Preliminary evaluation of a commercial shampoo and fine bubble bathing in the treatment of canine atopic dermatitis: A single-blinded, randomised, controlled study
Abstract
enBackground
Fine bubble (FB) bathing has shown benefits on a mouse model of atopic dermatitis (AD). However, its efficacy in dogs with AD remains to be evaluated.
Objective
This study aimed to assess the clinical effectiveness of FB bathing in dogs with AD.
Animals
Seventeen dogs with AD whose clinical presentation showed a Canine Atopic Dermatitis Extent and Severity Index, 4th iteration (CADESI-04) score of <40.
Materials and Methods
The dogs were randomly assigned to either the FB bathing group or the shampoo group. The treatments were administered once a week as per the instructions, in a trial totalling 4 weeks. Evaluations were conducted on Day (D)0 and D28 to assess the outcomes of the trial. The severity of AD was measured using the CADESI-04 and the pruritus Visual Analog Scale (PVAS). The skin barrier function parameters, transepidermal water loss (TEWL) and stratum corneum hydration were measured before and after the treatment.
Results
Both treatment groups demonstrated a decreasing trend in CADESI-04 scores, yet the FB group exhibited significant improvement in comparison to the shampoo group after 1 month of trial. There were no significant changes in PVAS scores in either group. No significant difference was found in skin barrier function parameters between the two treatments, although TEWL slightly decreased in the FB group and slightly increased in the shampoo group after treatment.
Conclusions and Clinical Relevance
These results suggested that FB treatment provides benefits for dogs with AD and offers an alternative topical treatment option with a lesser impact on skin barrier function compared to frequent shampooing.
Zusammenfassung
deHintergrund
Es hat sich gezeigt, dass sich ein Bad mit feinen Luftblasen (FB) bei einem Mausmodell mit atopischer Dermatitis (AD) günstig auswirkt. Seine Wirksamkeit bei Hunden mit AD muss jedoch noch evaluiert werden.
Ziel
Diese Studie erfasste die klinische Wirksamkeit von FB-Bädern bei Hunden mit AD.
Tiere
Siebzehn Hunde mit AD, deren klinische Präsentation einen Canine Atopic Dermatitis Extent und Severity Index, 4th Auflage (CADESI-04) Wert von < 40 zeigte.
Material und Methoden
Die Hunde wurden zufällig entweder in die FB-Badegruppe oder in die Shampoo-Gruppe eingeteilt. Die Behandlungen wurden nach entsprechender Anleitung einmal wöchentlich durchgeführt; das Ganze war als Versuch, der 4 Wochen dauerte, angelegt. Evaluierungen wurden am Tag (D) 0 und am D28 durchgeführt, um das Ergebnis des Versuchs zu erfassen. Der Schweregrad der AD wurde mittels CADESI-04 und der Pruritus Visual Analog Scale (PVAS) gemessen. Parameter der Funktion der Hautbarriere, nämlich der transepidermale Wasserverlust (TEWL) und die Hydrierung des Stratum corneum (SSH) wurden vor und nach der Behandlung gemessen.
Ergebnisse
Beide Behandlungsgruppen zeigten einen abnehmenden Trend der CADESI-04 Werte, wobei allerdings die FB-Gruppe im Vergleich zur Shampoo-Gruppe nach 1 Monat des Versuchs eine signifikante Verbesserung zeigte. Es gab bei keiner der beiden Gruppen signifikante Änderungen der PVAS-Werte. Bei den Hautfunktionsparametern wurde keine signifikante Veränderung zwischen den beiden Behandlungen gefunden, obwohl der TEWL in der FB-Gruppe geringfügig weniger wurde und in der Shampoo-Gruppe nach der Behandlung geringfügig zunahm.
Schlussfolgerungen und klinische Bedeutung
Diese Ergebnisse weisen darauf hin, dass sich die FB-Behandlung für Hunde mit AD günstig auswirkt und eine Alternative für die topische Behandlung mit einem geringeren Einfluss auf die Funktion der Hautbarriere im Vergleich zu häufigem Shampoonieren darstellt.
