Retrospective evaluation of clinical signs, clinical course, and prognosis between dogs with left atrial rupture secondary to myxomatous mitral valve disease and those with neoplastic cardiac tamponade (2015–2019): 70 cases
Abstract
Objective
To describe the clinical signs, clinical course, and prognosis of suspected left atrial rupture (LAR) secondary to myxomatous mitral valve disease (MMVD) in dogs and to compare them with dogs with suspected neoplastic cardiac tamponade (NCT).
Design
Retrospective study from November 2015 to October 2019
Setting
An out-of-hours Emergency Animal Hospital.
Animals
Twenty-three dogs with LAR secondary to MMVD (LAR group) and 47 dogs with NCT (NCT group).
Interventions
None.
Measurements and Main Results
The following were the characteristics of the study population (LAR group vs NCT groups) with P < 0.05 as the significance threshold: male sex, 83% vs 66%; median age, 11.9 vs 12.5 years; and median weight, 3.8 vs 6.4 kg (P < 0.001). Chihuahuas and Miniature Dachshunds were overrepresented in the LAR and NCT groups, respectively. Statistically different clinical findings between the 2 groups were as follows (LAR vs NCT): pulmonary edema, 43% vs 0%; pericardial thrombus, 70% vs 6% (P < 0.001); ineffectiveness of pericardiocentesis (whether aspiration of pericardial fluid was successful or not), 58% vs 2% (P < 0.001); mortality rate within 48 hours of visiting hospital, 35% vs 9% (P < 0.01). No significant difference was observed in survival time after discharge between the 2 groups.
Conclusions
The proportion of dogs with a diagnosis of LAR secondary to MMVD in dogs with cardiac tamponade was higher than the previously reported rate. Furthermore, the frequency of pulmonary edema, ineffectiveness of pericardiocentesis, and short-term mortality rate was higher in the LAR group than in the NCT group.
Abbreviations
-
- LA/Ao ratio
-
- left atrium to aortic root ratio
-
- LAR
-
- left atrial rupture
-
- MMVD
-
- myxomatous mitral valve disease
-
- MST
-
- median survival time
-
- NCT
-
- neoplastic cardiac tamponade
-
- PE
-
- pericardial effusion
-
- TPP
-
- total plasma protein
1 INTRODUCTION
Pericardial effusion (PE) is an uncommon clinical findings in dogs,1 the prevalence of which has been reported to be 0.43%.2, 3 Depending on the amount and rate of accumulation of pericardial fluid and the distensibility of the pericardium, intrapericardial pressure may exceed the right atrial pressure,4 which leads to collapse of the right atrium, reduced venous return, and a decreased cardiac output. This phenomenon is known as cardiac tamponade and is a potentially life-threatening emergency condition that requires prompt intervention.1, 5
Many studies on PE disease3, 5-8 have shown that neoplastic diseases such as hemangiosarcoma, heart base tumors, and mesotheliomas are the most common causes of PE, followed by idiopathic PE. Other diseases/conditions that can lead to the accumulation of pericardial fluid include infectious pericarditis,9 systemic inflammatory diseases,10 coagulopathies (eg, coumatetralyl-induced11), foreign body migration, peritoneal pericardial diaphragmatic hernia, congestive heart failure, and trauma.12
Myxomatous mitral valve disease (MMVD) is a most common acquired heart disease in dogs,13, 14, and can often lead to decreased cardiac output15, 16 in addition to increases in mitral valve regurgitation,17 left atrial pressure, and pulmonary capillary hydrostatic pressure, which may subsequently result in cardiogenic pulmonary edema. Left atrial rupture (LAR) is a rare but significant complication of MMVD.5, 18 Jet lesions in the left atrial wall are the most common cause for LAR as the wall develops endocardial erosion at a specific site where mitral regurgitation is concentrated at a velocity of approximately 5 m/s, striking the same site approximately 100+ times/min. Although LAR associated with mitral valve disease was first described in veterinary literature in 1964,19 only a few reports have described this disease since then.18, 20 Most reports related to PE or cardiac tamponade do not mention LAR secondary to MMVD. This disease tends to be considered quite rare and clinical features are still unknown.
However, in recent years, the number of reported cases of LAR secondary to MMVD has increased,4, 21 so the frequency and characteristics of the disease should be reevaluated. In the present study, we describe the clinical signs, clinical course, and prognosis of LAR secondary to MMVD in dogs compared to dogs diagnosed with NCT during the same period.
