Evaluating the Effectiveness and Safety of Fecal Management Systems among Severely Ill Patients Suffering from Fecal Incontinence: A Retrospective Cohort Study
Abstract
Background. Few large-sample studies have examined the use of fecal management systems (FMSs) in intensive care units (ICUs) or evaluated the associated complications. This study aims to assess the effectiveness and safety of FMS for stool diversion in ICU patients with fecal incontinence (FI). Methods. We enrolled 381 FI patients, assigning them to either an FMS group (n = 134), which used a fecal management device, or a usual care (UC) group (n = 247) that received standard care including regular perianal cleaning. Results. The FMS group reported lower incidence and severity of incontinence-associated dermatitis (IAD) and higher Braden Scale scores (10.42 ± 2.77) compared to the UC group (9.71 ± 2.56), indicating reduced pressure ulcer risk. Notably, FMS-associated complications were minimal, with only 5 patients (3.73%) affected; one required surgical intervention for rectal mucosal bleeding. Conclusions. FMS significantly reduced stool-associated skin irritation, lowered the incidence of IAD and pressure injuries, and improved nurses’ convenience compared to UC.
1. Introduction
FI is defined as the involuntary loss of solid or liquid stool [1]. Reports indicate that the median prevalence of FI in the general population is 7.7%, rising to 46% among elderly residents in institutional settings [1, 2]. FI can lead to the development of IAD and increase the risk of complications, including pressure ulcers and catheter-associated urinary tract infections [3, 4]. Beyond causing physical discomfort and exacerbating psychological distress, FI also escalates treatment costs, burdens nursing staff, and prolongs patient hospitalizations [5–7].
ICU patients are particularly vulnerable to FI and diarrhea due to their critical conditions and the frequent use of antibiotics, enteral feeding, and parenteral nutrition [8]. Patients with diarrhea are prone to IAD because their feces contain higher levels of proteolytic and lipolytic enzymes, which can erode the skin’s protective cuticle after prolonged exposure [9]. Early symptoms of IAD typically include erythema, rash, burning, pain, and severe ulceration. In some cases, erosion, bleeding, and infection may occur [3]. Managing FI and providing fecal care often present complex challenges that are difficult to resolve. Nurses encounter significant difficulties in maintaining patients’ skin integrity and protecting perineal wounds or burns from fecal contamination. Traditional disposable absorbent products like diapers and underwear are inadequate for managing large volumes of semiliquid feces. These products fail to effectively prevent infection spread and avoid perianal skin damage due to prolonged fecal contact [10]. Although zinc oxide barrier cream effectively blocks moisture, it requires reapplication after each incontinence episode [11].
In response to the management challenges of acute FI, FMSs were introduced in the early 21st century. These systems help bedridden patients or those unable to use a bedpan efficiently to evacuate feces [12]. Kowal-Vern et al. reported that the user-friendly nature of FMS/bowel management systems (BMSs) makes them especially suitable for ICUs, burn units, geriatric wards, and emergency hospitals [13]. By utilizing FMS, effective fecal management is achieved, preventing infection spread, protecting wounds, and avoiding fecal contamination. A prospective cohort study by Keshava, Anil et al. demonstrated skin condition improvement following the implementation of a stool management system (P < 0.0001) [14]. Furthermore, Pittman et al. conducted a randomized controlled trial comparing three methods for treating FI: BMS, rectal trumpet, and UC [15]. However, the results showed no statistically significant differences in IAD development and pressure ulcers among the three groups. Interestingly, the UC group reported the lowest IAD scores, contrasting with Keshava et al.’s findings [14]. This discrepancy may be attributed to the small sample size and the daily intensive monitoring of the UC group’s skin condition by experts, who actively participated in developing nursing plans. It is crucial to acknowledge that complications associated with FMS use should not be overlooked. For instance, Kane, William J. et al. assessed rectal complications from FMS use in their retrospective cohort study [16]. Unfortunately, many patients lacked information about the specific FMS types used and the timing of balloon volume adjustments. Currently, large-scale studies are lacking that compare FMS outcomes with routine nursing methods like diaper changes and perianal hygiene in ICU patients with FI, including evaluations of FMS-related complications. Building on the previous research study, this study used a retrospective cohort design with a moderate sample size and comprehensive observation indicators to compare changes in perianal skin conditions, such as IAD and pressure injuries, between patients using FMS and those receiving UC, also assessing the safety of stool diversion using FMS in ICU settings.