摘要
zh背景
细泡(FB)浴对特应性皮炎(AD)小鼠模型显示出益处。然而,它对患有AD的犬的疗效仍有待评估。
目的
本研究旨在评估FB沐浴治疗AD犬的临床效果。
动物
17只AD患犬,其临床表现为犬特应性皮炎程度和严重程度指数,第4次迭代(CADESI-04)得分<40。
材料和方法
将犬随机分为FB浴组或香波组。在总共4周的试验中,根据说明书每周进行一次治疗。在第(D)0天和第D28天进行评估,以评估试验的结果。使用CADESI-04和瘙痒视觉模拟量表(PVAS)测量AD的严重程度。测量治疗前后皮肤屏障功能参数,经表皮失水量(TEWL)和角质层水合程度(SSH)。
结果
两个治疗组的CADESI-04评分均呈下降趋势,但试验1个月后,FB组与香波组相比有显著改善。两组PVAS评分均无显著变化。两个处理之间的皮肤屏障功能参数没有显著差异,尽管治疗后FB组的TEWL略有下降,香波组的TEWL略有增加。
结论和临床相关性
这些结果表明,FB治疗为AD患犬提供了益处,并提供了一种替代的外部治疗选择,与频繁香波相比,对皮肤屏障功能的影响较小。
Résumé
frContexte
Le bain à fines bulles (BF) a montré ses avantages sur un modèle murin de dermatite atopique (DA). Cependant, son efficacité chez les chiens atteints de dermatite atopique n'a pas encore été évaluée.
Objectif
Cette étude vise à évaluer l'efficacité clinique du bain à fines bulles chez les chiens atteints de dermatite atopique.
Animaux
Dix-sept chiens atteints de DA présentant cliniquement un score CADESI-04 <40 (Canine Atopic Dermatitis Extent and Severity Index, 4th iteration).
Matériels et méthodes
Les chiens ont été assignés au hasard soit au groupe bain à FB, soit au groupe shampoing. Les traitements sont réalisés une fois par semaine, conformément aux instructions, dans le cadre d'un essai d'une durée totale de 4 semaines. Des évaluations sont réalisées au jour (J)0 et au jour (J)28 pour évaluer les résultats de l'essai. La sévérité de la DA est mesurée à l'aide de l'échelle CADESI-04 et de l'échelle visuelle analogique du prurit (PVAS). Les paramètres de la fonction de barrière cutanée, la perte d'eau transépidermique (TEWL) et l'hydratation de la couche cornée (SSH), ont été mesurés avant et après le traitement.
Résultats
Les deux groupes de traitement montrent une tendance à la baisse des scores CADESI-04, mais le groupe FB présente une amélioration significative par rapport au groupe shampoing après 1 mois d'essai. Aucune différence significative n'est mise en évidence dans les paramètres de la fonction de barrière cutanée entre les deux traitements, bien que le TEWL diminue légèrement dans le groupe FB et augmente légèrement dans le groupe shampooing après le traitement.
Conclusions et pertinence clinique
Ces résultats suggèrent que le traitement FB est bénéfique pour les chiens atteints de DA et qu'il constitue une option de traitement topique alternative avec un impact moindre sur la fonction de barrière cutanée par rapport aux shampooings fréquents.