2 MATERIALS AND METHODS
The electronic medical records database at our institution was searched for dogs diagnosed with cardiac tamponade that visited the emergency medical center during the 4-year period from November 2015 to October 2019. The diagnosis of cardiac tamponade was based on PE with collapse of the right atrium. Dogs with PE but no evidence of cardiac tamponade were excluded. Medical records of the selected dogs were carefully examined, and those with ultrasonographic data sufficient for verification were included. Subsequently, the age, sex, breed, heart disease and treatment history, clinical signs, body weight and other physical examination findings, blood test, radiographic and ultrasonographic findings, treatment, and prognosis of the selected dogs were investigated. Among them, dogs with mitral valve leaflet thickening or prolapse,13, 14 left atrium to aortic root ratio (LA/Ao ratio) of ≥1.5:1,4, 21 and severe mitral regurgitation (>50% of the atrium filled by aliased flow of regurgitation as shown by color Doppler examination21) were assigned to the group of suspected LAR secondary to MMVD (LAR group). In addition, other obvious causes of cardiac tamponade such as tumors, road traffic accidents, and rodenticide intake were exclusion criteria. Dogs that were suspected of having heart tumors, based on the findings of ultrasonography (mass lesions of the myocardium that appear to communicate directly with the pericardial cavity), were assigned to the group of suspected neoplastic cardiac tamponade (NCT group). Cases in which the presence of MMVD was suspected but a prominent cardiac mass was confirmed by ultrasonography were assigned to the NCT group. These ultrasonographic images were reassessed by a single veterinarian.
Statistical comparisons were conducted with Fisher's exact test and Mann–Whitney's U test to identify differences in sex, age, weight, breed, chief complaint/findings of physical examination, results of a blood test, radiographic and ultrasonographic findings, intervention, and short-term mortality rate. Data were shown in median and interquartile range. For the long-term prognosis survey, information was collected by the primary veterinarian via telephone, fax, and mail. Log-rank test was used to determine whether a significant difference existed between the 2 groups in the probability of survival at any time point and the Kaplan–Meier method was used to estimate the median survival time (MST). The significance level was set to 5%. Statistical analysis was performed using commercial statistical software.a
3 RESULTS
There were 108 dogs diagnosed with cardiac tamponade during the study period. Among them, 98 dogs had sufficiently verifiable ultrasonographic data to be included. Medical records were examined, and 23 and 47 dogs were assigned to the LAR and the NCT groups, respectively. Three dogs of the NCT group were suspected of having MMVD but they were assigned to the NCT group because a prominent cardiac mass was confirmed and apparent left atrial enlargement was not evident on ultrasonography. In the NCT group, suspected tumors were identified in the following regions: the right atrium, 43 (91%); heart base, 2 (4%); and left atrium and right ventricle, 1 each (2%). Twenty-eight of the 98 dogs were excluded because they did not meet the defined inclusion criteria (ie, there was no mitral regurgitation or enlargement of the left atrium, and no obvious cardiac mass).
The following were the patient characteristics (LAR vs NCT): male sex, 19 (83%) vs 31 (66%; P = 0.082); median age, 11.9 years (10.9–13.1 years) vs 12.5 years (10.5–13.7 years; P = 0.666); median body weight, 3.8 kg (3.0–5.0 kg) vs 6.4 kg (5.2–12.2 kg; P < 0.001). In the LAR group, Chihuahuas were most commonly affected (12 dogs; 52%); in addition, there were 3 Pomeranians and other breeds were 2 or less. In the NCT group, Miniature Dachshunds were most commonly affected (16 dogs; 34%); in addition, there were 5 Toy Poodles, 4 Golden Retrievers, 3 mongrels, and other breeds were 2 or less.
In the LAR group, the median LA/Ao ratio was 2.18 (1.67–3.17). In the NCT group, the LA/Ao ratio was measured in 32 cases (68%) from the stored ultrasound images and the median was 1.12 (0.98–1.24), which was significantly smaller than the LAR group (P < 0.001). In the remaining 15 dogs of the NCT group, the LA/Ao ratio could not be accurately measured due to the insufficient quality of the recorded images, although left atrial enlargement was not evident apparently. Twenty-two (96%) and 2 (4%) dogs had a history of mitral valve disease in the LAR and NCT groups, respectively. In the LAR group, data on medication prescribed for heart disease was available for 21 dogs, 16 (76%), 10 (48%), and 5 (24%) of whom had been prescribed angiotensin-converting enzyme inhibitors, pimobendan, and loop diuretics, respectively.
