Patients’ Reasons to Consider and Their Attitudes toward Complementary and Alternative Medicine
Abstract
Purpose. In recent years, decision-making between conventional medicine, complementary medicine (CM), and alternative medicine (AM) has been studied. The purpose of this study is to take a closer look at patients’ thoughts regarding AM and CM and, if possible, to identify differences. Patients and Methods. Ten cancer patients were recruited to participate in a guided semistructured interview. Recruitment was via verbal request during counseling sessions for complementary healing methods. The main recruiting criterion was their interest in or use of AM or CM. In the following face-to-face interviews, demographic data, previous experience with alternative medicine and conventional medicine, doctor-patient communication, role of the family, and sources of information were determined. The interviews were conducted in a semistructured manner using a guide and were recorded anonymously. The recordings were subsequently transcribed. Results. The number of patients was 10, of which eight were female and seven could show higher educational status. In most of the cases, poor communication was mentioned, both in past situations and at the time of diagnosis. Patients described a lack of emotion in the communication of their diagnosis and paternalistic discussions. They complained that they did not receive an overview of the therapy and that they were hardly involved in the decision-making process. Especially, the demanding content as well as the scarcity of conversation time played an important role for the doctor-patient relationship and the resulting trust toward the doctor. A fundamentally dismissive attitude toward CM, AM, and CAM procedures led to a more fragile trust base. Most frequently used sources were the Internet, support organizations, and books. Conclusion. The first point of contact for cancer patients is usually the conventional physician. Commonly, he is one of the most important sources. If the patient is satisfied with the atmosphere of the conversation and the information regarding CAM received, he will probably follow the doctor’s recommendations. Only in the case of dissatisfaction do patients seek advice from alternative medicine. Good training of conventional physicians in communication and complementary therapy options could, therefore, be of great importance.
1. Introduction
In modern times, it has become evident that a significant number of cancer patients, approximately half, are using complementary (CM) and alternative (AM) medicines.
The utilization rates range from 40 to 70% and have been observed to reach as high as 91% in cases of breast cancer patients [1–4].
However, it is important to know that these two forms of therapy, although often grouped together under the acronym “CAM” (complementary and alternative medicine), are distinct and separate procedures [5].
Complementary medicine refers to evidence-based practices that complement conventional medicine by addressing physical and emotional symptoms, providing patients with skills to manage their well-being during and after the regular cancer treatment. On the other hand, alternative medicine comprises procedures marketed as alternative methods healing cancer without conventional treatments. Alternative medicine is lacking scientific evidence and biological plausibility regarding safety and efficacy [6–8]. For patients, the difference is hard to define in case of a certain method.
With both, patients hope to enhance emotional well-being, to strengthen the immune system and to reduce side effects associated with conventional treatments [5, 9].
While the rate of cancer patients using complementary and alternative medicine increases, data are growing that CAM usage may go along with risks of side effects and interactions [10–13]. Counseling patients on CAM with the aim to reduce these risks and at the same time to increase self-efficacy and patient empowerment is a difficult task for physicians due to lack of knowledge on the topic and high expectations of patients on the effects of CAM [14–16].
In previous studies, various causes could be identified for this trend. Above all, dissatisfaction with communication and time pressure on the part of the physicians in conventional medicine have been analyzed as the decisive criteria why more and more patients resort to CM, AM, or CAM [17, 18].
Gaining deeper insights into patients’ thoughts and experiences regarding AM, CM, and CAM and uncovering additional factors that influence their decision-making with respect to CAM could help to develop counseling strategies. The aim of this study was to fill this research gap and gain a comprehensive understanding of patients’ perspectives in order to contribute to the development of patient-centered approaches to cancer care.
By choosing a qualitative study design, we aimed at eliciting the patients’ views without limiting them in their statements by predefined answer options.
2. Patients and Methods
2.1. Patients
From June 15, 2021, to February 10, 2022, 10 cancer patients were recruited to participate in a guided interview. Recruitment was via verbal request during counseling sessions for complementary healing methods at the University Hospital Jena.
Inclusion criteria were a diagnosis of cancer, age over 18 years, sufficient knowledge of the German language to answer the interview questions, and the interest in or actual use of alternative medical treatment during cancer therapy.