要約
ja背景
ファインバブル(FB)入浴は、アトピー性皮膚炎(AD)モデルマウスに有効であることが示されている。しかし、犬のアトピー性皮膚炎モデルにおけるFB入浴の有効性はまだ評価されていない。
目的
本研究は、ADの犬におけるFB入浴の臨床的有効性を評価することを目的とした。
対象動物
犬アトピー性皮膚炎重症度指数第4版(CADESI-04)のスコアが40未満であった17頭のAD犬。
材料と方法
犬をFB入浴群およびシャンプー群に無作為に割り付けた。治療は週1回、説明書に従って、合計4週間にわたって行われた。試験の結果を評価するため、0日目と28日目に評価を行った。ADの重症度はCADESI-04および掻痒の視覚的アナログスケール(PVAS)を用いて測定した。皮膚バリア機能パラメータである経皮水分蒸散量(TEWL)および角層水分量(SSH)は、治療前後に測定した。
結果
両治療群ともCADESI-04スコアは減少傾向を示したが、FB群はシャンプー群に比べ、試験開始1ヵ月後に有意な改善を示した。両群ともPVASスコアに有意な変化はみられなかった。TEWLは治療後、FB群でわずかに減少し、シャンプー群でわずかに増加したが、皮膚バリア機能パラメーターには両治療間で有意な差はみられなかった。
結論と臨床的意義
これらの結果から、FB治療はAD犬にとって有益であり、頻繁なシャンプーと比較して皮膚バリア機能への影響が少ない代替的な局所治療の選択肢を提供することが示唆された。
Resumo
ptContexto
O banho com bolhas finas (BF) mostrou benefícios em um modelo de camundongo para dermatite atópica (DA). Entretanto, a sua eficácia em cães com DA ainda precisa ser avaliada.
Objetivo
Este estudo teve como objetivo avaliar a eficácia do banho de BF em cães com DA.
Animais
Dezessete cães com DA cuja apresentação clínica apresentou pontuação <40 no Índice de Extensão e Gravidade da Dermatite Atópica Canina, 4ª iteração (CADESI-04).
Materiais e Métodos
Os cães foram devididos aleatoriamente entre o grupo de banho com BF ou o grupo de shampoo. Os tratamentos foram administrados uma vez por semana conforme instruções, em um ensaio de 4 semanas. As avaliações foram realizadas no Dia (D)0 e D28 para avaliar os resultados do ensaio. A gravidade da DA foi mensurada utilizando o CADESI-04 e a Escala Visual Analógica de prurido (PVAS). Os parâmetros de função da barreira cutânea, perda de água transepidérmica (TEWL) e hidratação do estrato córneo (SSH), foram mensurados antes e após o tratamento.
Resultados
Ambos os grupos de tratamento demonstraram uma tendência decrescente nas pontuações CADESI-04, mas o grupo BF exibiu uma melhora significativa em comparação com o grupo shampoo após um mês de ensaio. Não houve alterações significativas nos escores do PVAS em nenhum dos grupos. Nenhuma diferença significativa foi encontrada nos parâmetros da função de barreira da pele entre os dois tratamentos, embora a TEWL tenha diminuído ligeiramente no grupo BF e aumentado ligeiramente no grupo shampoo após o tratamento.
Conclusões e relevância clínica
Estes resultados sugerem que o tratamento com FB proporciona benefícios para cães com DA e oferece uma opção alternativa de tratamento tópico com menor impacto na função de barreira da pele em comparação com a lavagem frequente.
Resumen
esIntroducción
El baño de burbujas finas (FB) ha demostrado beneficios en un modelo de ratón con dermatitis atópica (AD). Sin embargo, aún queda por evaluar su eficacia en perros con AD.
Objetivo
Este estudio tuvo como objetivo evaluar la eficacia clínica del baño FB en perros con AD.
Animales
Diecisiete perros con AD cuya presentación clínica mostró un índice de extensión y gravedad de la dermatitis atópica canina, cuarta revisión (CADESI-04) con una puntuación <40.
Materiales y métodos
Los perros fueron asignados aleatoriamente al grupo de baño FB o al grupo de champú. Los tratamientos se administraron una vez por semana según las instrucciones, en un ensayo que duró 4 semanas. Las evaluaciones se realizaron el día (D) 0 y D28 para evaluar los resultados del ensayo. La gravedad de la AD se midió mediante el CADESI-04 y la Escala Visual análoga de prurito (PVAS). Los parámetros de la función de barrera cutánea, la pérdida transepidérmica de agua (TEWL) y la hidratación del estrato córneo (SSH), se midieron antes y después del tratamiento.