The chief complaints and findings of physical examination of both the groups are summarized in Table 1. In both groups, acute collapse, altered mentation, and pale/cold oral mucosa were the most common presenting signs. Heart murmur and tachypnea/dyspnea were significantly more common in the LAR group. Jugular vein distension and muffled heart sounds were not so common in the present study. One dog in the LAR group presented with knuckling of the right forelimb and this dog was diagnosed with concurrent thromboembolism of the right forelimb artery.
| LAR group | NCT group | ||||
|---|---|---|---|---|---|
| Chief complaint/physical examination findings | n | % | n | % | P-value |
| Altered mentation | 17 | 74 | 27 | 57 | 0.088 |
| Heart murmur | 16 | 70 | 2 | 4 | <0.001 |
| Acute collapse | 15 | 71 | 27 | 57 | 0.171 |
| Pale/cold oral mucosa | 15 | 71 | 38 | 81 | 0.085 |
| Tachypnea/dyspnea | 14 | 61 | 13 | 28 | 0.006 |
| Difficulty standing/wobble | 12 | 52 | 19 | 40 | 0.132 |
| Cyanosis | 5 | 22 | 1 | 2 | 0.012 |
| Dullness | 4 | 17 | 19 | 40 | 0.034 |
| Muffled heart sound | 4 | 17 | 15 | 32 | 0.105 |
| Anorexia | 2 | 9 | 6 | 13 | 0.288 |
| Cough | 2 | 9 | 0 | 0 | 0.105 |
| Salivation | 2 | 9 | 2 | 4 | 0.298 |
| Incontinence | 2 | 9 | 3 | 6 | 0.339 |
| Vomiting | 1 | 4 | 6 | 13 | 0.206 |
| Diarrhea | 1 | 4 | 0 | 0 | 0.329 |
| Knuckling of the forelimb | 1 | 4 | 0 | 0 | 0.329 |
| Seizure | 1 | 4 | 0 | 0 | 0.329 |
| Delirium | 1 | 4 | 0 | 0 | 0.329 |
| Jugular vein distension | 1 | 4 | 1 | 2 | 0.448 |
| Behavioral abnormalities | 0 | 0 | 2 | 4 | 0.448 |
| Hematochezia | 0 | 0 | 1 | 2 | 0.671 |
| Tremor | 0 | 0 | 1 | 2 | 0.671 |
- Note: Items shown in gray are significantly different (P < 0.05) between the 2 groups.
- Abbreviations: LAR, left atrial rupture; NCT, neoplastic cardiac tamponade.
There was no difference in temperature, pulse, and respiration (TPR) between the 2 groups. Comparing clinicopathological findings, blood glucose concentrations were significantly higher, and total plasma protein (TPP), albumin, and total cholesterol concentrations were significantly lower in the LAR group than in the NCT group. The median plasma lactate concentration was significantly increased compared with reference value in both groups (Table 2).