During the recruitment of the patients, we were guided by the “grounded theory.” According to this, patients were recruited as long as new aspects appeared in the interviews [19–23].
With a subject size of 10, we obtained an appropriate and common sample for a qualitative analysis.
2.2. Semistructured Interview
The interview was a semistructured interview conducted with the help of an interview guideline.
The guided interview was based on literature search via PubMed. Several publications were consulted that dealt with the topics of AM, CM, CAM, and decision criteria on the side of the patients [1, 2, 10, 17, 24–30].
Topics that were mentioned more than once or specifically investigated were discussed with experts on CM and CAM.
On this basis, six topics were selected which contain the factors that play the strongest roles in decision-making qualitatively and quantitatively. For each topic, appropriate questions were formulated to provide a comprehensive insight into the topic.
The six topics included 55 main questions (a) and 22 questions for further inquiry (b).
Questions that arose from the conversation were possible and were noted together with the answers in each protocol.
- (0)
Introductory question
- (1)
Demographic data
- (2)
Doctor-patient communication:
- (i)
Scope and setting
- (ii)
Type of communication
- (iii)
Conclusion
- (iv)
Focus on AM
- (i)
- (3)
Experience: Conventional medicine
- (4)
Experience: AM and CAM
- (5)
Influence of family and friends
- (6)
Sources of information
The distribution of questions among the categories is detailed in Table 1.
| Topics | (a) | (b) |
|---|---|---|
| Introduction | 1 | 0 |
| Demographic data | 8 | 0 |
| Doctor-patient communication | 27 | 8 |
| (i) Scope and setting | 6 | 1 |
| (ii) Type of communication | 7 | 3 |
| (iii) Focus on AM | 7 | 3 |
| (iv) Conclusion | 7 | 1 |
| Experience: conventional medicine | 4 | 2 |
| Experience AM and CAM | 6 | 6 |
| Influence of family and friends | 5 | 4 |
| Sources of information | 4 | 2 |
- (a) main question; (b) questions for further inquiry. The bold values indicate the total number of questions in this block.
While introduction and demographic data were intended as short parts of the interviews, doctor-patient communication, past experiences, influence of family and friends, and sources of information were planned without restriction to time and extent of subtopics.
The interviews were recorded pseudonymously, and the data were transcribed anonymously by Tucan.ai and Sonix. After transcription, an analysis was conducted to evaluate factors influencing the decision-making between AM, CAM, and conventional medicine.
The guideline with all interview questions is attached as Supplementary file 1.
2.3. Analysis According to Mayring
The transcribed interviews were evaluated using a qualitative content analysis according to Mayring [31].
All 10 interviews were included in the analysis.
A structuring content analysis was carried out, and a category system was developed in advance. This is similar to the categories from the interview guide. The categories were precisely defined, and a coding guide was created in order to classify the patients’ statements as precisely as possible into one of the categories.
Statements that had no relation to the topic were not included in the analysis (for example, context-free questions from the patients to the interviewer, small talk, etc.).
2.4. Ethics
Participation was voluntary and free of charge. Patients were free to refuse answers during the interviews.
They were informed that participating had no influence on counseling or treatment. Written informed consent was given by all patients before the start of the interview. The study was accepted by the Ethics Committee from University Clinic Jena (2021-2161-bef).
3. Results
3.1. Analysis According to Mayring
All interviews were read and coded by two of the authors (KM and JH). Coding started with the categories of the interview guideline. The interview time as well as the topics raised by the patients varied in the different sections.
All in all, two new categories emerged in the first two interviews spontaneously by the patients. These categories were included in the next interviews as part of the structured questions. No further categories emerged during the other interviews.
For each category, coding used subcategories as appropriate to more precisely denote the information provided by the patients.
Subsequently, a map was created that reflects the categories of the interview as well as Mayring’s analysis in keywords. It contains the main aspects of the interview and thus represents the structure of the results section (see Supplementary file 2).
3.2. Demographic Data
For this study, we collected the data from 10 patients. Of these, eight were female and two were male. Half of the participants belonged to the group of 51 to 65 years old. The age range was 34–85 years. The main cancer type was lymphoma (n = 4), followed by malignant melanoma (2) and breast cancer (2). Others were pancreatic cancer (1) and small intestine carcinoma (1).