2. Patients and Methods
This retrospective analysis was conducted at a single center, adhering to the ethical, moral, and scientific principles of the Declaration of Helsinki. It received approval from the Ethics Committee of Shanghai Fifth People’s Hospital (No. SFPH 2023-124). We obtained written informed consent from the patients to publish their anonymized data in this article.
3. Participants
Sample size and power analysis were conducted using PASS15 software. Assuming a significance level (α) of 0.05 and a power (1 − β) of 0.9, the estimated IAD incidence was 26.1% in the FMS group and 44.7% in the UC group, based on prior studies [17, 18]. Given a group allocation ratio of N2/N1 = 2, the required sample sizes were 97 for the FMS group and 194 for the UC group.
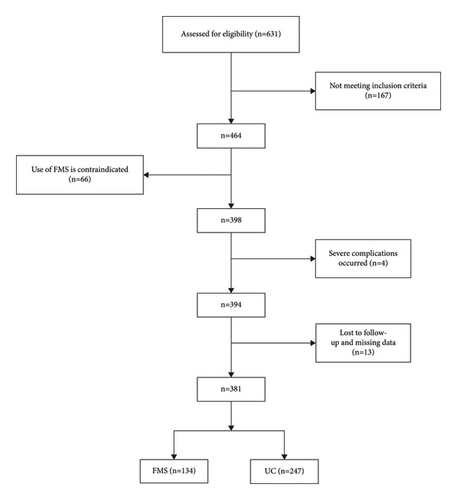
Patients with FI admitted to the general intensive care unit (GICU) and neurocritical intensive care unit (NICU) from January 2020 to March 2023 were selected for this study. The study comprised 134 patients in the FMS group and 247 patients in the UC group (Figure 1).
Inclusion criteria include (1) age ≥18 years; (2) FI of various etiologies or secondary to an indwelling catheter; (3) no existing IAD or pressure ulcers at admission; and (4) voluntary informed consent provided by patients or, for comatose patients, by their families.
Exclusion criteria include (1) history of inflammatory bowel disease or active proctitis; (2) conditions such as rectal prolapse, severe hemorrhoids, anal stenosis, or fistulae; (3) gastrointestinal bleeding; (4) pregnancy or history of uterine prolapse; (5) history of rectal or anal surgery or injury; and (6) known allergies to any product accessories.
4. Procedure
4.1. UC Group
Patients’ defecation was closely monitored, with immediate cleanup of feces. Clothing was changed as needed to ensure cleanliness. Perianal and perineal areas were kept clean and dry, using warm water and sterile paper towels for gentle cleaning.
4.2. FMS Group
4.2.1. FMS Group Equipment
The adult Fecal Management System used in this study included a silicone catheter, balloon, petroleum jelly, hanger, collection bag, bed sheet clip, syringe, and drape, designed for collecting liquid or semiliquid stool (refer to Figure 2).

4.2.2. Operation Method
Initially, evaluate patients’ perianal skin condition and confirm that informed consent is obtained from family members. Position patients in the lateral or supine position, preferably lateral, wearing sterile gloves. Connect the catheter to a disposable drainage bag, lubricate the catheter tip with paraffin oil, and gently insert it into the anus to a depth of 4-6 cm. Inject 45 mL of saline into the balloon and secure the fecal collection bag at the bedside, noting the date and time of use.
4.2.3. Postintubation Management
(1) Inspect the catheter twice daily. (2) Daily, nurses should record defecation volume and assess whether to replace or empty the collection bag. (3) Regularly check for any perianal mucus or fecal leakage, managing with conventional toilet paper and absorbent pads if detected. (4) Daily, cleanse the catheter with 30–50 mL of warm saline to ensure unobstructed flow and prevent blockages. If blockage occurs and flushing fails, remove the catheter immediately and assess the need for reinsertion. (5) To prevent catheter prolapse and intestinal mucosa damage in restless patients, consider restraining their hands.
