Carbohydrates Intake vs. Fats Intake Correlate With Blood Pressure in Adolescents: A Systematic Review
Abstract
Teenagers are experiencing a shift in their eating habits toward fast food, which is high in unhealthy fats and carbohydrates and correlates with an increased risk of obesity and hypertension due to its high-calorie density, large portion sizes, and accessibility. This systematic review compares the evidence on the carbohydrate and fat intakes toward adolescent hypertension. This evidence-based analysis is based on the Preferred Reporting Item for Systematic Review and Meta-Analysis (PRISMA) 2020 statement. The data were processed qualitatively to assess the risk of bias using the Newcastle–Ottawa Scale (NOS) and Agency for Health Research and Quality (AHRQ) standards as the threshold. This review was registered in PROSPERO with the registration number CRD42024599534. Published studies up to March 2024 sourced from PubMed Central, Springer Link, EBSCO Host, ScienceDirect, and Google Scholar were used as databases in this study. Nine studies were included in this systematic review. Eight studies (88.9%) showed a relation between carbohydrates and fat intake toward adolescent hypertension. From six studies that mainly discussed comparing carbohydrates and fat intake and the risk of hypertension in adolescents, three out of six studies agreed that the risk of hypertension is more closely associated with higher fat intake than with carbohydrate intake. In summary, both excessive carbohydrate and fat intake are related to the development of hypertension in adolescents, but higher fat intake might show more outcomes in developing hypertension. This study is expected to be a theoretical foundation for future research.
1. Introduction
Nowadays, teenagers are experiencing a shift in their eating habits toward fast food, which is high in unhealthy fats and carbohydrates. Fast food is common and positively correlated with an increased risk of obesity and hypertension due to its high-calorie density, large portion sizes, and accessibility. The prevalence of obesity has risen sharply globally, making it one of the most pressing public health problems of the twenty-first century [1, 2]. Adolescents who experience high blood pressure (BP) are likely to experience high BP in adulthood. A longer treatment cycle, more difficult BP control, and a worse prognosis have all been linked to earlier onset of hypertension, according to prior research. Adolescent hypertension is commonly known as “the silent killer” as most of its sufferers do not always show the usual signs [3, 4]. Through the last two decades, there has been a widespread trend of rising childhood hypertension prevalence, with an overall increase rate from 75% to 79% (from 2000 to 2015). The prevalence of hypertension ranged from 4.32% in children aged 6 years (95% confidence interval [CI], 2.79%−6.63%) to 3.28% in children aged 19 years (95% CI, 2.25%−4.77%) [5].
American Academy of Pediatrics (AAP) guidelines set the threshold—which is for BP ≥ 95th percentile or >120/80 mmHg at age 6–11 or >130/85 mmHg at age ≥12—and in the case of BP screening [6]. Multifactorial factors, including obesity, high-sodium intake, sedentary lifestyle, perinatal factors, socioeconomic factors, and ethnicity, are commonly associated with hypertension. An imbalanced diet is one of the variables that contribute to the development of hypertension in adolescents [7]. The right nutrients are necessary for the body to grow, develop mentally, be productive, and maintain itself. Three macronutrient classes are carbohydrates, proteins, and fats, which contain each for 50%, 30%, and 20% of the total calories in a balanced diet, respectively [8].
The correlation between the consumption of carbohydrates in the diet and cardiovascular well-being has garnered significant attention in recent times, whereas exceeding recommended dietary levels of carbohydrates and fats may have an impact on the prevalence of hypertension in adolescents [9]. Excess fat and carbohydrate intake increase the risk of overnutrition and obesity, which is marked by a very high body weight compared to either age or height and induces an increase in blood volume needed to supply oxygen and nutrients to the body tissues, which make heart rate and BP also increases due to this increase in blood volume [8]. Additionally, there is a disruption in blood insulin levels, which leads to renal sodium resistance [10].
