The Acceptability, Feasibility, and Effectiveness of Breast Massage Combined with Acupoint Stimulation to Promote the Volume of Human Milk in Mothers with Preterm Infants: A Pilot Study
Abstract
Background. Preterm infant mothers have always encountered difficulties in human milk production. For this reason, an intervention of breast massage combined with acupoint stimulation was designed to increase the production. Purpose. Through a pilot randomized trial, we assessed the acceptability, feasibility, and effectiveness of breast massage combined with acupoint stimulation and the study procedures. Methods. 40 participants of preterm infants born at less than 34 weeks of gestation were randomly allocated to the CG (control group) or the EG (group with breast massage combined with acupoint stimulation). Data related to the acceptability, feasibility, and effectiveness of the intervention and research procedures were collected and analysed. Results. The daily volume progressively increased each day in the first 7 days in both groups and a significant difference was observed between the groups (P < 0.001). The initiation time of lactogenesis stage II was 50.06 ± 6.78 (40.00–64.00) hours in the EG and 66.18 ± 14.64 (48.00–96.00) hours in the CG, where a significant difference was detected (P < 0.05). The mean score of satisfaction with the intervention in the EG was 4.56 ± 0.32 (4.0–5.0), while the retention rates were 82.5% and 85.5% (17/20) in the CG, and 80% (16/20) in the EG. Conclusion. This pilot study was oriented towards the effectiveness of breast massage combined with acupuncture stimulation for the increase of human milk production in the participants. The intervention was accepted well and the study process was reasonable. A large-scale RCT will be able to determine the beneficial effects of this intervention on human milk production.
1. Introduction
Breastfeeding has unparalleled advantages in both optimal infant development and the intimacy between mothers and infants, for preterm infants in particular. Research has demonstrated that human milk can reduce complications in preterm infants, including bronchopulmonary dysplasia, retinopathy, infection, such as meningitis, sepsis, and necrotizing enterocolitis [1, 2]. Thus, the World Health Organization has claimed that breastfeeding is the best choice for premature infants [3]. As the nutritional composition of human milk in different stages continuously changes, the suitability of milk for the growth and development of premature infants can be ranked from best to worst in the order of human milk from the mother, donor human milk, and formula milk [3].
Although human milk from the mother is the best choice for preterm infants, insufficient production is common among mothers [4]. The reasons are as follows [5, 6]: the baby is born with a small gestational age and the mammary gland of the mother is immature; there is no early, regular, and frequent emptying of the breast; the skin contact between the mother and the baby is reduced; the mother is feeling stressed or anxious; and the effect of certain demographic factors (the mother’s age, income, education level, marital status, and so on).
Mothers often report that failure to express enough human milk induces feelings of hopelessness and guilt, especially when infants thereof are in the NICU, as human milk is considered by mothers as the only positive contribution that can be made [7].
For mothers who are faced with this problem, a systematic review by Cochrane [8] recommended a number of procedures, including early skin-to-skin contact and bedside expression/pump, early initiation and frequent emptying of the breast, use of a hospital-grade breast pump, relaxation therapy (meditation and music therapy), peer support, and professional help from a lactation consultant. These methods can be effective for some mothers, but the amount of increase might still be insufficient [9]. Hence, an additional method to boost human milk production is proposed.
Lu et al.’s study mentioned that breast massage combined with acupoint stimulation has been revealed to be effective in increasing the human milk production of mothers who underwent caesarean section [10]. However, the study began 48 hours postpartum and only lasted 2 days and the method was conducted 1 side at a time, taking 15 minutes for each side and yielding a total treatment time of 30 minutes per day. Compared with mothers who underwent caesarean section, the treatment might not be sufficient for mothers of preterm infants that experience a long period of separation from their infants, particularly those whose gestation age is before 34 weeks.
