating revision or conversion to hip replacement [11].
For young adult patients with risk factors for poor bone quality or failed fixation, hip arthroplasty may be performed: (1) THA may be considered depending on pre-morbid mobility and cognitive status; (2) Bipolar HHA may be preferable to THA if such patients have alcohol abuse because HHA might minimize the risk of dislocation associated with alcohol withdrawal or postsurgical intoxication [12]. Recently, more literature has reported the use of hip arthroplasty as first-line operation in patients under the age of 50 [8].
Unlike most existing studies focusing on hip arthroplasty for FNF in older populations, substantial gaps exist in the current knowledge of clinical outcomes of the few young adult patients with FNF who undergo hip arthroplasty as initial surgical treatment. This dearth of information may hinder clinical decision-making and resource allocation [13]. Thus, based on the most current data available in the National Inpatient Sample (NIS), we aim to determine if there is a difference between HHA and THA for young patients FNFs with regard to postoperative LOS (pLOS), prosthesis-related complications (PRCs), and total charges incurred.
2. Methods
2.1. Study Design and Study Population
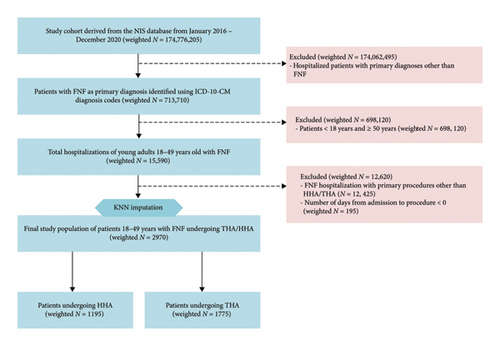
This is a Level of Evidence III retrospective observational study involving adult patients in the U.S. who underwent hip arthroplasty following a FNF between 2016 and 2020. Patients aged < 18 years or ≥ 50 years, as well as those who underwent other procedures for their FNF (e.g., internal fixation), were excluded. Patients with number of days from admission to primary procedure recorded as values < 0 were also excluded.
2.2. Study Outcomes and Endpoints
pLOS was defined as the number of days from the hip arthroplasty procedure to hospital discharge. pLOS was analyzed as a continuous variable and modeled to estimate the relative change in mean pLOS by procedure type.
PRCs, including mechanical loosening (ML), prosthesis dislocation (PD), periprosthetic fracture (PPF), and aggregate PRC, were defined as binary (yes/no) outcomes. The 10th Revision International Classification of Diseases, Clinical Modification (ICD-10-CM) codes were used to identify PRCs (Table A4) [14]. The aggregate PRC indicator signified the presence of at least one PRC in a patient. Adjusted odds ratios (aOR) of developing specific PRCs by procedure type were estimated.
Adjusted total charges was defined as the total financial cost (in U.S. dollars) billed for the index hospitalization. Consumer Price Indexes (CPIs) were used to adjust charges in prior years (2016–2019) for inflation and converted to 2020 U.S. dollars [15]. Adjusted total charges was analyzed as a continuous variable and modeled to estimate the relative difference in adjusted mean hospital costs by procedure type.
2.3. Comparison Groups and Comorbidities
ICD-10-CM codes were used to identify young adult patients admitted with FNF as a primary diagnosis (Table A1) [14]. The ICD-10, Procedure Coding System (ICD-10-PCS) codes were used to identify patients with FNFs undergoing HHA or THA as a primary procedure (Table A2) [16]. ICD-10-CM codes were also used to identify comorbidities or coexisting conditions of osteoporosis, obesity, diabetes mellitus (DM) with or without complications, hypertension (HTN), venous thromboembolism (VTE), tobacco use/nicotine dependence, alcohol abuse/dependence, and drug abuse/dependence (Table A3) [14].
2.4. Source and Details of Data
Data was obtained from the NIS, a deidentified administrative database in the Agency for Healthcare Research and Quality (AHRQ)-funded Healthcare Cost and Utilization Project (HCUP). The NIS is the largest openly accessible inpatient care database in the U.S., containing discharge-level data provided by 49 statewide data organizations [48 States plus the District of Columbia (D.C.)] participating in the HCUP [17].