This systematic review aims to analyze the role of diet, especially comparing carbohydrates and fat’s role toward BP in adolescents, thus providing new insights into overcoming risk factors and early diagnosis of hypertension in adolescents, considering that the long-term impact of hypertension cannot be treated.
2. Methods
This evidence-based review is based on the Preferred Reporting Item for Systematic Review and Meta-Analysis (PRISMA) 2020 statement [11]. This review was registered in PROSPERO with the registration number CRD42024599534. We detailed participants, exposure, comparison, and outcome (PECO); P: Adolescents respondence with ages 10 until 18 years old (according to Kemenkes RI), E: adolescents with higher carbohydrate intake and fats intake, C: adolescents with normal intake of carbohydrate and fats, and O: higher BP (systolic and diastolic). The authors identified the studies published through title and abstract by March 2024. Electronic databases, including PubMed Central, Springer Link, Medline, ScienceDirect, and Google Scholar, were used. In addition, a list of references for all eligible studies was manually reviewed. We used MeSH terms by combining the words “carbohydrates,” “fats,” and “adolescent hypertension.”
This systematic review study had to meet two following criteria in order to be included, such as (1) observational studies investigating the association between carbohydrates, fats intake, and hypertension, including case–control, cross-sectional, and cohort studies; (2) research on adolescents with aged from 10 to 18 years old. We excluded (1) subjects with other associated diseases, other associated lifestyle factors such as physical activity, sleep patterns, or socioeconomic status, and other macro- or micronutrient intake-related conditions; (2) comments, review articles, letters, editorial comments, conference abstracts, articles not in 10 years to reach the latest updates of the journals and previous systematic review and meta-analysis; (3) any gray literature or faculty journals that did not appear in our search engines.
All authors screened titles and abstracts for the initial study selection and obtained the full text of potentially eligible studies to confirm if they met our inclusion criteria. Data extraction is independently completed by all researchers from the confirmed articles and collected in an Excel spreadsheet. Any differences are resolved together to make a final decision. After the included studies were examined, the data extracted were the first author, place, publication year, study design, participant’s demographic (including number of population), and discussion between carbohydrates, fats, and adolescent hypertension. Each piece of data in the study is reported in full and discussed based on the results of each study, concluding the relative risk (RR), odds ratio (OR), hazard ratio (HR), mean and standard deviation (SD) of systolic or diastolic BP, or p value which determines whether the study states the relationship is significant or not.
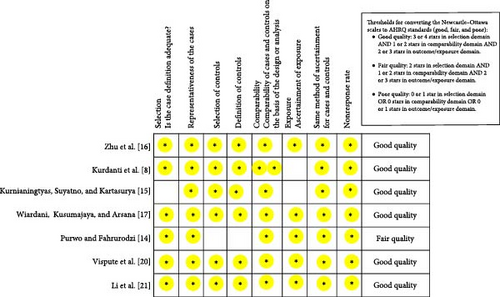
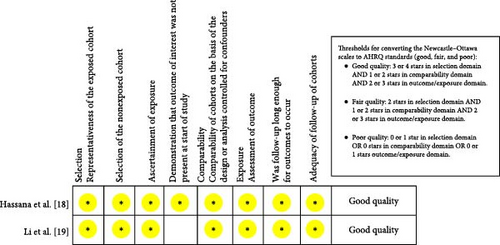
The risk of bias in included studies was assessed by using the Newcastle–Ottawa Scale (NOS). For case–control and cross-sectional studies, we examined the following eight domains: adequacy of case definition, representativeness of cases, selection of controls, definitions of controls, comparability of cases and controls, ascertainment of exposure, the same method of ascertainment for cases and controls, and nonresponse rate. For cohort studies, we evaluated the following eight domains: representativeness of exposed cohort, selection of nonexposed cohort, ascertainment of exposure, absence of outcome of interest at the start of the study, comparability of cohorts, assessment of outcome, follow-up duration, and adequacy of follow-up of cohorts [12]. We use Agency for Health Research and Quality (AHRQ) standards as a threshold to define the quality of the studies [13].