Demographics are detailed in Table 2.
| Total | |
|---|---|
| Gender | |
| Female | 8 |
| Male | 2 |
| Age | |
| <35 | 1 |
| 36–50 | 2 |
| 51–65 | 5 |
| 66–80 | 1 |
| >80 | 1 |
| Education | |
| Basic educationA | 1 |
| Secondary educationB | 2 |
| Higher educationC | 7 |
| Type of cancer | |
| Lymphoma | 4 |
| Malignant melanoma | 2 |
| Breast cancer | 2 |
| Pancreatic cancer | 1 |
| Small intestine carcinoma | 1 |
| Religiosity | |
| Evangelic | 4 |
| Catholic | 1 |
| Atheist | 2 |
| Others | 2 |
| No answer | 1 |
- ACertificate of Secondary Education. BGeneral Certificate of Secondary Education. CHigh school/college/university degree.
3.3. Communication between Doctor and Patient during Treatment
In all cases, the physicians accompanying the patients during treatments were different from those at the initial discussion of the diagnosis. In three cases (30%), patients were informed for the first time by the general practitioner that they might have cancer. Others were pathologists, hematologists, and surgeons. The discussions in which the diagnosis was confirmed and a therapy concept was developed were all conducted by hematologists and oncologists.
On average, it lasted about 10 minutes. The spatial atmosphere at the doctor’s office was usually appropriate. However, patients who received their diagnosis in a more private setting, such as at the patient’s bedside or at the dinner table, described a better relationship of trust.
Furthermore, two patients (20%) said they would have liked to have, and three (30%) had a trusted person present during the conversation.
“PATIENT C: “But these are short conversations, they are already without any feeling. It’s already all cold-hearted. So weak.””
“PATIENT B: “The message was quite terrible. He also noticed it, the doctor, and was then very frightened himself, because he saw that I was very close to tears and so was my husband, and then he said: “Oh dear, maybe I made a mistake there and maybe I shouldn′t have said it that way.” So, he tried to back out. But by then it was too late. Of course, we were both shocked by then.””
Additionally, an honest emphatic diagnosis message was important, so that they felt comfortable to express sorrow and worries. None of the 10 patients reported expressing their worries and fears at the time of diagnosis notification. Two patients (20%) mentioned that they would have liked to share their worries but did not do so due to the unfortunate interview situation.
Moreover, six patients (60%) described the conversation as one-sided and dominated by the physician, so there was not enough time to ask any questions. Seven patients (70%) reported only having received the diagnosis in the first consultation but no overview of the further treatment. This group of patients reported not receiving enough information to understand their illness. The information on disease and therapies they received from the physician was described often as not understandable. Most of these patients (60%) said they would have liked to understand their treatment options so that they could be actively involved in planning. At least they would have liked to know why exactly this therapy was chosen.
Nine patients (90%) additionally mentioned that they managed to get a good treatment overview later on. Thus, they were able to participate in decision-making, and as a consequence, trust and well-being increased.
On top of that, it could be determined that, while communication during the first discussion was described as poor by 6 patients (60%), communication during treatment was perceived as emphatic by 7 (70%).
“PATIENT F: “So what bothered me. On the one hand, I am told that the disease is not curable. On the other hand, I’m supposed to get a strenuous chemotherapy and that somehow doesn’t fit together for me and so I refused to do it that way.””
3.4. Knowledge about Alternative Medicine
In the interview, it turned out that four patients (40%) understood AM as supportive medicine. In other words, they described complementary medicine. Only two patients (20%) could distinguish alternative medicine from complementary medicine. Three patients (30%) described all natural healing methods as well as everything besides conventional medicine as alternative medicine. In addition, dietary changes were mentioned by two patients as CAM. Yet, no distinction between AM and CM was described.
Another patient had heard the term before but could not explain it.
3.5. Current Alternative Healing Methods and Diagnostics
“PATIENT H: “They have something that is complementary, supplementary and supportive and that’s where I wanted to like take care of in the direction of mistletoe therapy or also other means. And I will decide it then actively what I do and what not.””