The NIS dataset includes a stratified sample of 20% of discharges from all HCUP-participating hospitals, totaling seven million annual hospitalizations, approximating 35 million hospitalizations between 2016 and 2020, and 175 million when discharge weights are applied. This data estimates the coverage of 97% of discharges from nonfederal U.S. hospitals, encompassing 98% of the U.S. population [17].
The NIS was updated in 2015 to follow ICD-10-CM criteria. Each hospitalization is considered a distinct entry within the database, containing one principal diagnosis, a maximum of 39 secondary diagnoses, and 25 procedural diagnoses related to hospital admission. We employed discharge-level weights to aid in projecting national estimates alongside the requisite information for estimating variances [17].
2.5. Statistical Methods
We used IBM SPSS Statistics (Version 29) for all analyses, except for missing data imputation, which was performed using R statistical software (Version 4.3.2) [18].
The dataset met the missing completely at random (MCAR) assumptions for the variables age, race, median household income, pLOS, number of days from admission to the procedure, total charges, and primary expected Payer. However, to reduce the number of case-wise deletions during analysis and preserve statistical power, we utilized k-nearest neighbor imputation (k-NNI) to impute missing data. The k-value of 25 was determined by calculating the unweighted sample size square root and rounding to the nearest whole number [19, 20].
Frequencies and percentages for demographic, clinical, and hospital characteristics were calculated for each procedure group and tested for significant differences using independent t-tests, median tests and chi-square (χ2) tests. Trends of hip arthroplasty across procedure groups, as well as 5-year incidence of PRCs, were also assessed.
Weighted generalized linear models (GLM) were used to estimate the relative change in mean pLOS and adjusted mean total charges associated with each procedure type. The Poisson log-linear model was used for mean pLOS, and gamma with log link model was used for adjusted mean total charges [21]. Using multivariable logistic regression, the aOR were used to evaluate the association between procedure type and the respective PRCs. Demographic, clinical, and hospital characteristics that showed a significant association with procedure type were included in multivariable models as controlling variables.
Statistical significance for all tests utilized a two-sided approach, with values of p ≤ 0.05 deemed statistically significant.
2.6. Ethical Considerations
Neither Institutional Review Board (IRB) endorsement nor Informed consent was necessary. HCUP Data Use Agreements (DUAs) and relevant ethical oversight were in place for all researchers [17].
3. Results
Among 174,776,205 patient records in the NIS from 2016 to 2020, FNF was the primary diagnosis in 15,590 young adults, representing 2.18% of all FNFs. Of these, 2970 patients (19.05%) underwent hip arthroplasty. Within the hip arthroplasty cohort, 1195 (40.2%) underwent HHA, and 1175 (59.8%) underwent THA (Figure 1).
3.1. Demographic, Clinical, and Hospital Characteristics
The age distributions were comparable between the HHA and THA groups, with median ages of 46 years and 45 years, respectively. Patients undergoing HHA were more likely to be covered by Medicare, while those in the THA group predominantly had private insurance. In both groups, majority of patients were White, and admissions were primarily nonelective (Table 1).