Resultados
Ambos grupos de tratamiento demostraron una tendencia decreciente en las puntuaciones de CADESI-04, sin embargo, el grupo FB mostró una mejora significativa en comparación con el grupo de champú después de 1 mes de prueba. No hubo cambios significativos en las puntuaciones PVAS en ninguno de los grupos. No se encontraron diferencias significativas en los parámetros de la función de la barrera cutánea entre los dos tratamientos, aunque la TEWL disminuyó ligeramente en el grupo FB y aumentó ligeramente en el grupo de champú después del tratamiento.
Conclusiones y relevancia clínica
Estos resultados sugieren que el tratamiento con FB es beneficioso para perros con AD y ofrece una opción de tratamiento tópico alternativo con un menor impacto en la función de la barrera cutánea en comparación con el lavado frecuente con champú.
INTRODUCTION
Canine atopic dermatitis (cAD) is a chronic skin disease characterised by pruritus and inflammation, often associated with elevated levels of immunoglobulin (Ig)E in response to environmental allergens. The condition is further deteriorated by skin barrier function defects and imbalanced microbial flora.1 All of these factors could lead to secondary bacterial infection and/or Malassezia overgrowth. To address cAD, the 2015 treatment guidelines from the International Committee on Allergic Diseases of Animals (ICADA) recommend various topical therapies.2 The aim of these treatment strategies is to target two separate facets of cAD management. First, in cases without apparent infections, the recommendations focus on improving skin barrier function and hygiene. This includes initial options such as applying spot-on essential fatty acids or topical lipid complexes containing ceramides, cholesterol and EFAs, as well as nonirritating shampoos. Secondly, when dealing with secondary bacterial or yeast infections, it is crucial to emphasise the use of gentle, low-irritant antimicrobial shampoos on a weekly basis to restore microbial balance.2 This approach serves to reduce the excessive use of systemic antimicrobials, and its effectiveness has been substantiated through several well-executed clinical trials.2
However, it is important to note that topical antimicrobials, especially shampoos, have the potential to induce atopic dermatitis (AD) flare-ups, and treatment should be tailored to each patient.
While the significance of skin hygiene care in managing cAD is widely recognised, there remains a limited range of available options.2 Treatment guidelines mention only two specific shampoo products: Allermyl (Virbac) and DOUXO Calm (Ceva Sante Animale).3, 4 Nondrug shampoos containing phytosphingosine or ophytrium-based shampoos have shown positive results in clinical evaluations.4, 5 Therefore, there is a need to explore new bathing methods for cAD treatment and their efficacy and impact on skin barrier function parameters. Loflath et al. found that the use of ascending bubbles in a whirlpool can effectively lift the hairs, resulting in a more thorough cleansing of the skin surface by removing or diluting dirt, debris and inflammatory mediators. Additionally, this process helps to hydrate the stratum corneum.6 A newly developed technological device has the capability to generate fine bubbles (FB), which are defined as bubbles with sizes <100 μm. These FB are divided into ultrafine bubbles (UFB, <1 μm) and microbubbles (MB, 1–100 μm). They are prepared in an FB generator by passing the fluid through its honeycomb structure in a gas–liquid mixer under pressure, creating air-containing FB water. The FB water has been confirmed to possess a potent bactericidal effect on Pseudomonas aeruginosa.7 In addition, research demonstrated the beneficial effects of UFB shower on a mouse model of AD.8
Skin barrier dysfunction plays a role in the development of AD, with transepidermal water loss (TEWL) and stratum corneum hydration (SSH) serving as key parameters to assess epidermal function in atopic dogs. Numerous studies have showcased increased TEWL and reduced SH in atopic dogs as a result of lower ceramide distribution.9-11 The objective of this study was to assess the clinical effectiveness of FB therapy compared to the low-irritant shampoo method in dogs with AD. The evaluation included measurements of SSH and TEWL to assess skin barrier function. Furthermore, clinical improvements were recorded using Canine Atopic Dermatitis Extent and Severity Index, 4th iteration (CADESI-04)and a pruritus Visual Analog Scale (PVAS) before and after the treatment.