| LAR group | NCT group | |||||||
|---|---|---|---|---|---|---|---|---|
| Measured items | Reference value | Median | Q1 | Q3 | Median | Q1 | Q3 | P-value |
| Age (years) | 11.9 | 10.9 | 13.1 | 12.6 | 10.5 | 13.7 | 0.666 | |
| Body weight (kg) | 3.8 | 3.0 | 5.0 | 6.4 | 5.2 | 12.2 | <0.001 | |
| Body temperature (°C) | 37.5 | 36.8 | 38.1 | 37.6 | 37.2 | 39.8 | 0.379 | |
| Heart rate (/min) | 140 | 108 | 160 | 145 | 120 | 240 | 0.442 | |
| Respiratory rate (/min) | 57 | 36 | 60 | 40 | 30 | 120 | 0.117 | |
| LA/Ao ratio | 2.18 | 1.67 | 3.17 | 1.12 | 0.98 | 1.24 | <0.001 | |
| PCV (%) | 42–55 | 42 | 38 | 44 | 43 | 37 | 65 | 0.699 |
| WBC (×100/μl) | 60–120 | 142 | 83 | 174 | 132 | 109 | 337 | 0.457 |
| PLT (×104/μl) | 25–50 | 28.0 | 20.2 | 38.0 | 20.9 | 13.1 | 63.0 | 0.066 |
| TPP (g/dl) | 5.0–7.2 | 5.1 | 4.8 | 5.6 | 5.8 | 5.1 | 8.4 | 0.005 |
| BUN (mg/dl) | 9.2–29.2 | 31.8 | 27.0 | 43.8 | 27.5 | 20.6 | 76.9 | 0.107 |
| Cre (mg/dl) | 0.4–1.4 | 1.2 | 0.8 | 1.3 | 1.0 | 0.8 | 4.3 | 0.707 |
| TCHO (mg/dl) | 111–312 | 133 | 118 | 164 | 169 | 124 | 450 | 0.025 |
| Glu (mg/dl) | 75–128 | 293 | 167 | 451 | 118 | 95 | 352 | <0.001 |
| ALT (U/L) | 17–44 | 145 | 83 | 297 | 85 | 54 | 1000 | 0.056 |
| AST (U/L) | 17–78 | 109 | 69 | 262 | 65 | 37 | 1000 | 0.062 |
| ALP (U/L) | 47–254 | 163 | 97 | 557 | 189 | 136 | 3500 | 0.5 |
| ALB (g/dl) | 2.6–4.0 | 2.3 | 2.1 | 2.7 | 2.7 | 2.4 | 3.5 | 0.011 |
| Ca (mg/dl) | 9.3–12.1 | 9.7 | 9.1 | 10.5 | 10.0 | 9.5 | 12.8 | 0.402 |
| Bil (mg/dl) | –0.5 | 0.2 | 0.1 | 0.3 | 0.2 | 0.1 | 1 | 1 |
| Na (mmol/L) | 141–152 | 146 | 145 | 148 | 147 | 144 | 152 | 0.753 |
| K (mmol/L) | 3.8–5.0 | 4.1 | 3.8 | 4.3 | 4.0 | 3.8 | 5.4 | 0.995 |
| Cl (mmol/L) | 102–117 | 107 | 104 | 111 | 110 | 107 | 113 | 0.073 |
| CRP (mg/dl) | 0–1.0 | 0.4 | 0 | 1.6 | 0.9 | 0.2 | 5.1 | 0.067 |
| Lact (mmol/L) | 0.5–2.0 | 10.4 | 6.2 | 13.8 | 6.0 | 4.2 | 9.8 | 0.077 |
- Note: Items shown in gray are significantly different (P < 0.05) between the 2 groups. Q1 represents the first quartile and Q3 represents the third quartile.
- Abbreviations: LAR, left atrial rupture; NCT, neoplastic cardiac tamponade; LA/Ao ratio, left atrium to aortic root ratio; PCV, packed cell volume; WBC, white blood cell; TPP, total plasma protein; BUN, blood uria nitrogen; ALT, alanin aminotransferase; AST, aspartete aminotransferase; ALP, alkaline phospatase; CRP, C reactive protein.
On the basis of an evaluation of ultrasonography images, pericardial thrombus (defined as a homogeneous structure that was more echogenic than the myocardium located within the pericardial cavity) was suspected in a higher number of dogs in the LAR group (16 dogs; 70%) than in the NCT group (3 dogs; 6%; P < 0.001). Pericardiocentesis was attempted in 19 (83%) of the LAR group, but in 11 of them (58%), aspiration of pericardial fluid was not effective owing to the presence of pericardial thrombus. In the NCT group, this procedure was performed in 42 dogs (89%), but it was ineffective in only 1 dog (2%). There was a significant difference in the effectiveness of pericardiocentesis (whether aspiration of pericardial fluid was successful or not) between the 2 groups (P < 0.001).
On the basis of radiography, 10 (43%) dogs in the LAR group were diagnosed with cardiogenic pulmonary edema at the time of visit or during hospitalization, and 17 (74%) dogs were administered furosemide during treatment. None of the dogs in the NCT group had pulmonary edema (P < 0.001), and none of them were administered furosemide (P < 0.001). In the LAR group, 9 (39%) and 8 (35%) dogs were treated with pimobendan and dobutamine, respectively, but none of the dogs in the NCT group were administered these drugs. The lactated Ringer's solution was administered to 15 (65%) and 41 (87%) dogs in the LAR and NCT groups, respectively, and a significant difference was observed between the 2 groups (P = 0.027). Only 1 dog in the LAR group and 2 dogs in the NCT group were administered colloidal fluid.