| Variables | HHA N = 1195 (40.2%) | THA N = 1775 (59.8%) | Total N = 2970 (100%) | p value |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age | ||||
| Mean age† | 42.96 (6.34) | 43.18 (5.98) | 43.09 (6.129) | 0.026 |
| Median age ∗ | 46.0 (40.0–48.0) | 45.0 (41.0–48.0) | 45.0 (40.0–48.0) | 0.586 |
| Age groups (%) | 0.015 | |||
| Age group 18–29 years | 75 (6.3) | 70 (3.9) | 145 (4.9) | |
| Age group 30–39 years | 200 (16.7) | 305 (17.2) | 505 (17.0) | |
| Age group 40–49 years | 920 (77.0) | 1400 (78.9) | 2320 (78.1) | |
| Sex (%) | 0.102 | |||
| Male | 620 (51.9) | 975 (54.9) | 1595 (53.7) | |
| Female | 575 (48.1) | 800 (45.1) | 1375 (46.3) | |
| Race (%) | < 0.001 | |||
| White | 895 (74.9) | 1430 (80.6) | 2325 (78.3) | |
| Black | 140 (11.7) | 135 (7.6) | 275 (9.3) | |
| Hispanic | 100 (8.4) | 110 (6.2) | 210 (7.1) | |
| Asian or pacific islander | 15 (1.3) | 40 (2.3) | 55 (1.9) | |
| Native american | 20 (1.7) | 10 (0.6) | 30 (1.0) | |
| Other | 25 (2.1) | 50 (2.8) | 75 (2.5) | |
| Median household income for patient’s ZIP code (%) | 0.138 | |||
| 0–25th percentile | 375 (31.4) | 525 (29.6) | 900 (30.3) | |
| 26th to 50th percentile (median) | 340 (28.5) | 470 (26.5) | 810 (27.3) | |
| 51st to 75th percentile | 305 (25.5) | 470 (26.5) | 775 (26.1) | |
| 76th to 100th percentile | 175 (14.6) | 310 (17.5) | 485 (16.3) | |
| Patient level and admission (clinical) characteristics | ||||
| Primary payer (%) | < 0.001 | |||
| Medicare | 465 (38.9) | 330 (18.6) | 795 (26.8) | |
| Medicaid | 355 (29.7) | 390 (22.0) | 745 (25.1) | |
| Private insurance | 240 (20.1) | 725 (40.8) | 965 (32.5) | |
| Self-pay | 230 (6.3) | 370 (8.2) | 600 (7.4) | |
| No charge | 80 (6.7) | 165 (9.3) | 245 (8.2) | |
| Other | 45 (3.8) | 145 (8.2) | 190 (6.4) | |
| Admission type (%) | < 0.001 | |||
| Nonelective | 1125 (94.1) | 1555 (87.6) | 2680 (90.2) | |
| Elective | 70 (5.9) | 220 (12.4) | 290 (9.8) | |
| Admission day (%) | 0.486 | |||
| Weekday | 875 (73.2) | 1320 (74.4) | 2195 (73.9) | |
| Weekend | 320 (26.8) | 455 (25.6) | 775 (26.1) | |
| Comorbidities/coexisting conditions (%) | ||||
| Osteoporosis | 95 (7.9) | 110 (6.2) | 205 (6.9) | 0.065 |
| Obesity | 90 (7.5) | 210 (11.8) | 300 (10.1) | < 0.001 |
| DM | 255 (21.3) | 235 (13.2) | 490 (16.5) | < 0.001 |
| HTN | 550 (46.0) | 545 (30.7) | 1095 (36.9) | < 0.001 |
| VTE | 40 (3.3) | 20 (1.1) | 60 (2.0) | < 0.001 |
| Abuse/dependence of alcohol | 200 (16.7) | 200 (11.3) | 400 (13.5) | < 0.001 |
| Abuse/dependence of drug | 510 (42.7) | 625 (35.2) | 1135 (38.2) | < 0.001 |
| Tobacco use/nicotine dependence | 470 (39.3) | 625 (35.2) | 1095 (36.9) | 0.023 |
| Days from admission to procedure | ||||
| Mean days from admission to procedure⋄ | 1.51 (1.69) | 1.15 (1.20) | 1.30 (1.43) | < 0.001 |
| Median days from admission to procedure♦ | 1.0 (1.0–2.0) | 1.0 (0.0–2.0) | 1.0 (1.0–2.0) | < 0.001 |
- Note: Percentages in brackets are column percentages. Percentages indicates direct comparison between HHA and THA amongst patients with FNF from year 2016–2020.
- Abbreviations: DM = diabetes mellitus, HHA = hip hemiarthroplasty, HTN = hypertension, THA = total hip arthroplasty, VTE = venous thromboembolism.
- †Expressed in mean ± SD years. Distribution is left-skewed (skewness value: −1.354).
- ∗Expressed in median years with the interquartile range (IQR) in parentheses.
- ⋄Expressed in mean ± SD days. Distribution is right-skewed (skewness value = 3.102).
- ♦Expressed in median days with the IQR in parentheses.