MATERIALS AND METHODS
Case selection
The diagnosis of cAD was made using set 1 criterion proposed by Favrot et al., while also considering the patient's compatible history, ruling out ectoparasites and other pruritic dermatoses, all in accordance with standard guidelines.12, 13 Screening tests consisted of Wood's lamp examination, multiple trichograms, skin scrapings to rule out ectoparasites and cytological evaluation to screen for microbial infection. Each dog should have been presented with a CADESI-04 score ≥ 10 and PVAS score ≥2.14, 15 The exclusion criteria included individuals with severe internal or neoplastic diseases, pregnant or lactating individuals, individuals younger than 3 months, individuals on which antibiotics or antifungal agents had been used 1 month before the start of the trial or during the trial period, individuals who had changes in the dosage or usage of pharmacotherapy for cAD 3 months before the start of the trial or during the trial period and individuals who had changes in their skin care regimen for cAD 3 months before the start of the trial or during the trial period.
Production of FB water
The water containing high-density FB was prepared using the FB shower head (ReFa FINE BUBBLE S MTG Co.; Figure 1) The device uses air supplied to tap water to produce FB with bubble sizes ≥100 μm.

Study design
This study was a randomised, single-blinded comparative trial conducted at a veterinary hospital in Japan from April to December 2022. A total of 17 cases were enrolled in this trial. The study was conducted according to the Procedures of Good Clinical Practice guideline outlined by the Japanese Ministry of Health, Labour, and Welfare. Prior to the study, written consent from owners allowing their dogs to participate was obtained. The participants in the study were dogs diagnosed with AD as described in the case selection section. They were randomly assigned to either the FB group or the shampoo group (Allermyl; Virbac Japan Co., Ltd) based on a computer-generated random sequence that was established before the trial. The FB group were rinsed or bathed for 5 min per session, and the shampoo group was treated following the manufacturer's manual (https://jp.virbac.com/products/dermalcare/adermyl-1#video). Both treatment periods lasted 4 weeks, during which time the dogs received treatments once a week while maintaining their stable medications.
Assessment of treatment efficacy
The veterinarian who evaluated the cases was blind to the treatment grouping. Skin barrier function parameters were evaluated by VAPOMETER and MOISTUREMETER (Delfin Technologies Ltd) before Day (D)0 and after the 4 week treatment (D28). Before TEWL and SSH measurement, a 30 min acclimatisation period was provided for the dogs in the examination room. The measurements were conducted on the inguinal region under controlled environmental conditions, with temperatures ranging from 20°C to 25°C and humidity ranging from 50% to 70%. The measurements were conducted on both the left and right inguinal areas, and measurement was repeated three times on each side. The average values were used for analysis. However, if the variation between the three measurements exceeded 15%, the results were considered unreliable, and the measurement had to be repeated. CADESI-04 was evaluated by the same veterinarian and PVAS scores were obtained by owner observation at D0 and D28.
Statistical analysis
Clinical scores for the SSH, TEWL, CADESI-04 and PVAS before and after bathing were analysed using paired Student's t tests. Intergroup differences in the clinical scores for all subjects were analysed via the Wilcoxon–Mann–Whitney U-test. All statistical analyses were performed using STATVIEW software (v5.0; Hulinks); p < 0.05 was considered statistically significant.
RESULTS
Of 17 dogs, nine were in the FB group and 8 in the control group. The average age of the dogs was 4.5 years (range 1–11 years). The breeds consisted of 8 French bulldogs, 2 each of shiba inu, West Highland white terriers and toy poodles, and 1 each of Yorkshire terrier, Lhasa apso and mixed breed (toy poodle × Maltese terrier).