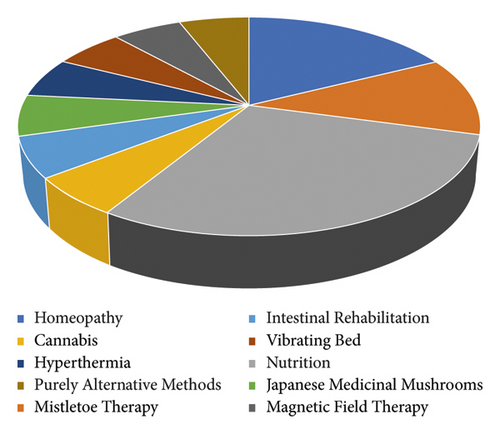
The most frequently mentioned procedures were complementary to typical cancer therapy. The most common procedure was homeopathy. This was followed by mistletoe therapy.
A lot of the other methods were related to nutrition and diet. In the aggregate, they made up the largest part.
They reported using foods such as carrots and garlic to supplement their therapy.
Nutritional supplements and vitamins, such as vitamin D and B, were also mentioned.
“PATIENT E: “I feel a bit nauseous in between. That is supposed to be quite normal with radiation, that you can use ginger, for example. I also got medication from the doctor, but I find it much better now with ginger.””
Further procedures were Japanese medicinal mushrooms, hyperthermia, vibrating bed, and magnetic field therapy. These procedures were also performed in parallel with conventional therapy.
Eye diagnostics was mentioned as a purely alternative diagnostic method. This is a procedure in which the patient’s state of health can be determined based on his eyes.
The same patient also mentioned family constellations, which reveal interactions between family members. These tensions could lead to cancer and would be resolved through this alternative psychological therapy.
Of the many alternative and complementary healing methods available on the current market, the ones described are only those mentioned by the patients themselves.
The following graph also refers to the curative procedures used by this group of patients. It is not transferable to the general public (see Figure 1).
4. Precancer Experience
4.1. AM/CM
In contrast to all patients having had contact to conventional medicine, only eight (80%) had already had experience with AM and CM in the past. Another patient described the experience of a close relative, and one patient had only come into contact with AM and CM at the time of his cancer diagnosis.
While four out of these eight patients reported they had good experiences with AM or CM, three described bad experiences. One patient reported both positive and negative experiences. These bad experiences were based on an unsatisfactory outcome in three out of four cases, and in one case, the treatment approach was described as too alternative.
These methods were homeopathy, globules, Schuessler salts, nutrition, sports, acupuncture, and power of thoughts.
Moreover, they described the visit to an alternative practitioner or alternative doctor as positive. Some of the patients had a general practitioner who also has homeopathic training, so that they could be cared for alternatively, complementary as well as conventionally.
“PATIENT F: “That was the first help I got. So, my impression is that the homeopaths take more time.””
“PATIENT C: “But now completely omitting conventional medicine, that does not exist with me. So I want it to always be primarily conventional medicine and the alternative or nature-based, that should only be accompanying.””
“PATIENT F: “I had a chronic middle ear infection and there was a specialist in Leipzig who prescribed a remedy that was supposed to help. This also helped temporarily, but then no longer. And I was then operated on.””
5. Precancer Experience
5.1. Conventional Medicine in Different Departments
All patients had experience with conventional medicine to treat disease prior to their cancer diagnosis.
“PATIENT C: “Well, you have to say as a patient. That’s just the way it is. You have to be active so that nothing happens to you that you don’t want to happen. So, you know what I mean?””
“PATIENT F: “The doctor was not quite on his toes. I can also prove that. He prescribed a medicine for me to take in the evening. However, he was so responsible that he said: “I don’t want to decide this on my own” and he sent me to the rheumatologist. And the rheumatologist says to me, “so this remedy you take it immediately no more. This is rat poison.” So, the orthopedist here prescribed me a drug that the rheumatologist, who obviously knew better, called rat poison.””
Only two patients (20%) reported exclusively good experiences. These were related to obstetrics and general practitioners for example. None of the patients described entirely bad experiences.
There was also a patient who was a proponent of conventional medicine.
According to his statement, he would never leave conventional medicine out of the equation. Yet, this patient did not comment on whether he would describe his past experiences as negative or positive.