Patients undergoing THA were more likely to be obese, whereas those in the HHA group had higher rates of DM, HTN, VTE, and substance abuse or dependence (of alcohol, drugs, and tobacco). HTN and drug abuse/dependence were the most prevalent comorbidities in the HHA cohort, whereas tobacco abuse/dependence and drug abuse/dependence were the most common comorbidities in the THA group. The median number of days from hospital admission to procedure was one day in both groups but mean time to procedure was shorter for THA patients than HHA patients (Table 1).
The choice of hip arthroplasty was not affected by sex, median household income, day of admission, or osteoporosis status (Table 1).
For both procedure groups, surgery was more likely to be performed in private nonprofit, urban teaching hospitals (Table 2).
| Variables | HHA N = 1195 (40.2%) | THA N = 1775 (59.8%) | Total N = 2970 (100%) | p value |
|---|---|---|---|---|
| Hospital level characteristics | ||||
| Bed size of hospital (%) | 0.467 | |||
| Small | 205 (17.2) | 335 (18.9) | 540 (18.2) | |
| Medium | 350 (29.3) | 500 (28.2) | 850 (28.6) | |
| Large | 640 (53.6) | 940 (53.0) | 1580 (53.2) | |
| Hospital location/teaching status (%) | < 0.001 | |||
| Rural | 160 (13.4) | 145 (8.2) | 305 (10.3) | |
| Urban nonteaching | 310 (25.9) | 375 (21.1) | 685 (23.1) | |
| Urban teaching | 725 (60.7) | 1255 (70.7) | 1980 (66.7) | |
| Hospital region | 0.122 | |||
| Northeast | 135 (11.3) | 245 (13.8) | 380 (12.8) | |
| Midwest | 250 (20.9) | 395 (22.3) | 645 (21.7) | |
| South | 555 (46.4) | 770 (43.4) | 1325 (44.6) | |
| West | 255 (21.3) | 365 (20.6) | 620 (20.9) | |
| Control/ownership of hospital (%) | 0.015 | |||
| Government, nonfederal | 180 (15.1) | 205 (11.5) | 385 (13.0) | |
| Private, nonprofit | 840 (70.3) | 1280 (72.1) | 2120 (71.4) | |
| Private, invest-own | 175 (14.6) | 290 (16.3) | 465 (15.7) |
- Note: Percentages in brackets are column percentages. Percentages indicates direct comparison between HHA and THA amongst patients with FNF from year 2016–2020.
- Abbreviations: HHA = hip hemiarthroplasty, THA = total hip arthroplasty.
The choice of hip arthroplasty was not affected by the bed size or geographic region of the hospital (Table 2).
3.2. Hip Arthroplasty Trends
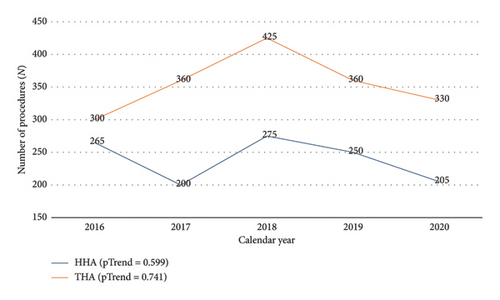
There was no significant linear trend in the number of HHA or THA procedures performed between 2016 and 2020 (Figure 2).
3.3. In-Hospital Outcomes by Procedure Groups
3.3.1. Unadjusted Comparisons
The mean pLOS for patients undergoing HHA was 5.26 days, and the median pLOS was 4 days. Patients who underwent THA had a mean pLOS of 3.66 days and a median pLOS of 2 days (Table 3).
| In-hospital outcome | HHA N = 1195 (40.2%) | THA N = 1775 (59.8%) | Total N = 2970 (100%) | p value |
|---|---|---|---|---|
| Mean pLOS (days)† | 5.26 (5.99) | 3.66 (4.55) | 4.30 (5.24) | < 0.001 |
| Median pLOS (days) ∗ | 4.0 (3.0–6.0) | 2.0 (2.0–4.0) | 3.0 (2.0–5.0) | < 0.001 |
| PRC | ||||
| -ML | 10 (0.8%) | 10 (0.6%) | 20 (0.7%) | 0.372 |
| -PD | 5 (0.4%) | 20 (1.1%) | 25 (0.8%) | 0.038 |
| -PPF | 35 (2.9%) | 20 (1.1%) | 55 (1.9%) | < 0.001 |
| -Aggregate PRC | 35 (2.9%) | 50 (2.8%) | 85 (2.9%) | 0.858 |
| Mean adj. total charges ($)⋄ | 100,110.64 (72,873.48) | 100,285.81 (69,404.55) | 100,215.33 (70,808.63) | 0.007 |
| Median adj. total charges ($)♦ | 86,225.84 (58,904.00–114,145.27) | 75,617.84 (57,296.06–116,572.98) | 80,494.95 (58,374.00–114,791.00) | < 0.001 |
- Note: Percentages in brackets are column percentages. Percentages indicates direct comparison between HHA and THA amongst patients with FNF from year 2016–2020.