CADESI and pVAS
Figure 2 presents the mean ± SD (range) of CADESI-04 and PVAS scores at D0 and D28. In the FB group, the mean ± SD (range) of CADESI score decreased significantly from 16.0 ± 3.8 (1–35) at D0 to 9.4 ± 1.8 (3–19) at D28 (paired Student's t-test, p < 0.05). However, in the shampoo group, the mean CADESI score decreased from 24.8 ± 7.2 (6–62) to 19.3 ± 6.3 (7–50), yet the difference was not significant compared to D0 (p = 0.10).
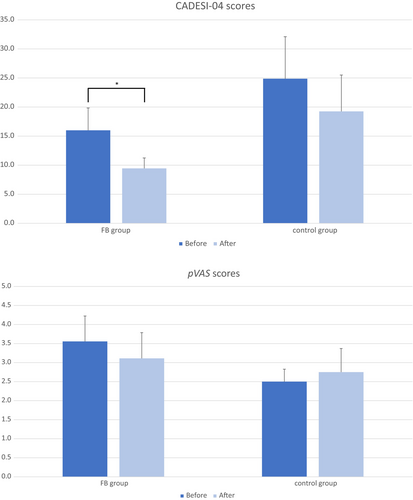
In the FB group, the mean ± SD (range) of PVAS was 3.6 ± 0.7 (2–7) at D0 and reduced to 3.1 ± 0.7 (0–6). In the shampoo group, the mean ± SD of PVAS was 2.5 ± 0.3 (2–4) at D0 and increased to 2.8 ± 0.6 (1–6) at D28. However, there were no significant changes in PVAS in either group (p > 0.05).
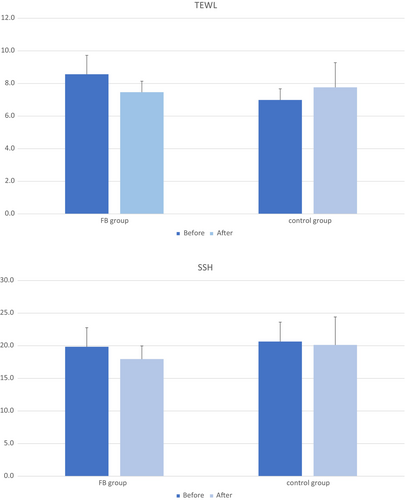
TEWL and SSH
The changes of TEWL and SSH before and after the trial, presented as mean ± SD (range), are shown in Figure 3. In the FB group, the TEWL values were 8.6 ± 1.2 (4.6–12.0) at D0 and 7.5 ± 0.7 (4.5–11.0) at D28. In the shampoo group, the TEWL values were 7.0 ± 0.7 (5.0–10.8) at D0 and 7.8 ± 1.5 (3.4–17.5) at D28. The SSH values in the FB were 20.0 ± 2.9 (12.5–39.7) at D0 and 18.0 ± 2.0 (10.0–25.9) at D28. The equivalent values in the shampoo group were 20.7 ± 3.0 (11.4–36.0) and 20.1 ± 4.3 (8.4–46.0), respectively. No significant changes were observed in TEWL and SSH in both groups, and there was no significant difference in improvement rates between the groups (p > 0.05).
Adverse events
No adverse events related to the use of the FB shower or shampoo were reported by the patient's family or evaluating veterinarians during the trial period.
DISCUSSION
In this randomised, single-blind, controlled trial, the effects of FB on canine atopy were investigated. The results revealed that dogs with AD that received FB bathing once a week for 4 weeks demonstrated a significant reduction in CADESI-04 scores, and no significant changes in PVAS, TEWL and SSH. However, none of dogs in the group that followed the treatment guidelines from 2015 and underwent shampoo treatment demonstrated a significant improvement.