One dog in the LAR group was diagnosed with arterial thromboembolism of the right forelimb associated with LAR, and when Monteplase, a tissue plasminogen activator (tPA), was administered, worsening of cardiac tamponade was observed immediately afterward. However, improvement in the signs of embolization of the right forelimb artery was observed several hours later.
The number of dogs that died within 48 hours after visiting a hospital was significantly higher in the LAR group (8 dogs, 35%) than in the NCT group (4 dogs, 9%; P < 0.01). It was possible to follow up to the deaths of 17 in the LAR group and 22 in the NCT group. The Kaplan–Meier survival curves are shown in Figure 1. MSTs were 26 days (0–820 days) in the LAR group and 44 days (0–445 days) in the NCT group. There was no statistically significant difference between the 2 groups (P = 0.824).
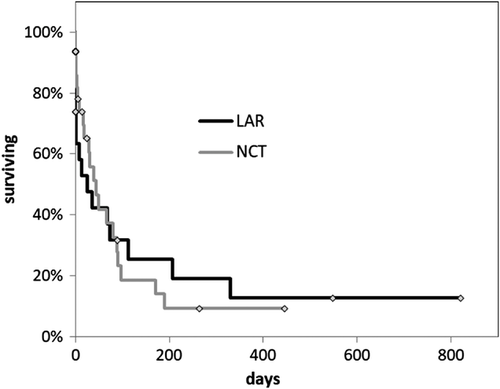
One of the dogs in the LAR group that survived underwent chordae tendineae reconstruction surgery and survived for a long time. The MST of the LAR group excluding this dog was 26 days (0–548 days), and even in this case, there was no significant difference in survival time between the 2 groups.
4 DISCUSSION
In the present study, we describe the clinical signs, course of treatment, and prognosis of 23 dogs with LAR secondary to MMVD and compared them with those of dogs diagnosed with NCT during the same period. LAR is documented as a rare cause of PE or cardiac tamponade in dogs; however, in the present study, among the 98 dogs diagnosed with cardiac tamponade 23 dogs were diagnosed with LAR secondary to MMVD. It has been hypothesized that the causes of cardiac tamponade in dogs are mainly neoplastic diseases followed by idiopathic disease3, 5-8; however, considering the results of the present study, LAR secondary to MMVD should be added to the differential diagnosis as one of the typical causes of cardiac tamponade.
LAR secondary to mitral valve disease was first described in a report published in 1964; in that study, necropsy of 22 dogs with mitral valve disease confirmed a split in the left atrial endocardium.19 A necropsy-based study conducted in 1972 on 30 dogs with chronic mitral valve disease revealed the occurrence of ruptured left atrium wall.20 Information on LAR has not been significantly updated since the 2 studies cited here were published, and most reports related to PE or cardiac tamponade do not even mention LAR secondary to MMVD.
In recent years, 2 case series, 1 conducted in 2008 with 14 dogs4 and another conducted in 2014 with 11 dogs,21 have provided detailed information about the disease. These 2 case series also used similar diagnostic criteria. The criteria were as follows: the presence of (1) mitral valve regurgitation, (2) LA/Ao ratio of at least 1.5:1, (3) PE, and (4) a soft tissue lesion consistent with a pericardial thrombus as visualized in the pericardial cavity near the left atrium by ultrasonography. In addition to the above 4 criteria, the latter study18 added another criterion: the presence of a mitral regurgitation signal occupying ≥50% of the left atrium on color Doppler echo. In the present study, the diagnosis of LAR was based on the criteria described in the abovementioned studies, except the presence of pericardial thrombus. The presence of pericardial thrombus may be one of the useful identifiers of LAR, but in the present study, the incidence of pericardial thrombus of the LAR group was 70%. Among the remaining dogs, there were 2 dogs in which the pericardial fluid could not be drained, probably due to the coagulation of the pericardial fluid, even though ultrasonography did not detect an obvious pericardial thrombus. This supports the hypothesis that a pericardial thrombus may not always be visualized by ultrasonography.