Breast massage is premised on the theory of viscera and meridians combined with the anatomy of Western medicine [11, 12]. Performing pushing, pressing, and kneading on the breast, areola, and nipple with hands and fingers to promote blood circulation has been demonstrated to be effective in breastfeeding management [12]. A systematic review [13] identified the effectiveness of breast massage as a treatment for women with breastfeeding problems. In this review, breast massage was found to facilitate the flow of milk for mothers while pumping, so as to establish a milk supply. Despite this, the use of breast massage in mothers of premature infants was not confidently ascertained in this review. Jones et al. [14] reported breast massage enhanced the human milk supply of mothers, but these results were reported after one pumping session without noting time or day. The findings of Cho et al. [15] were made using an uncommon outcome measurement by counting the number of sucks of a neonate feeding directly at the breast per minute, which has not been replicated in further related studies. An observation can be made that there is a scarcity of research on breast massage that focuses on the initiation time of lactogenesis stage II, which is closely related to the success of breastfeeding [16].
Acupoint simulation is another kind of ancient Chinese massage that originated about 2000 years ago and has made appearances in the history of European and North American medicine [17]. Massage techniques can vary but generally proceed according to the following: pressing, rubbing, pushing, holding, kneading, beating, and so on, which are used not only in isolation, but also in cooperation with each other [18, 19]. According to Dong’s master’s project survey, the top five acupoints used frequently to treat postpartum hypogalactia were Tanzhong CV17, Rugen ST18, Shaoze SI1, Zusanli ST36, and Hegu LI4 in China in the last 30 years [20]. A study in Italy also proved the acupuncture points Tanzhong CV17, Rugen ST18, and Shaoze SI1 effective in increasing human milk secretion, but the subjects of this study were normal term mothers, not the mothers of preterm infants that experience a long period of separation from their infants [18]. Zhu et al. [21] employed acupoint massage to increase human milk secretion, but this intervention began 3 days after caesarean, as the colostrum is vital for preterm infants within 1–2 days of birth, which is used in oropharyngeal administration for considerably low birth weight infants and can reduce necrotizing enterocolitis [22]. Several studies lacked precise calculation of the human milk quantity. Here, the volume of human milk was measured by an electric breast pump for 15 min, 1 hour after the last breastfeeding of the baby [23], and the satisfaction of baby after breastfeeding was taken into account [17, 23]. However, the speed of milk secretion is different at different times and unsettled babies are most often misunderstood as being a factor of insufficient milk supply [24]. No data of lactogenesis stage II has been found in the previous studies on acupoint simulation.
Thus, a hypothesis of the present article is that breast massage combined with acupoint stimulation could increase human milk secretion and the initiation time of lactogenesis stage II of mothers of preterm infants separated therefrom. From the present understanding, this was the first time breast massage was combined with acupoint stimulation to increase the curative effect, especially in mothers of preterm infants. Compared with other valuable studies, the present intervention was conducted in the whole period of separation between mothers and infants, being initiated within 24 hours and lasting until the separation was over. Further, the measurement of the expressed human milk in 24 hours was more accurate than one pump session and considering the satisfaction of infants. In this pilot randomized control study, the acceptability, feasibility, and effectiveness of the intervention and research procedures were assessed.
The aim of the pilot RCT was to answer three questions. (1) Will mothers of preterm infants accept breast massage combined with acupoint stimulation? (2) Is the research process feasible? (3) Is the intervention effective on human milk production?
2. Materials and Methods
2.1. Study Design
A randomized control test study was designed to evaluate the acceptability, feasibility, and effectiveness of the intervention of breast massage combined with acupoint stimulation and research procedures in the mothers of preterm infants.
2.2. Setting and Sample
The pilot study was conducted in a level-III obstetrics hospital in Shanghai, China, where recruitment was initiated at the postpartum ward from September 08, 2019, to January 31, 2020. This level-III hospital is a baby-friendly hospital with a birth number of 15,000 per year. Moreover, the hospital accommodates three full-time IBCLCs (International Board of Lactation Consultants) and three part-time IBCLCs who are responsible for the education and professional lactation support of all the pregnant and maternal women patients. All mothers of preterm infants receive education from these six IBCLCs about the importance of human milk, the methods of expressing milk by hand and pump, and the knowledge of storage and delivery of human milk. In addition to the above instructions, all mothers of preterm infants receive standard nursing, namely, early skin-to-skin contact if the physical condition of the infant is stable, delivery of human milk to the NICU if so desired, and receiving information about the health condition of the preterm infants from pediatricians.