3. Result
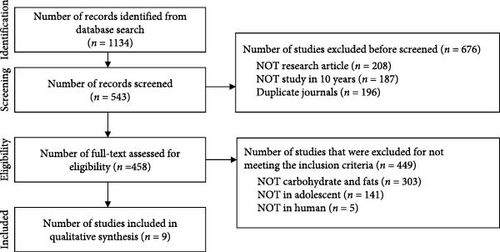
Following all MeSH words that we used, our search strategy turned up a total of 1134 possibly pertinent studies. After the removal of duplicates (n = 196), studies over a 10-year period (n = 187), and not article journals (n = 208), 543 (47.88%) studies were screened based on title and abstract, full-text analysis, and inclusion criteria, as the results according to PRISMA 2020 are shown in Figure 1.
Nine studies with a total population of 142,487 children and adolescents aged from 5 to 18 years old were drawn from the majority of Asian populations, namely China, Indonesia, Egypt, and India, as well as research on Asians conducted in America. Included subjects were considered healthy with an overall 3-day diet diary for nutritional data collection and BP measurements, while students with health problems, such as psychological problems or any other disease, as well as students on medication that might affect their BP, were excluded from the final analysis. In this study, pairwise matching was carried out between the case group and the control group based on age, gender, and school origin or peer group.
From a total of nine studies that were included in qualitative synthesis, all of the studies have good quality, based on utilizing NOS and AHRQ. However, a study by Purwo et al. was rated as having only moderately good quality because it fulfilled only two of the four requirements in the selection domain, specifically due to the lack of details regarding the selection and definition of control subjects [14]. The research conducted by Kurdanti et al. [8] and Kurnianingtyas et al. [15] included follow-up data collection over 3 days, and the results were broadly categorized into obesity and nonobesity groups to explore their association with the risk of hypertension in adolescents. The study by Kurnianingtyas et al. also did not clearly outline the criteria for selecting respondents, leading to insufficient rigor in the selection process and an increased risk of biased criteria exposure.
The overall results of the study quality assessment in the form of a visual star of every domain are shown in Figures 2 and 3. However, the heterogeneity across the variables between the intake of carbohydrates and fats that were discussed in every included journal made a meta-analysis impractical.
A total of nine articles met all inclusion criteria [8, 14–21]. Five studies were case–control studies, two were cross-sectional studies, and two were cohort studies with a prospective study design. Table 1 lists the characteristics of the studies, and a total of nine studies are included in this systematic review that discuss both carbohydrates and fats.
| Authors, country (year) | Study design | Subjects | Macronutrient | Conclusion |
|---|---|---|---|---|
| Zhu et al. [16], China (2014) | Case–control | 672 Chinese Han students (average age of population: 16.85 years old) | Carbohydrates, fats |
|
| Kurdanti et al. [8], Indonesia (2015) | Case–control |
|
Carbohydrates, fats |
|
| Kurnianingtyas, Suyatno, and Kartasurya [15], Indonesia (2017) | Case–control | 70 students at Semarang City High School (aged 15–18 years old) | Carbohydrates, fats | The risk of hypertension is more closely associated with higher fat intake than with carbohydrate intake (high-carbohydrate intake [OR = 1.000; 95% CI = 0.13–7.53; p = 1.000] and high fat intake [OR = 1.133; 95% CI = 0.43–3.01; p = 0.803]). |
| Wiardani, Kusumajaya, and Arsana, [17], Indonesia (2018) | Cross-sectional | 109 students (aged 15–18 years old) | Carbohydrates, fats |
|
| Purwo and Fahrurodzi [14], Indonesia (2018) | Cross-sectional | 30,133 students over 15 years old | Fats | There is a relation between cholesterol levels and the risk of hypertension (OR = 4.450, CI 95%, 3329–5984, p value: 0.000). Patients who have high cholesterol levels have a 4450 times chance of developing hypertension. |
| Hassana et al. [18], Egypt (2019) | Prospective Cohort study | 159 students (82 children and 77 adolescents) |
