Ischemic Colitis Revealing Polyarteritis Nodosa
Abstract
Ischemic colitis is one of the most common intestinal ischemic injuries. It results from impaired perfusion of blood to the bowel and is rarely caused by vasculitis. We report a case of ischemic colitis revealing polyarteritis nodosa (PAN) in a 55-year-old man. Histological examination of the resected colon led to the diagnosis of PAN.
1. Introduction
A 55-year-old man admitted with acute abdomen surgery proved to be necessary. Histological examination of the pathologic specimens revealed fibrinoid necrosis and destruction of the internal lamina in small and medium size arteries. Although the gastrointestinal tract is frequently involved, it is rare for PAN to be accompanied by severe ischemic colitis as initial presentation [1, 2].
2. Case Report
A 55-year-old man, with recurrent abdominal pain since 10 months treated with antispasmodic drugs, was admitted in Rabta’s Department of Surgery (A), because of fever, abdominal pain, and bloody stool. Abdominal examination revealed mild rebound tenderness.
Laboratory tests revealed severe inflammation. Upper gastrointestinal endoscopy was normal. Colonoscopy showed “ulcerative and bleeding mucosa in sigmoid colon.”
CT-scan revealed “dilatation of sigmoid colon, wall thickening, and hyperattenuation. Colon was distended upstream.”
At laparotomy, the colon appeared cyanotic. Gentle palpation of sigmoid colon caused violaceous discoloration of the bowel. Pulsations were left in the celiac, superior mesenteric, and inferior mesenteric arteries. The entire colon was resected and ileostomy was created.
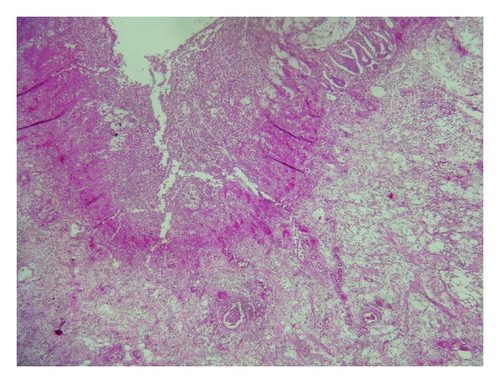
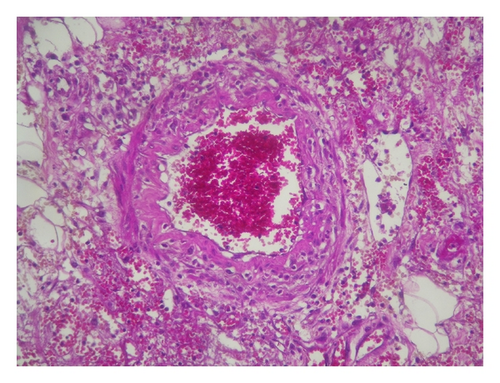
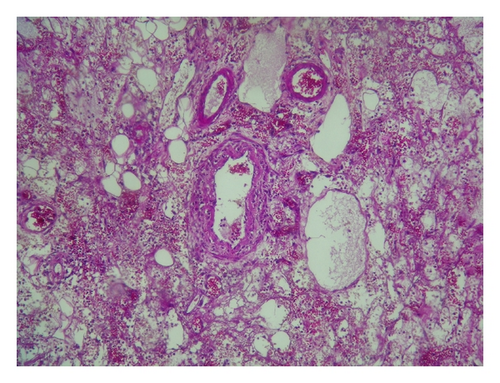
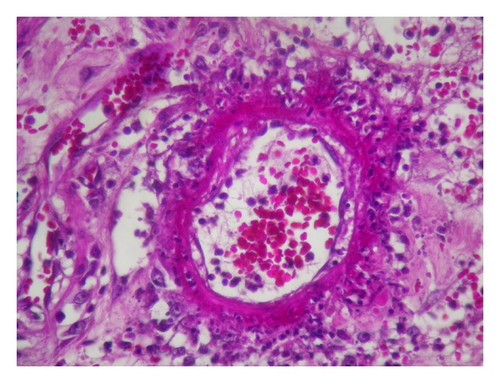
Histological examination of the pathologic specimens revealed “fibrinoid necrosis and destruction of the internal lamina in small and medium-size arteries which are rich in plasma cells, lymphocytes, and neutrophils” (Figures 1, 2, 3, and 4).
He was diagnosed with PAN and was admitted to our department.
Physical examination revealed reduction in tactile sensitivity in the territory of the right peroneal nerve and both ulnar nerves; the electromyography showed multiple mononeuropathy.