Mothers were included in the trial, if they (1) had a baby with a gestational age before 34 weeks, (2) were 18 years or older, (3) had a preterm baby in NICU, and (4) were willing to express milk and participate in the trial. Mothers were excluded if they (1) were unable to breastfeed, (2) were reluctant to express milk, (3) had serious complications that would affect the expression, (4) had a mental disorder, or (5) had difficulties in listening, speaking, reading, or writing that would affect communication.
All eligible mothers were selected by the nurses in the ward, hereinafter referred to as the main researcher (MR). The MR visited the mothers within 24 hours after delivery. Here, the aim and procedure of the pilot trial were presented and explained to the mothers, upon which consent was required. The pilot project was approved by the Institutional Review Board at the Obstetrics and Gynecology Hospital of Fudan University, Code number: 2019-120, clinical trial registration number: ChiCTR 1900028699.
2.3. Sample Size
The number of participants who took part in the present pilot trial was 40, which was revealed to be sufficient for the pilot trial [25, 26].
2.4. Randomization
The computer generated a random number table automatically and the participants were randomly assigned to the experimental group (EG) or the control group (CG).
2.5. Binding
No binding was used in the present pilot trial because of the nature of the intervention. Both researchers and participants were aware of the intervention.
2.6. Control
In the CG, the participants received education and support primarily from the IBCLCs in the hospital, including how to maintain early skin-to-skin contact if the physical condition of infants is stable, the benefits of human milk to the preterm infants, the methods of expressing milk by hand/pump, the methods of storage and transportation of human milk, hand/pump cleaning, and the prevention of lactation-related problems [8, 27].
All of the participants were encouraged to express milk by hand and measure the amount of human milk by 1 ml or 5 ml syringes before the onset of lactogenesis stage II, because at this time the amount of human milk was considerably small and expression by hand has been revealed to be more effective without any waste [28]. After lactogenesis stage II, a double electric pump of any brand was recommended and the amount was measured by a small cup accurate to 1 milliliter, the reasons being the following: (1) mothers preferred to use an electric pump when the amount of human milk was large [28]; (2) hospitalized double electric pumps were the preferable choice [8] but were not affordable for all of the Chinese women and there were also no lending options available in the hospital where the study was conducted; (3) double electric pumps have been demonstrated to be effective and time-saving, yet no high quality study has indicated which brand is preferable [8].
Besides the above, MR supervised the expression starting within 6 hours after delivery and at least 6 times a day and instructed the participants to keep expression diary. MA telephoned the participants to give the professional support and collected the data every day until the preterm infants came back to the family and the expression was no longer needed.
2.7. Intervention
In the EG, the MR conducted the intervention on the participants, in addition to the standard care provided in the CG. The MR and a Chinese medicine doctor designed the intervention predicated on a myriad of literature [13–15, 19, 21, 23] in combination with shared clinical experience. The strength of the breast massage ranged from light to heavy, suitable enough to be painless with only the feeling of acid or swelling. The duration of the breast massage was 15–20 minutes per breast before expression. The strength of acupoint stimulation was suitable enough to massage the acupoints with acid, numbness, and swelling (i.e., getting Qi), but was not excessively strong. The duration of acupoint stimulation was 3 to 5 minutes after getting Qi, three times a day. Table 1 illustrates the details of the breast massage and acupoint stimulation.
| Intervention component | Timing and frequency | Description |
|---|---|---|
| Breast massage | <24 h after delivery, before expression (6–8 times per day), 15–20 minutes, 1 side, 30–40 minutes per time | (1) Massage the breast circularly with finger and palm, 20 times |
| (2) Touch the breast with palm and shake it gently, 20 times | ||
| (3) Pat the breast with four finger pulps from the periphery to center, 20 times | ||
| (4) Comb the breast with five fingers from the root to the nipple, 20 times | ||
| Acupoint stimulation | <24 h after delivery, three times a day, 3–5 minutes per acupoint | Press Rugen ST18, Tanzhong CV17, Hegu LI4, and Shaoze SI1 acupoints, with index finger |
| (1) Rugen ST18: located in the chest, under the straight nipple, at the root of breast, level with the fifth intercostal space, 4 inches from the anterior midline | ||
| (2) Tanzhong CV17: located in the chest, the fourth costal space, on the anterior midline, the midpoint of the line between the two nipples | ||
| (3) Hegu LI4: located at the midpoint of the first and second metacarpal bones, when the thumb and index finger are extended | ||
| (4) Shaoze SI1: located 0.1 inches beside the nail corner on the side of the small ruler | ||
The MR contacted the participants within 24 hours after delivery, discussed the process of breast massage and acupoint stimulation with the participants and any family members, and instructed the families how to conduct the intervention by themselves.