4.2.4. Precautions for Intubation
(1) Monitor for water leakage from the airbag and ensure the catheter is securely positioned to prevent fecal overflow. (2) Periodically deflate the balloon to avoid prolonged intestinal wall compression, which could cause ischemia and necrosis. (3) Discontinue FMS use if excessive fecal leakage occurs. (4) If feces are too thick, administer Lactulose Oral Solution (1 bag three times daily) orally or via tube. If obstruction persists, deactivate the FMS and consider withdrawing the patient from the study.
5. Outcome Evaluation
Primary outcomes included anogenital skin changes (IAD and pressure ulcers), catheter displacement, fecal leakage, and rectal mucosal bleeding in the FMS group. Secondary outcomes encompassed average daily nursing time (involving replacement, cleaning, and repositioning), hospital stay duration, nurse satisfaction (assessed with a custom scale from 0 to 100, where >80 indicates very satisfied, 60–80 satisfied, and <60 dissatisfied), and frequency of FI episodes (times per day).
6. Statistical Analysis
Categorical data were presented as numbers and percentages and continuous data as means ± standard deviation. We used the independent sample t-test for normally distributed continuous data and the chi-square test for categorical data. Statistical significance was established at P < 0.05. Data analyses were conducted using GraphPad 9.0.
7. Results
7.1. Subject Demographics
From January 2020 to March 2023, we enrolled 381 patients with FI in the GICU and NICU of our hospital. This cohort included 134 patients in the FMS group and 247 in the UC group. Both groups had similar baseline characteristics, including age, gender, height, weight, body mass index (BMI), use of sedative drugs, nutritional support, oxygen supply, and history of diabetes and hypertension. The data were comparable across groups. Notably, 57.46% of patients in the FMS group and 55.47% in the UC group, all critically ill, required invasive ventilation. Approximately one-fifth of the patients in each group died during hospitalization (refer to Table 1 for details).
| Group | FMS (n = 134) | UC (n = 247) | p |
|---|---|---|---|
| Age (y) | 62.49 ± 16.91 | 63.60 ± 17.22 | 0.546 |
| Gender (male: female) | 82 : 52 | 147 : 100 | 0.749 |
| Height (m) | 1.65 ± 0.09 | 1.66 ± 0.09 | 0.301 |
| Weight (Kg) | 64.00 ± 10.36 | 64.98 ± 11.41 | 0.409 |
| BMI (kg/m2) | 23.29 ± 2.79 | 23.36 ± 3.19 | 0.831 |
| Diabetes | 23 (17.16%) | 57 (23.08%) | 0.176 |
| Hypertension | 70 (52.24%) | 109 (44.13%) | 0.130 |
| Sedative drug use | 95 (70.90%) | 186 (75.30%) | 0.350 |
| Department of the patients | 0.472 | ||
| GICU | 61 (45.52%) | 103 (41.70%) | |
| NICU | 73 (54.48%) | 144 (58.30%) | |
| Nutrition | 0.840 | ||
| Oral entry | 6 (4.48%) | 11 (4.45%) | |
| Enteral nutrition | 41 (30.60%) | 80 (32.39%) | |
| Enteral nutrition | 48 (35.82%) | 87 (35.22%) | |
| Enteral + parenteral nutrition | 45 (33.58%) | 69 (27.94%) | |
| Oxygen delivery | 0.952 | ||
| Nasal catheter | 33 (24.63%) | 67 (27.13%) | |
| Face mask | 24 (17.91%) | 43 (17.41%) | |
| Trachea intubation | 51 (38.06%) | 93 (37.65%) | |
| Tracheotomy | 26 (19.40%) | 44 (17.81%) | |
| Clinical outcomes | <0.0001 | ||
| Cure OR | 115 (85.82%) | 168 (68.02%) | |
| Remission | |||
| Death | 9 (6.71%) | 62 (25.10%) | |
| Others | 10 (7.46%) | 17 (2.83%) |
7.2. Primary Outcomes
The incontinence-associated dermatitis (IAD) scores were significantly lower in the FMS group compared to the UC group (P < 0.05), indicating reduced skin damage. The incidence of IAD was 21% lower in the FMS group (P < 0.01, Table 2). The Braden Scale scores were also higher in the FMS group, indicating a reduced risk of pressure ulcers compared to the UC group (P < 0.05). It is worth noting that the IAD scores in both groups had a high degree of dispersion, and the difference in pressure ulcers was not statistically significant, which may be related to the high number of deaths during hospitalization. In terms of nursing management, FMS usage reduced the average daily nursing time from 152 minutes to 63 minutes, a 59% decrease. The length of hospital stay was 18% shorter in the FMS group. Nurse satisfaction was notably higher with FMS usage, enhancing job satisfaction and reducing workload. Additionally, the higher usage of cathartics in the FMS group might have increased FI incidence. The duration of FMS usage ranged from 1 to 29 days, with a median of 4 days.