5.2. Influence of Family and Friends
For a lot of patients, family and friends play an important role on the cancer journey. Eight patients (80%) reported involving their partner and immediate family in decision-making. Mostly, partners were described as supportive advisors. They would serve as emotional support, escort to appointments, and take over domestic and family tasks.
Above all, people who have been affected themselves play a major role, as patients can confide in someone who has been through a similar situation.
“PATIENT C: “Well, I discuss everything with my husband. But at the end of the day, I decide and I don’t let anyone change my mind. So, I have my own opinion and I stick to it.””
5.3. Sources of Information
“PATIENT J: “And a woman and also a man smiled at me when I told them about hyperthermia. They said they didn’t believe in it.””
The second source was the Internet. It was used by 90% of patients. Frequently, they searched for the cancer disease and cancer treatments. Besides a lot of misinformation, they usually encountered clinics offering alternative or complementary cures.
“PATIENT B: “The doctors, of course, and the Internet. I enter various search terms and if I come across something that I think might be interesting, I find out about it. But it’s also the case that I don’t believe everything I read. So if I come across something that I think might be interesting, I talk to my doctor.””
One of the most frequently mentioned support organizations was the Biological Cancer Defense in Heidelberg, an organization concentrating on counseling cancer patients on complementary as well as alternative medicine without strict adherence to evidence-based medicine, as well as the German Cancer Aid, a lay organization offering a telephone hotline for medical as well as social problems.
Some got additional information from television and magazines or brochures. Almost all mentioned books as a source of information.
In some cases, health insurance companies and health food stores were also consulted. This was done mainly not only by telephone but also through on-site consultation.
“PATIENT D: “I have a daughter who works in a big international company and this company offers alternative second opinions. And that’s when she asked me if I was in good hands. Especially since I still had questions about some things where I was unsure. And she set that in motion and then all of a sudden, I got a long letter from Harvard University where my treatment was reviewed.””
Some patients actively sought for advice from specialists and affected persons in their circle of acquaintances. Specialists were doctors, nurses, biologists, and pharmacists.
5.4. What Would Improve the Situation?
“PATIENT C: “I would like to see more of the system, that the two treatment methods that exist, the conventional and the alternative, are more in harmony. That a general practitioner or an oncologist can also prescribe this. That in the end, health insurance companies will also cover it. Or even that one gets subsidies, if already not completely taken over.””
Also, they reported they would like to see better physical and psychological care during and after cancer therapy (see Figure 2).

6. Discussion
To the best of our knowledge, this is the first study to examine patients’ thoughts regarding AM, CAM, and CM associated with decision-making using structured interviews.
As patients were free to answer the questions in as much detail as they wished.
The focus of the interviews was primarily on the initial conversations between patients and their treating physicians. It is striking that almost all patients described the first conversation as significantly worse compared to the second conversation.
It is important to consider that the initial conversation usually includes the diagnosis message. While the focus in follow-up conversation is on treatment, medical knowledge and skills, good communication skills are particularly necessary in the initial conversation, especially since this involves the delivery of bad news.
Similar findings have been made in past studies. While our study looked more closely at the differences in communication between initial and follow-up conversations, it was found in previous studies that physicians have difficulties in delivering bad news [32, 33]. This could be a possible justification of our study result.
It was not only in our study that communication plays a crucial role in the doctor-patient relationship. As this problem has been known for a long time, different communication models have been developed to help improve the communication skills of physicians and to make the delivery of bad news easier for both the patient and the physician. However, studies have shown that even such a model is not fully effective. The question is whether new models should be developed or whether training in the use of these communication models is lacking [32].
Some studies show that applying and practicing such communication models bring success [34–36].
It may be relevant to offer workshops that reinforce these skills. One example from a 2007 study showed that a four-day workshop, called Oncotalk, was sufficient to distinguish between pre- and postworkshop consultations by 91%. The workshop focused on practicing the “SPIKES” protocol. This means that in 91% of the cases, there was a correct and successful application of the model [34].
Another example can be found in a 2017 study comparing communication skills between control and intervention groups in an OSCE. The intervention group received short briefings of only 60 minutes before the exam. These are intensive teaching units in which theory is clarified using video clips. The result of the study was positive and showed that even short, well-chosen teaching units are sufficient to achieve improvement [36].