The MR would first perform the breast massage with acupoint stimulation personally, so as to demonstrate the process to the observing family members of the participants. Further, a handbook of the methods of breast massage and acupoint stimulation was given to the participants afterwards.
For the next time, the MR instructed the families to conduct the intervention by themselves. If the families had difficulties, the MR would take over and instruct the families again, until the methods were mastered.
Before discharge, the MR observed the family members conducting the whole process at least once to determine whether they had become fully familiar therewith. If the families still had difficulties, the participants would transfer to the CG. At the end of the study, all the participants mastered the intervention before discharge.
In order to ensure the implementation of the intervention after discharge, we have done something as follows. (1) In the intervention design, MR reviewed a large number of literatures, consulted TCM experts, and considered the actual situation. Since the operator might not have a medical background after discharge, the commonly used acupoints in clinic were selected: Tanzhong CV17, Rugen ST18, Shaoze SI1, and Hegu LI4, because these acupoints were located clearly on the chest and hands, which were easy to find. Zusanli ST36 was deleted, because Zusanli ST36 was on the leg and difficult to find compared with the other four acupoints. (2) As far as possible fixed operators, it was recommended not more than 1-2 family members. (3) In the formal guidance stage, the MR explained the operation steps in detail and encouraged family members to operate together. For example, when MR pressed the Shaoze SI1 acupoint on the mother’s right hand, MR encouraged family members to press the left hand, so that the mother could perceive the strength of both. (4) The handbooks were distributed, including the detailed steps of operation, the operation time and frequency, and the location map of the acupoints. (5) During hospitalization, the MR was a special person to observe and guide the parturient or her family to ensure that they master the operation method, for example, observing the implementation face to face and checking the frequency and timing from the expression diary at least once a day. (6) Before discharge, the MR observed the family members conducting the whole process at least once to determine whether they had become fully familiar therewith. (7) After discharge, the MR telephoned the families at least once a day to ensure the implementation of the intervention.
2.8. Data
In both groups, participants and their families were requested to record a milk expression diary, including the start and end time of expression, left or right breast, the volume of the human milk, the method of the expression (if using a pump, noting the model), and the feeling of the breast (a fullness or engorgement feeling could help determine the arrival of lactogenesis stage II [24]).
A sociodemographic questionnaire was conducted in both groups, consisting of (1) participants’ age, race, education, number of pregnancies, working conditions, mode of delivery, family income, number of children, mode of medical payment, and place of residence; (2) premature infants’ sex, gestational age, and birth weight; and (3) breastfeeding experience and decision. On the basis of the physical condition, the questionnaire was completed by the mother of the premature infant or her family under the guidance of the MR before the end of the trial.
2.9. Data Collection
The MR recruited the participants in the inpatient department, explained the purpose and process of the study, and asked all participants to sign the informed consent form and complete the sociodemographic questionnaire. Meanwhile, all participants were given an introduction on how to record an expression diary. In order to ensure the process of the study, the MR visited the participants every day when they were in hospital and followed up by telephone after discharge every day until the preterm infants were returned to the participants and the expression was finished. The MR assessed the timing and frequency of expression, calculated the amount of human milk, and the initiation time of lactogenesis stage II through the diary every day. Before discharge, the MR investigated the satisfaction with the intervention in the EG by employing a 1–5-point scale.
2.10. Measurement
Daily human milk secretion in the first 7 days refers to the amount of human milk expressed by hand or pump every 24 hours in the first 7 days. In the present study, the moment when the preterm baby was delivered was taken as the starting point.
Initiation time of lactogenesis stage II denotes the duration of time from when the preterm infants were being delivered to when the participants began to feel fullness in their breasts. The participants reporting their breasts felt “noticeably fuller” on a scale of 1–5 (where 1 = no change since giving birth, 3 = noticeably fuller, and 5 = uncomfortably full) indicated the onset of lactogenesis stage II [29, 30].
Participants’ satisfaction with the intervention was investigated by the MR before discharge, adopting 0–5-point scales, where 0 was very dissatisfied and 5 was very satisfied.