| Group | FMS (n = 134) | UC (n = 247) | p |
|---|---|---|---|
| IAD score | 9.42 ± 9.28 | 11.98 ± 11.72 | <0.05 |
| IAD | 24 (17.91%) | 95 (38.46%) | <0.01 |
| Braden Scale score | 10.42 ± 2.77 | 9.71 ± 2.56 | <0.05 |
| Pressure ulcer | 11 (8.21%) | 36 (14.57%) | >0.05 |
| Average daily nursing time | 63.13 ± 10.35 | 151.74 ± 13.46 | <0.0001 |
| Length of stay (d) | 13.35 ± 10.70 | 16.21 ± 10.74 | <0.05 |
| FMS usage time (d) | 5.40 ± 4.21 | — | — |
| Nurse satisfaction | <0.0001 | ||
| Very satisfied | 93 (69.40%) | 47 (19.03%) | |
| Satisfied | 29 (21.64%) | 98 (39.68%) | |
| Dissatisfied | 12 (8.96%) | 102 (41.30%) | |
| FI frequency (times/day) | 4.81 ± 2.84 | 3.28 ± 1.97 | <0.0001 |
| Use laxatives | 47 (35.07%) | 22 (8.91%) | <0.0001 |
| Bristol Stool Scale | <0.05 | ||
| Type 1–5 | — | — | |
| Type 6 | 55 (41.04%) | 133 (53.85%) | |
| Type 7 | 79 (58.96%) | 114 (46.15%) |
7.3. Safety of Using FMS
Five patients (3.73%) experienced FMS-related complications, with one patient (0.75%) requiring surgical intervention (see Table 3). The first case involved an 85-year-old female admitted with traumatic acute subdural hemorrhage and a 20-year history of type 2 diabetes. On the ninth day of FMS use, hematochezia occurred and examination revealed rectal mucosal bleeding. Initially, conservative treatment and management with gelatin sponge packing were used to control the bleeding, but these measures were ineffective, and bleeding persisted. Subsequently, suturing and ligation of the bleeding site were performed, which successfully stopped the bleeding. The second patient, a 74-year-old female, was diagnosed with lung cancer and had histories of grade 3 hypertension for 17 years and type 2 diabetes for 15 years. Hematochezia appeared on the third day of FMS use, and an examination revealed rectal mucosal ulceration. Anticoagulation was discontinued, and conservative treatment was administered, leading to improved symptoms. Additionally, three patients (2.24%) experienced leakage of fecal juice around the catheter. Despite attempts to replace the catheter, the results remained unsatisfactory, prompting the discontinuation of FMS use.
| FMS-related complications | Cases | Management | FMS use time | Signs | Admission main diagnosis | Outcome |
|---|---|---|---|---|---|---|
| Catheter shedding | 0 | — | — | — | — | — |
| Mucous bleeding | 1 | Suture ligation, compression hemostasis | 9d | Hematochezia | Traumatic acute subdural hemorrhage | Discharged after improvement |
| Catheter blockage | 0 | — | — | — | — | — |
| Seepage of excrement | 3 | |||||
| Terminate FMS | 2d | Stool leakage | Traumatic subdural hematoma | Cure | ||
| Terminate FMS | 4d | Stool leakage | Hepatapostema | Cure | ||
| Terminate FMS | 4d | Stool leakage | Lung infection | die | ||
| Mucosal ulcer | 1 | Conservative treatment, stop anticoagulation | 3d | Hematochezia | Lung cancer | Discharge after improvement |
8. Discussion
FI is highly prevalent among hospitalized patients. This condition damages skin integrity and significantly impacts patients’ quality of life, increasing social and psychological issues [3, 5, 19]. Consequently, the study of FI has become increasingly important. Compared to patients in general wards, critically ill patients exhibit higher incidences of FI, IAD, and pressure ulcers. This is attributed to their critical condition, reduced physical stress tolerance, and decreased activity and consciousness levels [20]. Historically, FI treatment in intensive care primarily involved using pads or bags for fecal management, complemented by various skin protectants [15, 21]. However, nursing care for these patients is labor-intensive, time-consuming, and costly, presenting significant challenges.