|
|
| Li et al. [19], China (2021) | Prospective Cohort study | 95,157 students | Carbohydrates |
|
| Vispute et al. [20], India (2022) | Case–control | 2713 students aged 9–18 years old (rural = 1818; urban = 895) |
|
Rural children are in danger of having primary hypertension (18% vs. 10%), especially those who consume a lot of junk food, which contains higher fat and carbohydrates’ intake. |
| Li et al. [21], United States (2023) | Case–control | 13,330 adolescents (11,614 were nonhypertensive and 1716 were hypertensive) | Fats | An increased intake of omega-3 (OR = 0.82, 95% CI: 0.72–0.93, p = 0.002) and omega-6 (OR = 0.86, 95% CI: 0.75–0.98, p = 0.025) PUFAs, octadecatrienoic acid (OR = 0.82, 95% CI: 0.72–0.93, p = 0.003), and octadecadienoic acid (OR = 0.86, 95% CI: 0.75–0.98, p = 0.025) was associated with significantly lower odds of hypertension, and individuals with higher omega-6/omega-3 ratio had significantly higher odds of hypertension (OR = 1.09, 95% CI: 1.02–1.17, p = 0.025). The risk of hypertension is more closely associated with higher fat intake with omega-6/omega-3 ratio. |
- Abbreviations: CI, confidence interval; OR, odds ratio; PUFA, polyunsaturated fatty acid; SD, standard deviation.
Seven out of nine studies discussed about the relation between carbohydrates. Seven out of nine studies discussed the relationship between carbohydrate intake and BP in adolescents [8, 14–18, 20, 21]. All of them showed that there was a relationship between carbohydrate intake and the incidence of hypertension. Eight studies discussed the relationship between fat intake and BP in adolescents [8, 14–18, 20, 21], and seven of them showed that there was a relationship between fat intake and the incidence of hypertension fat intake [8, 14–18, 20].
However, one other research by Li et al. [21] stated contradictory results that show that high fat intake is not a risk factor for hypertension. Six studies discussed comparing carbohydrates and fat intake and the risk of hypertension in adolescents, and three of them (50%) agreed that the risk of hypertension is more closely associated with higher fat intake than with carbohydrate intake [15–17].
4. Discussion
Prior to our knowledge, this is the first systematic review discussing the possible relation between carbohydrate and fat intakes and hypertension, specifically in adolescents. Nine studies are included in this systematic review. Eight studies (88.9%) showed a relationship between carbohydrates and fat intake and adolescent hypertension. From six studies that especially discussed comparing carbohydrates and fat intake and the risk of hypertension in adolescents, three out of six agreed that the risk of hypertension is more closely associated with higher fat intake than with carbohydrate intake [15–17]. This is also in line with the statement of some studies that stated people who have higher fat (cholesterol) intakes have a 4.3 and 4.45 times chance of developing hypertension [14, 17]. Compared to fat intake, one study found that consuming more carbohydrates increased the risk of hypertension by 0.30 times [8]. Two other studies stated that both higher carbohydrate and fat intake are equally significantly related to the risk of hypertension in adolescents.
Generally, consuming excessive amounts of carbohydrates can lower the level of sodium excreted in the urine, which can lead to a buildup of sodium in the blood, elevate BP, and lead to hypertriglyceridemia, which raises the risk of atherosclerosis [22, 23]. At the same time, higher intake of saturated fatty acids is positively correlated with the prevalence of oxidative stress and hypertension, as saturated fat readily accumulates in blood vessels and induces atherosclerosis [24]. Both consumption-induced changes in the equilibrium between the sympathetic and parasympathetic nervous systems are the source of the hyperactivity of the sympathetic nervous system, which is linked to obesity and hypertension. This hyperactivity includes elevated heart rate and BP [25, 26].