2.11. Statistical Analysis
IBM SPSS24.0 software was adopted to handle the data and predominantly included the following aspects: a descriptive statistical method was applied to describe the general data of the research object, in which the measurement data were expressed by means of mean ± standard deviation, and the counting data were expressed by frequency and percentage; Pearson’s chi-squared test or Fisher’s exact test was utilized for comparison of the counting data between groups; T test was used for the measurement data; and a generalized estimating equation (GEE) was employed to compare the repeated measurement data in different groups and times.
3. Results and Discussion
3.1. Results
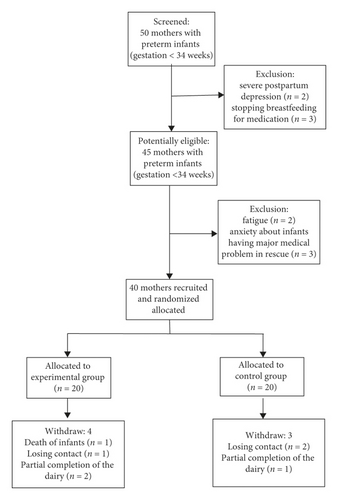
The medical records of 50 potential participants out of 267 preterm mothers were reviewed to screen the eligibility of mothers of preterm infants. 2 were excluded because of severe postpartum depression, while 3 were excluded because they had to stop breastfeeding for medical reasons. Ultimately, 45 participants were recruited. During the recruitment period, the number of eligible mothers was 40, as 88.9% (40/45) agreed to take part in the pilot trial and signed informed consent. The reasons for refusal included fatigue (n = 2) and that the infants had a major medical problem requiring emergency treatment (n = 3). Among these 40 participants, 33 finished the trial. The retention rates were 82.5% and 85.5% (17/20) in the CG, and 80% (16/20) in the EG. As revealed in Figure 1, the reasons for attrition included partial completion of the dairy (n = 3), infant death (n = 1), and loss of contact (n = 3).
As can be observed in Table 2, no statistically significant differences were found between the two groups that completed the trial relating to their sociodemographic characteristics and confounding variables.
| Variable | Experimental group (n = 16) | Control group (n = 17) | P |
|---|---|---|---|
|
31.06 ± 5.07 (25.00–44.00) | 30.88 ± 3.30 (26.00–41.00) | 0.902a |
| Ethnicity, n (%) | — | ||
| Han | 16 (100.00) | 17 (100.00) | |
| Other nationalities | 0 (0.00) | 0 (0.00) | |
| Level of education, n (%) | 0.334b | ||
| High school | 1 (12.50) | 1 (5.88) | |
| Junior college | 7 (37.50) | 4 (23.53) | |
| University | 8 (50.00) | 12 (70.59) | |
| Does mother have a job? n (%) | 0.251c | ||
| Yes | 12 (75.00) | 14 (82.35) | |
| No | 4 (25.00) | 3 (17.65) | |
| Does mother have an insurance? n (%) | 1.001c | ||
| Yes | 16 (100.00) | 15 (88.24) | |
| No | 0 (0.00) | 2 (11.76) | |
| Annual income, n (%) | 0.311b | ||
| $1,000–$2,000 | 3 (18.75) | 1 (5.88) | |
| $2,000–$5,000 | 8 (50.00) | 12 (70.59) | |
| $5,000–$10,000 | 4 (25.00) | 4 (23.53) | |
| More than $10,000 | 1 (6.25) | 0 (0.00) | |
| Residence, n (%) | 1.002c | ||
| Local | 16 (100.00) | 16 (94.12) | |
| Out of Shanghai | 0 (0.00) | 1 (5.82) | |
| Type of pregnancy, n (%) | 1.002c | ||
| Simple | 13 (81.25) | 13 (76.47) | |
| Multiple | 3 (18.75) | 4 (23.53) | |
| Parity, n (%) | 0.291c | ||
| Primiparous | 10 (62.50) | 13 (76.47) | |
| Multiparous | 6 (37.50) | 4 (23.53) | |
| Mode of delivery, n (%) | 0.762c | ||
| Vaginal | 9 (56.25) | 11 (64.71) | |
| Caesarean | 7 (43.75) | 6 (35.29) | |
| Birth weight of preterm infant, g | 1.73 ± 0.34 (1.01–2.19) | 1.58 ± 0.23 (1.10–1.98) | 0.162a |
| Mean ± SD (min-max) | |||
| Gestational age at birth | 31.81 ± 1.53 (28.50–33.60) | 31.91 ± 1.51 (28.40–33.60) | 0.852a |
| Mean ± SD (min-max) | |||
| Previous breastfeeding experience, n (%) | 0.291c | ||
| Yes | 0 (0.00) | 3 (17.65) | |
| No | 16 (100.00) | 14 (82.35) | |
| Timing of the decision on breastfeeding, n (%) | 0.301b | ||
| Before pregnancy | 3 (18.75) | 3 (17.65) | |
| During pregnancy | 6 (37.50) | 7 (41.18) | |
| Since birth | 2 (12.50) | 0 (0.00) | |
| During postpartum | 5 (31.25) | 7 (41.18) | |
- aT test. bPearson’s chi-squared test. cFisher’s exact test.