- Abbreviations: HHA = hip hemiarthroplasty, ML = mechanical loosening, PD = prosthesis dislocation, PPF = periprosthetic fracture, PRC = prosthesis-related complication, THA = total hip arthroplasty.
- †Expressed in mean ± SD days. Distribution is right-skewed (skewness value = 6.551).
- ∗Expressed in median days with the IQR in parentheses.
- ⋄Expressed in mean ± SD U.S. Dollars. Distribution is right-skewed (skewness value = 2.810).
- ♦Expressed in median U.S. Dollars with the IQR in parentheses.
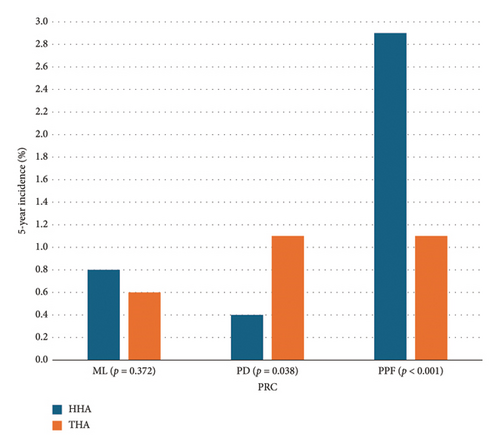
PPF was the most common PRC following HHA, while PPF and PD were equally prevalent after THA. ML was the second most common PRC in patients who underwent HHA. More patients in the THA group developed PD than patients who had HHA, while patients who underwent HHA developed PPF at a higher rate than patients who had THA. There was no statistically significant difference in the 5-year incidence of ML among both groups (Table 3) (Figure 3).
Mean adjusted total charges incurred for HHA patients were lower than THA by $175.17. However, the median adjusted total charges incurred for HHA patients was higher than THA by $10,608 (Table 3).
3.3.2. Adjusted Comparisons
Controlling for demographic, clinical, and hospital characteristics, multivariable GLM Poisson log-linear analysis revealed a significant relationship between procedure type and pLOS, with patients in the HHA group experiencing a 22.4% longer pLOS compared to those in the THA group (Table 4).
| In-hospital outcome | HHA N = 1195 (40.2%) | THA N = 1775 (59.8%) | p-value |
|---|---|---|---|
| Mean pLOS [exp(B)] | 1.224 (1.183, 1.266) | 1.0 (REF) | < 0.001 |
| PRC (aOR) | |||
| - PD | 1.0 (REF) | 6.00 (1.78, 20.24) | 0.004 |
| - PPF | 9.06 (4.21, 19.48) | 1.0 (REF) | < 0.001 |
| Mean adj. total charges [exp(B)] | 1.0 (REF) | 1.033 (0.995, 1.075) | 0.092 |
- Abbreviations: HHA = hip hemiarthroplasty, PD = prosthesis dislocation, PPF = periprosthetic fracture, PRC (aOR) = prosthesis-related complication, THA = total hip arthroplasty.
Multivariable logistic regression analysis adjusted for demographic, clinical and hospital characteristics, showed a significant association between procedure type and PRC for both PD and PPF. THA was associated with six times higher odds of PD than HHA while, HHA was associated with nine times higher odds of PPF compared to THA (Table 4).
No significant change in adjusted total charges between both procedure groups was observed after GLM with gamma and log link analysis, adjusted for demographic, clinical, and hospital characteristics (Table 4).