Whereas, in the past, it was primarily the physician who did most of the talking and the paternalistic model of communication was common; recent studies have shown that the shared decision model is superior [35, 37].
Also, our study showed that most patients prefer to be an active part in the treatment planning process. It was often mentioned that it would have been possible to actively participate in the decision-making process at any time. In most cases, however, patients had not received sufficient information from physicians to weigh options against each other. The latter is consistent with data from other studies [25, 38–40].
“PATIENT G: “So I was able to participate in the decision-making process all along. If I’d had the knowledge I have now before, I probably would have asked differently.””
Nevertheless, physician-controlled decision was also said to be acceptable, provided that the motives are well comprehensible and explained to lay persons.
“PATIENT G: “But I think |you| just have to work on it with the people, they are overrun, they have no knowledge and there is only the Internet with bad information. But |you| just have to give the options clearly on the way.””
Besides questions about the initial interview, we also asked for past experiences in AM and conventional medicine.
Our data indicate that most patients had positive experiences with AM and CM treatments. These experiences are mainly based on trust and the way they are treated by alternative practitioners. Already in past studies, it could be shown that alternative medicine fulfills almost all wishes and prerequisites for a successful doctor-patient relationship [41].
While, in conventional medicine, the focus is on the treatment of a disease and its symptoms, alternative practitioners address all areas of the patient’s life in a detailed discussion [41, 42].
In addition, the alternative healing methods appear tangible to the patient in their mode of action. They are easy to apply from home and are sold by alternative practitioners with a positive outcome. Finally, this professional group works with the idea of self-efficacy and the strengthening of one’s own self-healing powers. Besides the reduction of side effects of conventional therapy, these two points are the main concerns of a cancer patient regarding the visit of an alternative practitioner [2, 42].
On top of that, our study showed that patients were unlikely to leave conventional medicine out of the equation and would like to see a combination of it, AM and CM. This result is also in line with past studies. In a study focusing on the expectations of nonmedical practitioners, it was shown that, although patients have confidence in this professional group, conventional medicine was superior in all points investigated [42].
In contrast to the descriptions regarding alternative medicine, many negative experiences were described in conventional medicine. A large proportion of the bad experiences were made in hospitals.
One explanation for this could be that hospitalization is usually accompanied by the suspicion of a more serious illness, in which the patient enters the consultation with more awe and is confronted with a foreign physician.
The question now arises as to how a patient’s trust develops.
In a study from 2021, the authors reported that trust consists of an institutional and interpersonal aspect [43].
While the institutional aspect is based on trust in the healthcare system, the interpersonal aspect plays a greater role in our study because it includes an appropriate communication on the part of the doctor as well as the presence of a doctor with whom the patient knows he is in good hands [43].
Another study found that longitudinal care by the same doctor and the patient’s experience with consultation are the main reasons for trust [44].
“PATIENT J: “There is always a new doctor. You don’t have a regular contact person, and that’s really bad.””
It is difficult to circumvent this problem completely, as it is hardly possible to change clinical structures from scratch. However, one could try to minimize the problem by developing the communication skills of physicians and educating them about this problem to fulfill at least part of the requirements for trust.
A further noteworthy aspect is the influence of family and acquaintances on the decision-making process.
In past studies, it has been shown that the family plays a major role in the treatment of a cancer patient. The main function was described as a supportive one. This is consistent with the results of other studies [45, 46].
“PATIENT H: “Alternatively, the wish would have been. Yes, but it was out of the question for me anyway when I first became ill. My children were much smaller. And I couldn’t get out of the number. I have to do something; I have to work and do something evidence based. In hindsight, I kind of question it. Yeah, I don’t know if it was all right.””
At this point, it would be interesting to find out if the fact that a patient with a relapse and already aware of the side effects of conventional therapy would have a propensity for CM and AM procedures. However, this cannot be proven from our study because neither the group of subjects nor the number of patients is adequate for this purpose.
Not only the family but also other sources of information play a crucial role in the journey of a cancer patient.
Since we already knew from other studies that the physician is one of the most important sources of information for patients, it was no surprise that our study result was also in line with these data [47–49].