3.2. Frequency, Duration, and Total Days of Human Milk Expression
In the first week, the frequency of daily milk expression was 6.74 ± 0.77 times/day and ranged from 5.00 to 9.00 times/day in the EG, while that of the CG was 6.79 ± 1.09 times/day and ranged from 5.00 to 9.00 times/day. The duration of expression was 161.04 ± 17.56 minutes/day and ranged from 134.50 to 178.90 minutes/day in the EG, while that of the CG was 170.96 ± 16.35 minutes/day and ranged from 144.50 to 189.90 minutes/day. The total number of days of expression was 43.75 ± 11.50 (28.00–62.00) days in the EG and 38.64 ± 9.18 (29.00 – 64.00) days in the CG. No significant difference was detected between the two groups (Table 3).
Variable Mean ± SD (min-max) |
Experimental group (n = 16) | Control group (n = 17) | P |
|---|---|---|---|
| Frequency of expression, times per day | 6.74 ± 0.77 (5.00–9.00) | 6.95 ± 0.90 (5.00–9.00) | 0.482a |
| Duration of expression, minutes per day | 161.04 ± 17.56 (134.50–178.90) | 170.96 ± 16.35 (144.50–189.90) | 0.762a |
| The total days of expression, days | 43.75 ± 11.50 (28.00–62.00) | 42.65 ± 8.86 (29.00–64.00) | 0.761a |
- aT test.
3.3. Frequency and Duration of Breast Massage and Acupuncture Stimulation
The average frequency of breast massage was 6.73 ± 0.69 (5.00–9.00) times/day, and the average duration was 18.24 ± 1.44 (15.00–24.00) minutes/time. Further, the average frequency of acupoint stimulation was 2.94 ± 0.18 (2.00–4.00) times/day, and the average duration was 4.36 ± 0.64 (4.00–6.00) minutes/acupoint. All of the above met the intervention requirements.
3.4. Volume of Expressed Human Milk
In the first week, the daily volume of expressed human milk was from 0 to 880 ml/day. The average volume of daily expression in the first week between groups is reported in Table 4.
Variable Mean ± SD (min-max) |
Experimental group (n = 16) | Control group (n = 17) |
|---|---|---|
| D1 volume of expressed human milk, ml | 2.51 ± 3.48 (0.00–10.70) | 1.21 ± 1.60 (0.00–5.30) |
| D2 volume of expressed human milk, ml | 48.67 ± 60.72 (7.00–240.00) | 7.64 ± 11.36 (0.00–40.00) |
| D3 volume of expressed human milk, ml | 240.36 ± 87.24 (120.00–350.00) | 86.61 ± 82.26 (0.00–250.00) |
| D4 volume of expressed human milk, ml | 414.69 ± 72.38 (280.00–480.00) | 213.36 ± 137.52 (0.10–400.00) |
| D5 volume of expressed human milk, ml | 533.44 ± 108.67 (320.00–600.00) | 302.65 ± 144.98 (5.00–520.00) |
| D6 volume of expressed human milk, ml | 646.25 ± 133.46 (480.00–800.00) | 394.71 ± 141.43 (120.00–640.00) |
| D7 volume of expressed human milk, ml | 710.00 ± 128.63 (500.00–850.00) | 499.41 ± 160.13 (150.00–650.00) |
The groups and days were used as independent variables to fit the generalized estimation equation. The results indicate that there were significant differences between the experimental group and the control group in the first 7 days after delivery (P < 0.001) (Table 5).