4. Discussion
The age range defining a young patient often spans from skeletal maturity to 50 years, though the upper limit varies among surgeons [9]. FNFs pose a significant treatment challenge in this population and while internal fixation has traditionally been the standard treatment for young patients with FNF, emerging data suggests a potential shift in these conventions [8, 13]. To our knowledge, this study is the first to utilize a national administrative database to compare in-hospital outcomes of HHA and THA among young adult patients in the U.S.
Our observation of a one-in-five rate of hip arthroplasty in young adults with FNFs represents a fivefold increase compared to prior estimates by Johnson et al., who surveyed orthopedic surgeons primarily in North America and Europe [8]. Similarly, Johnson et al. reported a fourfold increase (from 5.3% to 22.3%) in the use of THA between 2002 and 2014 [8], and Maman et al. documented a 19% THA rate among patients aged 35–44.9, a subset of our study population [13]. This rising use of THA likely reflects the durability of total hip implants as well as risks of avascular necrosis and hardware failures with internal fixation [8]. Our study uniquely identifies a higher-than-expected use of HHA, likely driven by the higher prevalence of comorbidities as well as alcohol abuse or dependence, which affected one out of every six patients in this cohort [12].
Our adjusted models demonstrated significantly higher pLOS among patients who underwent HHA compared to THA. Prior studies on pLOS for FNFs, largely focused on older populations, have shown mixed results [22–24]. Voskuji et al. observed a higher pLOS risk among hip arthroplasty patients with medical comorbidities, despite comparable pLOS between HHA and THA [24]. In our study, HHA patients had more comorbidities than THA patients, which may explain their longer pLOS.
PPF was the most common PRC overall, with patients in the HHA group having a significantly higher adjusted risk of PPF than patients in the THA group. This mirrors findings in previous literature where osteoporosis and wide femoral canals were identified as significant contributors to PPFs in patients who underwent HHA [25]. The relatively low incidence of PD in our study compared to previous studies was unexpected [26]; however, the higher adjusted odds of developing PD after undergoing THA than HHA was consistent with previous studies [26]. Surgical approach is known to influence hip stability, and the anterolateral approach is often recommended given the higher dislocation rates of the posterior approach [27].
Total charges recorded in the NIS vary from patient to patient but typically include charges for hospital rooms, supplies, medications, laboratory fees, and care staff (such as nurses). Total charges may include emergency charges prior to hospital admission but typically exclude professional fees (such as those for doctors) and noncovered expenses [17]. After adjusting for patient and hospital factors, we found no significant change in the adjusted total hospital charges between the procedure groups. In contrast, Slover et al. revealed that HHA patients, on average, had significantly lower costs than THA patients ($57,034 vs. $72,840) [28]. Other studies suggest that beyond the immediate post-op period, HHA may incur higher long-term costs than THA due to treatments for failed HHA or conversion surgeries [29, 30].
This study has several limitations. First, as a retrospective analysis of hospital admission data, it is restricted to inpatient events, making it difficult to assess the duration of FNF symptoms before presentation or long-term postsurgical outcomes. Second, the dataset lacks operative details such as anesthesia type, surgical duration, or blood loss, which are important considerations in surgical research [31]. Third, the small sample size of some PRCs resulted in a quasi-complete separation between PRCs and certain independent variables. To address this, we collapsed problematic variable levels for improved model stability [32].
5. Conclusion
In young adults with FNFs undergoing hip arthroplasty, HHA is associated with a longer pLOS and a higher risk of PPF, while THA is linked to a higher risk of PD. The costs between the two procedures are comparable. When hip arthroplasty is indicated, whether as a primary intervention or a revision after failed internal fixation, patient-specific factors should guide the choice of procedure to optimize outcomes. Further research is needed to clarify the benefits and risks of hip arthroplasty as its use continues to grow in this population.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
Hembashima Gabriel Sambe contributed to the study concept, design, data acquisition, analysis, and manuscript drafting, revision, and submission. Urvish Patel refined the study design and data analysis and provided careful revisions to the final manuscript. All authors read and approved the final submitted manuscript.
Funding
The authors received no financial support from any third party, institution, organization, or company for the research, authorship, or publication of this article.