In the present study, the group that received shampoo (Allermyl; Virbac) treatment did not show a significant improvement in terms of clinical presentation and skin barrier function parameters. This finding contradicts the previous study that used the same shampoo method.6 One possible reason for this difference could be attributed to variations in the inclusion criteria. In our study, only cases diagnosed with environmental AD were included, while the previous study included cases with allergic pruritus or pruritus of unknown cause. It has been established that dogs with AD suffer from impaired skin barrier function, and shampoo therapy can potentially alleviate pruritus through short-term skin rehydration and mechanical cleaning.6 However, it should be noted that shampooing may contribute to skin dryness, as evidenced by a slight increase in TEWL following the shampoo treatment.2 Similar observations have been reported in other studies that utilised emollient bathing or a 2% miconazole/chlorhexadine shampoo administered twice weekly, indicating that even emollient bathing can transiently elevate TEWL.16 Therefore, it is crucial to carefully adjust the frequency of bathing or select an appropriate bathing method based on the specific condition of the skin and any existing infections. This individualised approach is necessary to avoid exacerbating skin dryness and irritation.
While there is limited research on the cleaning effects of FB in dogs, a study conducted on healthy dogs demonstrated that bathing with MB (diameter range approximately 1–100 μm) for 15 min had a similar cleansing effect to shampooing for 5 min.17 Additionally, UFB water may possess bactericidal effects on Pseudomonas aeruginosa via damaging the bacterial cell walls, ultimately resulting in cell death.7. Although we did not investigate the bactericidal effects in the current study, UFB bathing could potentially be considered as a treatment option for dogs affected by bacterial infections in the future. Another noteworthy point is recent evidence suggesting that bathing with cleansing agents or surfactants, even those containing moisturisers, may still potentially impair the skin barrier function in dogs.16 Therefore, solely cleaning with FB might provide an alternative option for maintaining skin hygiene. FB bathing has been found to be more effective in cleaning than traditional surfactant-based methods as a consequence of bubble action at the gas/solution interface whereby ascending FB bursts and remove the dirt from the skin surface through negative electrolysis of aqueous solutions.18 Overall, these findings suggest that FB may achieve the same level of skin hygiene as shampooing or even provide better results.17 FB has the potential to alleviate clinical signs in dogs with AD by mechanically removing allergens and micro-organisms from the hair coat and skin. These preliminary findings indicate that FB could be a promising approach for managing allergens and controlling micro-organisms in cAD, potentially offering better clinical outcomes compared to conventional shampoo or even antiseptic shampoo. However, further clinical trials are needed to fully understand the mechanisms and confirm the effectiveness of FB in veterinary dermatological practise.
We must acknowledge the few limitations of our study, including the insufficient number of cases included. Although the statistical analysis showed improvement in the FB group, further trials with large sample sizes and longer durations are necessary to fully understand the efficacy of FB. In conclusion, AD is characterised by the presence of allergens adhering to or penetrating the skin barrier, leading to inflammation, itching and potential complications, such as seborrhoea and imbalanced microflora, which can worsen skin clinical signs. Therefore, effectively managing adhering allergens and micro-organisms through proper cleaning and improving skin and coat hygiene is crucial in the treatment of cAD. In our study, there were no significant changes in skin barrier function parameters observed in either group, although TEWL demonstrated a slight decrease in the FB group and a slight increase in the shampoo group. TEWL is a commonly used indicator for assessing skin barrier function and is associated with CADESI in cAD patients.19 Thus, the main objective of this study was to maintain skin hygiene and minimise damage to the skin barrier function. Based on our findings, FB bathing demonstrated potential as a new cleansing tool with high tolerability and the ability to improve clinical signs in cAD treatment, while having less impact on skin barrier function than frequent shampooing.
AUTHOR CONTRIBUTIONS
Norihito Taguchi: Project administration. Ikki Onishi: Resources. Keita Iyori: Supervision; investigation; funding acquisition; methodology; resources. Yun-Hsia Hsiao: Writing – original draft; writing – review and editing.
ACKNOWLEDGEMENTS
The authors would like to express their gratitude to the owners who dedicated their time to the clinical trial, particularly for participated in the weekly bathing.
FUNDING INFORMATION
This study was partly financially supported by ReFa FINE BUBBLE S MTG Co., which also supplied the fine bubble shower head used in the trial. The funders had no role in study design, data collection and analysis, in writing the manuscript, or decision to publish.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.