| Parameter | B | SE | 95% CI | P | |
|---|---|---|---|---|---|
| Interception | 681.756 | 25.2109 | 632.344 | 731.169 | <0.001 |
| Control group | −155.762 | 25.1158 | −204.988 | −106.536 | <0.001 |
| Experimental group | 0a | . | . | . | |
| D1 | −599.679 | 30.5403 | −659.537 | −539.821 | <0.001 |
| D2 | −573.982 | 29.5827 | −631.963 | −516.001 | <0.001 |
| D3 | −440.359 | 24.7515 | −488.871 | −391.847 | <0.001 |
| D4 | −290.542 | 19.4793 | −328.721 | −252.364 | <0.001 |
| D5 | −186.970 | 12.6239 | −211.712 | −162.227 | <0.001 |
| D6 | −84.848 | 9.9597 | −104.369 | −65.328 | <0.001 |
| D7 | 0a | . | . | . | |
- aThis parameter is redundant, so it is set to zero.
3.5. Initiation Time of Lactogenesis Stage II
The initiation time of lactogenesis stage II was 50.06 ± 6.78 (40.00–64.00) hours in the EG and 66.18 ± 14.64 (48.00–96.00) hours in the CG. Here, a significant difference was detected (Table 6).
Variable Mean ± SD (min-max) |
Experimental group (n = 16) | Control group (n = 17) | P |
|---|---|---|---|
| Initiation time of lactogenesis stage II, h | 50.06 ± 6.78 (40.00–64.00) | 66.18 ± 14.64 (48.00–96.00) | <0.001a |
- aT test.
3.6. Participant Satisfaction with the Intervention
Before discharge, the mean score of satisfaction with the intervention in the EG was 4.56 ± 0.32 (4.0–5.0).
3.7. Discussion
A pilot RCT aimed at estimating the acceptability, feasibility, and effectiveness of breast massage combined with acupoint stimulation was undertaken, in preparation for a large-scale RCT. From the pilot trial, several conclusions could be drawn.
Firstly, the breast massage combined with acupoint stimulation was well accepted by the participants. In the questionnaire, all the participants in the EG expressed satisfaction or strong satisfaction with the intervention. TCM including Chinese herbal medicine, breast massage, and acupuncture can be found not only in China, but also in other countries. In America, more than 1/3 adults have used TCM [17], while in Sweden, 39% of midwives have recommended acupuncture to women reporting inadequate lactation [31]. All of the aforementioned prior studies did not report the dissatisfaction and serious side effects of participants. In the present study, breast massage combined with acupoint stimulation was chosen for the intervention because of the following reasons: (1) in traditional Chinese culture, for lactation, women can be unwilling to accept medicine; (2) the method of breast massage is simple and easy to master, which has been demonstrated by a previous study [14]; (3) acupuncture requires professionals to pierce the skin with needles, which is not easy to be mastered by participants; (4) acupoint stimulation has similar effects to acupuncture [33] and is easier to be accepted and mastered by participants owing to non-invasiveness.
Secondly, the recruitment percentage was 90% (45/50) and the retention percentage was 82.5% (33/40); this suggests a higher level of satisfaction compared with several prior studies on breastfeeding support in preterm infants [32–36]. In said studies, the recruitment percentage varied from 70% (40/57) [32] to 95% (204/214) [36], while the retention percentage varied from 79% (85/108) [35] to 82.5% (33/40) [32]. This could potentially be attributed to the professional support given to the participants, which is anticipated by mothers with premature infants [37]. By giving face-to-face instructions, assessing the intervention before discharge, and making a follow-up call after discharge, the participants were facilitated in following the requirements and completing the trial. The diary of expression including the time, duration, and amount of expression not only allowed for the collection of data, but also recorded the behavior of expression and promoted the participants to follow the instructions.
Thirdly, the randomized process of the trial was verified. The participants were grouped according to a randomized table generated by computer. The analysis of the characteristics of the participants revealed that the randomization was effective. Each of the participants was in a single room in the hospital. The nurses in the ward were asked to help participants transport the human milk to the NICU and not to disclose the situations of other participants. No contact was observed between the participants in the process, thereby revealing that there was no contamination among the samples between the groups.