Though it seems sensible to speculate that in LAR, pericardial thrombus is more likely to form due to erosion of the left atrial endocardium and the turbulent blood flow, the formation and dissolution of a blood clot is dynamic, and depending on the time elapsed since the onset of bleeding and the degree of coagulation, no pericardial thrombus may be seen. Therefore, we do not consider the presence of pericardial thrombus on ultrasonography to be an essential criterion for LAR.
Confirmation that the pericardial fluid is blood by pericardiocentesis was not required as a diagnostic criterion in either previous studies or the present study. It is known that the congestion associated with right heart failure causes PE,5 which is not generally characterized by bleeding but by transudate, and for strict confirmation, pericardiocentesis must be performed to determine whether the fluid in the pericardial cavity is bleeding caused by LAR. On the contrary, in LAR, unlike PE due to right heart failure, it is conceivable that intrapericardial pressure exceeds the right heart pressure in a short time owing to acute pericardial fluid accumulation, causing cardiac tamponade. Therefore, in the present study, we adopted the condition that cardiac tamponade occurs as the selection criterion for cases. It is possible that LAR causes PE without cardiac tamponade, but they were excluded because they do not meet the inclusion criteria in the present study.
In the present study, there was a male predominance observed in both LAR and NCT groups, which is consistent with the findings of previous studies.4, 7, 8, 19, 20 There was no age difference between the 2 groups. The weight difference between the 2 groups was remarkable, and the LAR group was dominated by small breeds, mainly Chihuahuas. In the geographical area of this study, there are a large number of small-breed dogs, such as Chihuahuas, which are prone to developing MMVD or cardiogenic pulmonary edema.22 Therefore, it was not unexpected that many of the dogs in the LAR group were small breeds.
Comparing the chief complaint and physical examination findings, heart murmur, tachypnea/dyspnea, and cyanosis were significantly more common in the LAR group, which may be related to the higher number of cases with cardiogenic pulmonary edema in the LAR group. Well-known traditional physical examination findings of cardiac tamponade such as jugular vein distension and muffled heart sounds were not so common in the present study. However, the frequency of these signs in the present study is by no means low when compared to previous reports.1, 8, 21 With reference to previous studies, muffled heart sounds are more likely to be present in NCT8 and less likely to be present in LAR21 and this tendency is consistent with what was observed in the present study. Though it is not clear how this tendency occurs, severe cardiac enlargement or strong heart murmur may make it difficult to recognize muffled heart sound.
One of the dogs in the LAR group showed knuckling of the right forelimb at the time of the visit. The right forelimb was clearly cold, and as a result of comparing the blood glucose concentrations of both forelimbs, the blood glucose concentration of the right forelimb was markedly lower, and arterial thromboembolism of the right forelimb was strongly suspected.23 One study reported a dog with a split in the left atrial wall, myocardial infarction, and arterial embolism in the right forelimb.24 In this case report, it was presumed that thrombus formation was promoted by damage to the left atrial wall and turbulent blood flow. It is considered that a similar phenomenon occurred in a case in the present study.
Blood tests conducted at the time of visit revealed high plasma lactate concentrations in both groups, which is considered to reflect the pathophysiology of circulatory insufficiency well. Blood glucose concentrations were significantly higher, and TPP and albumin concentrations were significantly lower in the LAR group than in the NCT group. Hyperglycemia may suggest that the degree of shock was greater in the LAR group. It has been shown that hypoalbuminemia can be associated with cachexia and worsened prognosis in dogs with heart failure,25 but the association with lower serum TPP and albumin in the LAR group in the present study is unclear. It is noteworthy that these blood test results in the LAR group, such as hyperlactatemia, hyperglycemia, and hypoproteinemia, appear to be relatively similar to the previously reported results.4
Among the 23 dogs in the LAR group, 10 (43%) were diagnosed with cardiogenic pulmonary edema at the time of visit or during inpatient treatment. It is speculated that the left atrial pressure should have decreased temporarily in the case of occurrence of LAR; however, in the present study, the recording of the flow velocity of the mitral valve regurgitation and the left ventricular inflow wave was insufficient, and it is difficult to verify the left atrial pressure at the time of the LAR. Furosemide was administered not only to dogs that developed cardiogenic pulmonary edema but also to those that did not (a total of 17 dogs, 74%). However, it is controversial to administer furosemide to cases with unknown causes of pulmonary edema. Diuretics may cause more harm, especially in cases of hypotension. On the contrary, in the LAR group, 15 dogs (65%) were administered lactated Ringer's solution, and 1 dog was administered colloidal fluid for the signs of shock, but increase in hydrostatic pressure in the pulmonary circulation due to intravenous infusion may cause pulmonary edema. Administration of diuretics and intravenous infusion should be cautiously determined according to condition of each case in LAR.