The hypothalamic–pituitary–adrenal (HPA) axis changes were the primary biological mechanisms suggested to underlie the causal relationship between BP and carbohydrate consumption. Increased cortisol levels, which result from hyperfunction of the HPA axis, have been linked to weight gain and fat storage, as well as the pathophysiology of psychological disorders and hypertension. On the other hand, diets high in carbohydrates may result in reduced HPA axis stress reactions, which may help to relieve hypertension and psychological dysfunction associated with the HPA axis [27, 28]. This answered the previous statement that stated that the risk of hypertension is more closely associated with higher fat intake than with carbohydrate intake. Therefore, teenagers should be aware of their consumption, preferably low fat, and consume normal carbohydrates according to daily adequacy.
Although the exact etiology of hypertension is still unknown, a number of factors, including increased cardiac output and peripheral resistance, the renin–angiotensin system, and the autonomic nervous system, can contribute to the condition. Constant contraction of the smooth muscle in the arteriolar walls can result in angiotensin-mediated structural alterations and thickening of the blood vessel walls, which raises peripheral resistance irreversibly [26, 29].
Other risk factors that might influence the results include eating habits, such as fast food consumption, gender, genetics, physical inactivity, socioeconomic status, and other macro- and micronutrient intake [8, 14, 15, 17]. Food intake, specifically in carbohydrates and fats, has distinct effects on higher BP in men and women, some of which may be influenced by physiological, pathological, psychological variation or hormonal effects related to estrogen, which can cause BP to rise by lowering their serum angiotensin-converting enzyme (ACE) activity and raising their ACE2 activity [30].
The role of fast food is quite significant in providing an energy contribution of 10%–25% to energy intake. Frequent fast food consumption was linked to oxidative stress, lipid and lipoprotein abnormalities, poor insulin and glucose homeostasis, overweight, and abdominal fat gain. Frequent fast food and out-of-home meal eating ≥1–3 times per week was linked to a 20%–129% increased risk of obesity, and a 56%–162% higher risk of coronary heart disease mortality was also linked to higher fast food consumption and exposure to more readily available, affordable, and high-energy fast food sources. Clinical and experimental investigations have looked into a few of the pathways that might account for the metabolic effects of fast food. Other potential explanations for the cardiometabolic effects of fast food include postprandial unfavorable metabolic diseases, such as lipemia, oxidative stress, and pro-inflammatory processes following a fast food meal, as seen in human research [31, 32].
This study has several limitations because very few studies have been conducted specifically in the adolescent population to compare the risk of hypertension from both carbohydrates and fats. It is also challenging to make conclusions on temporal relationships because the majority of the included research seems to be cross-sectional in characteristics. Overall, the included studies used 3-day food recall evaluations, where information collected using this technique may not accurately represent subjects’ eating habits. There is also methodological heterogeneity across all of the included studies, which makes a meta-analysis unfeasible.
This study is expected to be a theoretical foundation for future research. Future research should aim to draw on larger and more diverse samples to ensure wider applicability. Longitudinal studies would be more effective in determining whether dietary changes precede the development of hypertension in adolescents. Future studies might also look at entire dietary patterns instead of focusing on individual nutrients, as this could offer a more thorough understanding of how food affects hypertension. Outlining other risk factors that might influence the results of hypertension in adolescents, like how education influences dietary decisions or how fast food affects teenage eating habits, and how physical inactivity affects the risk of obesity. This can also help determine the recommended optimum intake and whether it is in accordance with the recommendations.
5. Conclusions
Nine studies included in this systematic review concluded that both carbohydrates and fats are related to adolescent hypertension. Six studies that discussed comparing both carbohydrate and fat intakes showed that three out of six studies stated that the risk of hypertension is more closely associated with higher fat intake than with carbohydrate intake. This study is expected to be a theoretical foundation for future research. However, considering there are still very few studies discussing the relationship on this topic, it is worth further research with more studies.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
No funding was received for this research.
Supporting Information
Additional supporting information can be found online in the Supporting Information section.
Open Research
Data Availability Statement
The authors confirm that the data and materials supporting the findings of this study are available in the article.