Fourthly, the results of the pilot trial aligned considerably with the research hypothesis, although the hypothesis could not be supported due to the low statistical power that increased the probability of a type II error [38]. In traditional Chinese medicine, “Qi” is an active main component of the human body: “energy flow” or “life force.” “Xue” is a kind of dense form of body fluid which is acted and stimulated by “Qi.” It goes beyond the definition of “blood” in Western medicine and includes additional media flowing in the meridians. The deficiency or imbalance of the “Qi” and “Xue” can lead to various symptoms of illness, including the inhibition of human milk production. Therefore, our protocol was designed to follow the “Qi” and “Xue” net work of the human body and stimulate the key acupoints to control the mammary gland functions as well as the central balance of the entire body. Breast massage can promote the blood circulation of breast, provide an impetus to milk ejection, and accelerate milk flow [39]. Meanwhile, acupoint stimulation can regulate Qi and blood, relax meridians, and activate collaterals. Further, Rugen ST18 and Shaoze SI1 are able to increase milk production and enhance prolactin levels [40], which is more obvious with the effects of combining Tanzhong CV17 and Hegu LI4 [18, 19]. These four acupoints are commonly used and easy to master. In traditional Chinese medicine, Tanzhong CV17, Rugen ST18, Shaoze SI1, and Hegu LI4 acupoints are commonly used to promote milk secretion [20]. In modern medicine, in some animal experiments, acupuncture effects are mediated by the secretion of neurotransmitters and opioids, as well as by the stimulation of the hypothalamus and pituitary glands. According to modern anatomy, the fourth costal nerve is distributed near Tanzhong CV17, intercostal nerve, subcostal nerve, and anterior thoracic nerve are distributed around Rugen ST18, ulnar nerve is distributed near Shaoze SI1, and flexor nerve is distributed near Hegu LI4. Through massage, work on acupoints, mechanical force into heat, might stimulate the nerve, and through the sympathetic nerve through the spinal cord to the hypothalamus. The initiation time of lactogenesis stage II is closely related to the rate of exclusive breastfeeding at a later period [29, 30]. If the mother of a premature infant does not receive effective support, the initiation time of lactogenesis stage II will be later than 72 hours, which is referred to as a delay [41]. In the trial, the initiation time of lactogenesis stage II in two groups was less than 72 hours, showing that the professional support of the lactation consultant [36], daily telephone follow-up [42], and the use of expression diary [32] could also promote breastfeeding to some extent, in addition to the intervention.
Finally, the balance of benefits and risks between the EG and the CG was considered. The breast massage and acupoint stimulation were noninvasive and would not damage the body. All of the participants were provided instructions for expression by hand and pump, the frequency of expression, the knowledge of the importance of breastfeeding, and methods of storage and transportation of human milk from the MR and IBCLCs, which have been demonstrated to be effective in improving the amount of expressed human milk [43, 44]. All of the participants also received a follow-up call once a day, through which the participants could consult with the MR about any breastfeeding difficulties. Hence, the analysis of the benefits and risks in the pilot trial suggested that the randomized controlled trial was preferable.
3.8. Limitation
Firstly, the pilot trial was conducted in a level-III obstetric hospital in Shanghai, which was a baby-friendly hospital. The results of the pilot trial were representative of a small portion of the population; thus, a multicenter study could be conducted in the future. Secondly, the initial time of the intervention was not evaluated, since one researcher was responsible for the intervention, which was difficult to initiate at midnight. Thirdly, because of the developments of the regional economy and the high ratio of employed mothers, the electric double pump was widely accepted. Once popularized in other regions, the economic burden of mothers purchasing the pump should be considered.
4. Conclusion
The present pilot study was oriented towards the effectiveness of breast massage combined with acupuncture stimulation for the increase of human milk production in preterm mothers. The intervention was well accepted and the study process was reasonable. A large-scale RCT will be able to determine the beneficial effects of the present intervention on human milk production.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Acknowledgments
The authors express their gratitude to the participants of the present study.
Open Research
Data Availability
All the data used to support the findings of this study are included within the article.