Pericardiocentesis is the mainstay of emergency treatment for cardiac tamponade. In the present study, pericardiocentesis was attempted in 42 dogs (89%) in the NCT group, and only 1 of these attempts appeared to be ineffective because of pericardial thrombus. In the NCT group, only 3 dogs (6.4%) were suspected of pericardial thrombus as shown by ultrasonographic images, whereas in the LAR group, 16 dogs (70%) were suspected of having pericardial thrombus. Pericardiocentesis was attempted in 19 (83%) dogs in the LAR group, but effective pericardiocentesis was not performed in 11 of them (58%). The high rate of pericardial thrombus in the LAR group is a major obstacle to effective pericardiocentesis and may be one of the reasons why aggressive fluid therapy had been performed early to improve circulatory insufficiency. However, in patients with cardiac tamponade caused by LAR secondary to MMVD, it must be taken into account that aggressive intravenous infusion to improve circulatory insufficiency may increase preload and exacerbate congestive heart failure.
In the present study, the number of deaths that occurred within 48 hours after attending the hospital was significantly higher in the LAR group (8 dogs, 35%) than in the NCT group (4 dogs, 9%). High mortality may be related to the fact that in many cases, pericardiocentesis was not performed effectively in the LAR group and that many cases were accompanied by cardiogenic pulmonary edema. On the contrary, the long-term prognosis was not significantly different between the 2 groups (MST: LAR vs NCT = 26 days vs 44 days).
One study reported that 9 of 14 LAR were not discharged and 3 of the remaining dogs died within 35 days,4 while another study reported that 10 of 11 LAR dogs discharged and MST was 203 days.21 Though the prognosis of the LAR group in the present study appears to be relatively better than that in the former study, they should be cautiously compared because in the former study4 there were more euthanasia cases and deaths upon arrival at the hospital. In the latter study21 that showed better prognosis than the former study (and the present study), it is mentioned that the use of pimobendan might have improved prognosis. Different prognosis among studies might be due to the different treatment or other factors such as study population.
4.1 Limitations
There are several limitations to the present study. First, in the LAR group, there were no cases in which LAR was visually confirmed by surgical intervention or necropsy, and no pathological support was obtained for the diagnosis. In addition, as mentioned above, the diagnostic criteria that were defined on the basis of ultrasonography and adopted in the present study do not favor the inclusion of LAR and NCT dogs that have PE without cardiac tamponade. Furthermore, it is possible that cases of NCT with MMVD were assigned to the LAR group as some masses causing cardiac tamponade may not have been identified on the first occasion.3 It is also a limitation that LA/Ao ratio measured in the NCT group may lack accuracy because there were not ideal images left in one third of the group. So, the possibility cannot be excluded that a part of the NCT group had severe MMVD and should be assigned to the LAR group. However, because dogs in the NCT group did not show apparent left atrial enlargement at the time of visit, it is possible that clinicians were not prompted to measure LA/Ao ratio. In the present study, pericardial thrombus was not adopted as a diagnostic criterion for LAR, and the proportion of suspected presence of pericardial thrombus was 70% in the LAR group. Considering these points, caution is required in comparing this study with previous studies. Further investigation will be necessary to establish the diagnostic criteria based on pathological findings. Finally, especially in the NCT group, there were many cases that had not been followed up from the beginning, so cautious interpretation may be required about the long-term prognosis.
5 CONCLUSIONS
LAR secondary to MMVD is generally considered to be a rare disease, but in the present study, LAR accounted for 23% of dogs of cardiac tamponade (23/98), which is higher than the previously recognized diagnosis rate. We suggest that LAR should not be considered as a rare cause of cardiac tamponade in dogs. Compared with NCT cases, in the LAR cases, there were more small breeds, more cases with pulmonary edema, pericardiocentesis was more ineffective due to pericardial thrombus, and short-term mortality rate was higher.
ACKNOWLEDGMENTS
The authors would like to thank Editage (www.editage.com) for English language editing of this manuscript.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
DISCLAIMERS
The views expressed in the submitted manuscript are author specific and do not represent the official position of the institution.