Appendix A: ICD-10-CM and ICD-10-PCS Codes Utilized in the Study
| Right | Left | Unspecified |
|---|---|---|
| S72001A | S72002A | S72009A |
| S72001B | S72002B | S72009B |
| S72001C | S72002C | S72009C |
| S72011A | S72012A | S72019A |
| S72011B | S72012B | S72019B |
| S72011C | S72012C | S72019C |
| S72031A | S72032A | S72033A |
| S72031B | S72032B | S72033B |
| S72031C | S72032C | S72033C |
| S72034A | S72035A | S72036A |
| S72034B | S72035B | S72036B |
| S72034C | S72035C | S72036C |
| S72041A | S72042A | S72043A |
| S72041B | S72042B | S72043B |
| S72041C | S72042C | S72043C |
| S72044A | S72045A | S72046A |
| S72044B | S72045B | S72046B |
| S72044C | S72045C | S72046C |
- Note: ICD-10-CM = 10th revision of the international classification of diseases, clinical modification.
| HHA | THA | ||
|---|---|---|---|
| Right | Left | Right | Left |
| 0SRR019 | 0SRS019 | 0SR9019 | 0SRB019 |
| 0SRR01A | 0SRS01A | 0SR901A | 0SRB01A |
| 0SRR01Z | 0SRS01Z | 0SR901Z | 0SRB01Z |
| 0SRR039 | 0SRS039 | 0SR9029 | 0SRB029 |
| 0SRR03A | 0SRS03A | 0SR902A | 0SRB02A |
| 0SRR03Z | 0SRS03Z | 0SR902Z | 0SRB02Z |
| 0SRR07Z | 0SRS07Z | 0SR9039 | 0SRB039 |
| 0SR903A | 0SRB03A | ||
| 0SR903Z | 0SRB03Z | ||
| 0SRR0J9 | 0SRS0J9 | 0SR9049 | 0SRB049 |
| 0SRR0JA | 0SRS0JA | 0SR904A | 0SRB04A |
| 0SRR0JZ | 0SRS0JZ | 0SR904Z | 0SRB04Z |
| 0SRR0KZ | 0SRS0KZ | 0SR9069 | 0SRB069 |
| 0SR906A | 0SRB06A | ||
| 0SR906Z | 0SRB06Z | ||
| 0SR907Z | 0SRB07Z | ||
| 0SR90EZ | 0SRB0EZ | ||
| 0SR90J9 | 0SRB0J9 | ||
| 0SR90JA | 0SRB0JA | ||
| 0SR90JZ | 0SRB0JZ | ||
| 0SR90KZ | 0SRB0KZ | ||
- Note: ICD-10-PCS = 10th revision of the international classification of diseases, procedure coding system.
- Abbreviations: HHA = hip hemiarthroplasty, THA = total hip arthroplasty.
| Comorbidity | ICD-10 CM code |
|---|---|
| Osteoporosis | M80, M81 |
| Obesity | E660, E661, E662, E663, E668, E669 |
| DM with/without complications | E08, E09, E10, E11, E13 |
| HTN | I10, I11, I12, I13, I15, I16, I1A |
| VTE | I82, I26 |
| Abuse/dependence of alcohol | F101, F102 |
| Abuse/dependence of drug | F11, F12, F13, F14, F15, F16, F17, F18, F19 |
| Tobacco use/nicotine dependence | Z720, F172, O9933 |
- Note: ICD-10-CM = 10th revision of the international classification of diseases, clinical modification.
- Abbreviations: DM = diabetes mellitus, HTN = hypertension, VTE = venous thromboembolism.
| Right | Left | |
|---|---|---|
| Mechanical loosening (ML) | T84030A | T84031A |
| T84030D | T84031D | |
| T84030S | T84031S | |
| Dislocation of prosthesis (PD) | T84020A | T84021A |
| T84020D | T84021D | |
| T84020S | T84021S | |
| Periprosthetic fracture (PPF) | M9701XA | M9702XA |
| M9701XD | M9702XD | |
| M9701XS | M9702XS | |
- Note: ICD-10-CM: 10th revision of the international classification of diseases, clinical modification.
Open Research
Data Availability Statement
The data supporting the findings of this study are available on Zenodo, a publicly available database, at https://doi.org/10.5281/zenodo.14523498.