FMS has proven to be an effective tool for fecal management in critically ill patients, offering benefits like replacing surgical intestinal shunts, preventing perianal skin abrasion, and reducing nosocomial infection spread [22–24]. The FMS in this study collected feces from critically ill FI patients, containing both fluid and semifluid feces in its system to prevent leakage, protect perianal skin, and minimize frequent patient repositioning. The previous research study has supported FMS’s efficacy in reducing infections, incontinence-related dermatitis, and stress injuries [23, 25]. Our results also confirmed these findings. The FMS group showed lower IAD scores (9.42 ± 9.28) than the UC group (11.98 ± 11.72), with a significantly reduced incidence of IAD (17.91% compared to 38.46%). These findings demonstrate that the FMS group experienced both a lower incidence and severity of IAD than the UC group. Additionally, the Braden Scale scores, which assess pressure ulcer risk, were higher in the FMS group (10.42 ± 2.77) compared to the UC group (9.71 ± 2.56), suggesting a reduced risk of pressure ulcers in the FMS group. Moreover, a clinical evaluation by Padmanabhan A and colleagues found that a high percentage of nurses (83% to 90%) agreed or strongly agreed that FMS was user-friendly, time-saving, and effective for both nurses and patients [26]. Regarding costs, a significant patient consideration, a study by Langill et al. showed that the material costs of using FMS are substantially lower than those of traditional nursing methods. On average, the daily material cost for each ICU patient using FMS was $93.74 less than that incurred by the traditional approach [27].
It is vital to recognize that FMS usage may pose risks to some patients. Although rare, severe complications including rectal ulcers, fistula formation, and bleeding can occur with FMS use [16, 28]. However, it should be emphasized that for most patients with FI, FMS is a safe and effective treatment option. Our study corroborates this finding. Only a small percentage of patients (3.73%) experienced complications related to FMS, with surgical intervention required for just one patient (0.75%) due to rectal mucosal bleeding. Although the incidence of FMS-related complications is low, we strongly recommend a comprehensive patient evaluation before initiating FMS treatment. It is crucial to carefully assess the risk-to-benefit ratio for patients with compromised rectal mucosal blood flow. Additionally, it is essential to implement a stringent post-device observation plan. Further research is necessary to enhance our understanding and improve the prevention and treatment of FMS-related complications.
9. Limitations
Firstly, as a retrospective analysis conducted at a single center, our study is limited by a small patient sample and inherent biases of retrospective cohort designs, such as selection and information biases, which may affect the generalizability of our results. Secondly, the study may underestimate the true incidence of rectal injuries caused by the use of FMS as asymptomatic rectal ulcers or bleeding may have gone undetected. Finally, the lack of postdischarge follow-up data restricts our ability to assess the medium- to long-term impacts of FMS on patient outcomes. To address these issues, future prospective, multicenter, randomized controlled trials with longer follow-up periods are necessary.
10. Conclusions
Our study demonstrated that FMS provides a user-friendly, easily mastered, and highly satisfactory solution for managing fecal incontinence (FI). FMS has proven to be time-saving, labor-saving, cost-effective, and associated with fewer complications. FMS is an ideal method for protecting perianal skin, especially suited for critically ill patients with FI or diarrhea. Therefore, FMS merits widespread clinical adoption and utilization.
Ethical Approval
The study obtained approval from the Ethics Committee of Shanghai Fifth People’s Hospital (No. SFPH 2023-124).
Consent
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
Authors’ Contributions
Xiecheng Zhou and Ying Yue have equally contributed to this work and share the first authorship. Jian Shi and Yuankun Cai contributed equally to this work.
Acknowledgments
This study was supported by grants from the Minhang District University Discipline Construction Project (No. 2020MWDXK02) and Research Topic of Natural Science in Minhang District (No. 2021MHZ038).
Open Research
Data Availability
The data supporting the findings of this study are not publicly available due to privacy and ethical considerations. However, they can be obtained from the corresponding author upon request.