Urinalysis, coagulation profile, serum electrolytes and enzymes, serology of hepatitis B and C, antineutrophil cytoplasmic antibody (ANCA), and serum tests for rheumatic diseases were normal.
Computed tomography did not reveal microaneurysms.
Treatment included 3 intravenous pulses of methylprednisolone, 60 mg/day of prednisone, and 12 monthly intravenous pulses of cyclophosphamide. After discharge, a progressive withdrawal of prednisone was accomplished. One year after, PAN has not relapsed.
3. Discussion
We have presented a case of PAN revealed by ischemic colitis necessitating acute surgical intervention.
Polyarteritis nodosa (PAN), first described in 1866 by Kussmaul and Maier [1], is systemic necrotizing vasculitis that predominantly affects medium sized arteries and is primary in most patients but is the consequence of viral infections, mainly hepatitis B virus (HBV), in some. Biopsy material can prove the diagnosis, especially if an affected area or lesion of the skin, muscle, or other tissue is available. The characteristic histopathological changes of PAN are fibrinoid necrosis of the walls of medium or small arteries, with a marked inflammatory response within or surrounding the vessel [2].
PAN involves the gastrointestinal (GI) tract in more than 50% of patients at some time during its course [3, 4].
Clinically apparent ischemic disease of the small bowel is the frequent site of involvement. The colon is less commonly involved [4].
The presentation of colonic PAN may mimic inflammatory bowel disease in young patients and atherosclerotic ischemic colitis in older ones [5]. Thus, any GI symptoms which are preceded by fever, weight loss, myalgia, or arthralgias should raise the possibility of vasculitis. In those patients who do not require an urgent intervention, a deep endoscopic biopsy must be taken. This can give the diagnosis without the need for surgery.
When studying 342 patients with PAN, Pagnoux found that GI involvement was present in 132 cases (37.9%) and was significantly more frequent in HBV related PAN (P < 0.001) [3]. GI manifestations requiring surgery were noted in 48 patients (13.8%). In multivariate analysis, Gl manifestations requiring surgery at diagnosis were associated with increased risk of death. Bourgarit et al. conclude that GI symptoms were most frequently associated with early death from HBV-PAN [6].
Although GI involvement is frequent in PAN, the isolated abdominal initial presentation is uncommon, and since 1975, only 9 cases have been published in the English language literature. They are summarized in Table 1 [7–15].
| N [Reference] | Year | Age/sex | GI symptoms | Extra GI symptoms | Finding on RS | Perforation | Surgery | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 [7] | 1979 | 76/M |
|
|
Colitis | No | Yes | D |
| 2 [8] | 1982 | 52/M | None |
|
— | No | Yes | S |
| 3 [9] | 1984 | 58/M |
|
Fever | Colitis | Yes | Yes | S |
| 4 [10] | 1991 | 28/M |
|
None | Colitis | No | Yes | S |
| 5 [11] | 1994 | 48/M |
|
|
Colitis | Yes | Yes | S |
| 6 [12] | 1994 | 78/F | Abdominal pain and bloody stool | None | — | No | Yes | — |
| 7 [13] | 1996 | 38/F |
|
|
Colitis | No | No | S |
| 8 [14] | 1999 | 60/M |
|
None | Colitis | Yes | Yes | — |
| 9 [15] | 2008 | 70/M |
|
None | Colitis | Yes | Yes | S |
| Our case | 2010 | 55/M | Abdominal pain and bloody stool |
|
Colitis | No | Yes | S |
- M: male; F: female; GI: gastrointestinal, RS: rectosigmoidoscopy; S: survived; D: died.
In the presence of acute abdominal signs, early surgery is warranted. In their absence, medical treatment should suffice. In all cases, close observation by a surgical team must be undertaken.
For many years, PAN treatment has involved administration of high-dose steroid with an additional cytotoxic agent, such as cyclophosphamide, to induce remission. In most patients, it is appropriate to treat aggressively. Once remission is achieved, maintenance therapy with daily or alternate-day low-dose prednisolone and oral azathioprine is frequently used for up to 18 months [16].
PAN, unlike some other vasculitides such as Wegener granulomatosis, appears to be a condition in which permanent remission can be achieved. Relapses can occur, but despite these, a real possibility of cure can be anticipated. However, if treatment is delayed or inadequate, life-threatening complications can occur due to the vasculitic process.
4. Conclusion
Although the gastrointestinal tract is frequently involved with PAN, it is extremely rare for PAN to be accompanied by ischemic colitis, particularly at the initial presentation.