Considering the focus of our study, it was striking that almost all patients reported being dissatisfied with the reaction to the request for CAM as well as the counseling regarding these methods.
There are two possible explanations for this. On the one hand, patients described a pejorative attitude of physicians regarding the topic of CAM, on the other hand, inadequate advice. The former may be due to the low level of evidence on most CAM methods in cancer care [50].
Yet, using CAM may increase adherence to conventional cancer treatments as well as quality of life.
This is a strong argument why physicians should provide information and counseling about it [2, 41, 51, 52].
The second aspect, the counseling, could be explained by the fact that the knowledge about evidence-based CAM methods is still very small and the knowledge of some physicians even smaller [51, 52].
This could be shown in a recent study from Beirut. This study found that, in summary, both doctors and nurses are open to CAM but do not feel able to advise on it, although 67% are convinced that it can increase patient satisfaction [52].
It is, therefore, not only in our study that it would make sense to offer further training on this topic: on the one hand, to ensure a comprehensive and good consultation and on the other hand, to protect our patients from obtaining the necessary information from untrustworthy nonmedical personnel or websites.
7. Limitations
Since this study is qualitative, we refrained from performing statistical analyses of associations with demographic data. Due to the small group of subjects, only a small impression is possible. This is largely consistent with the literature.
To be able to clearly prove associations, the group of participants would have to be enlarged many times over.
While in many previous quantitative studies, correlations between gender, age, and different outcomes could be established, this is also not possible in our study not only because of the small number of participants but also because of the imbalance between male and female gender and age distribution.
The second limitation refers to the splitting between the terms AM and CM.
While many past studies have examined the influencing factors in decision-making regarding conventional medicine and AM/CM, it would have been interesting to find out if there are also differences regarding AM and CM [48, 53, 54].
The prerequisite for this is that patients should be able to separate these two terms and that their therapies are either alternative or complementary. In our study, there was not a single patient who did not use both procedures.
8. Conclusion
The diagnosis of cancer makes patients feel like they are losing control over their bodies. Therefore, it is even more important for them to strengthen their self-efficacy. They want to contribute to their own health [2, 6, 49]. The easiest way is through CAM. For this, however, patients need good advice and support from the doctors. The prerequisite for this is intensive and regular training of conventional physicians. Said training should consequently be the promotion of communication skills as well as the knowledge regarding CAM methods. Even if some of these methods are already part of the curriculum, they should be given a higher priority in the studies due to the growing interest.
Patients who feel that they have received good advice and are taken seriously usually establish a relationship of trust with their physician. This is necessary to optimize participatory decision-making and patient compliance.
However, if trust in the physician is lacking or the patient does not feel taken seriously, they are more likely to turn to a nonmedical practitioner. After all, they are said to have the communication skills and empathy that are often lacking in conventional medical practitioners [41].
This may be one reason why patients who initially have an interest in CM may end up in AM treatment.
In summary, the first encounter with conventional medicine sets a milestone for the patient’s decision-making. It should be the duty of the doctor to advise a patient as best as possible and to protect against dubious offers. The best way to do this is through proper communication and the ability to adequately inform the patient about the benefits and risks of AM, CM, and CAM and to refer them to specialized departments.
- (1)
A need for information regarding CAM emerged in the group of participants
- (2)
Several patients criticized the communication skills of some physicians
Since 10 is not a representative number for all cancer patients, it would make sense to examine the above results in a second quantitative study with a larger number of patients. This could be done for the first result by using a questionnaire, which represents the medical knowledge concerning CAM and shows gaps if applicable.
Secondly, the results could also be evaluated by using a questionnaire. Here, it would also make sense to ask not only the doctors about their training in communication but also the patients about their positive and negative experiences in communication during their cancer treatment.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Acknowledgments
The authors acknowledge the open access funding enabled and organized by Projekt DEAL.
Open Research
Data Availability
The transcripted interview data used to support the findings of this study are available from the corresponding author upon request. Some statements from patients were translated and are included in the article. The Mayring analysis data, transformed in a mindmap, used to support the findings of this study are included within the supplementary information files. The interview guideline used to support the findings of this study is included within the supplementary information files.