Effectiveness of prehospital chest decompression in resolving clinical signs of tension pneumothorax
Abstract
Background
Thoracic injuries are a leading cause of morbidity and mortality in military trauma. Tension pneumothorax (TPX) is a critical diagnosis that can lead to rapid hemodynamic and respiratory collapse if untreated. While timely intervention is essential, prehospital TPX diagnosis is challenging and may lead to unnecessary interventions. This study aimed to assess military prehospital chest injury management, including indications for chest decompression and clinical improvement post-intervention.
Study Design and Methods
Retrospective analysis of the Israel Defense Forces (IDF) Trauma Registry from January 2010 to August 2023 identifying patients who underwent needle or chest tube decompression. Data included demographics, injury mechanisms, vital signs, additional interventions, and prehospital mortality. Chart review evaluated decompression indications and outcomes, with the primary outcome being resolution of decreased oxygen saturation, tachycardia, or hypotension post-decompression.
Results
Overall, 224 patients were included, with a median age of 22 years. The most common injury mechanisms were gunshots (36.6%) and motor vehicle accidents (34.4%). Needle chest decompression was performed in 58.5% of cases, chest tubes in 12.5%, and both in 29.0%. Indications included traumatic cardiac arrest (53.1%), profound shock (17.9%), and SpO2 < 85% (13.8%). In 15.2% of cases, decompression did not meet the IDF guideline criteria. Only three cases (1.3%) showed resolution of tachycardia, hypotension, or low oxygen saturation. In five cases, vital signs briefly returned after traumatic cardiac arrest, but none survived to hospital admission.
Discussion
Chest decompression may be overutilized in prehospital military trauma. Future studies should refine criteria to optimize benefits while minimizing iatrogenic risks.
1 BACKGROUND
Tension pneumothorax (TPX) stands as a significant cause of potentially preventable death on the battlefield, underscored by its potential reversibility through timely and proper field interventions.1-3 The diagnosis of TPX is challenging and is particularly difficult to establish or retrospectively infer once needle or chest tube decompression has been performed. Therefore, the prevalence of this diagnosis remains unclear, with estimates ranging from 1% to 5% among casualties with major trauma.4 In the seminal study by Eastridge and colleagues3 TPX accounted for only 0.2% of mortalities among US military personnel in the conflicts in Afghanistan and Iraq. Although TPX can presumably be effectively managed with immediate chest decompression, several studies have underscored the potential risks associated with such procedures.5-7
The proposed pathophysiology behind TPX includes the loss of the normally negative intrapleural pressure within the affected hemithorax, with increased pressure buildup in the pleural space, which eventually inflicts compression of the intrathoracic vena cava. This compression reduces cardiac preload, leading to a decrease in cardiac output, which can rapidly progress to hemodynamic collapse.8, 9 Alternatively, TPX may also manifest through respiratory dysfunction attributed to progressive atelectasis, pulmonary arterial shunting to poorly ventilated regions, and subsequent hypoxemia.10 This underlying pathophysiology has mainly been established in animal models, which simulated pressure buildup within the thoracic cavity to demonstrate the suggested mechanism of gradual air accumulation in TPX.4, 8, 11 The pathophysiology of pneumothorax is further complicated in multi-trauma patients who may suffer from concurrent bleeding in the chest cavity12 or in other foci, significantly affecting clinical assessment. Furthermore, it is apparent that both the pathophysiology and clinical presentation vary markedly between patients who are spontaneously breathing and those receiving positive pressure ventilation, further complicating diagnosis and management.4, 10, 13
In the prehospital setting, providers' assessment of pneumothorax and tension physiology relies mostly on clinical signs of respiratory or hemodynamic compromise, which dictate the decision for decompression.9, 10 Despite the emphasis of current prehospital protocols, including the Prehospital Trauma Life Support (PHTLS)14 and Tactical Combat Casualty Care (TCCC)15 on the prompt treatment of suspected TPX using needle chest decompression (NCD) and chest tube placement, there is a lack of empirical data supporting the effectiveness of these interventions in addressing suspected TPX or hemothorax in the prehospital context. In this study, we aim to characterize the clinical characteristics of trauma patients who underwent either NCD or chest tube placement by prehospital Israel Defense Forces Medical Corps (IDF-MC) teams and evaluate the effectiveness of these interventions as exhibited by dynamics in vital signs before and after the intervention.
2 STUDY DESIGN AND METHODS
2.1 Study design
Retrospective registry-based study utilizing the IDF trauma registry (IDF-TR). This study was approved by the IDF institutional review board as part of ongoing research to improve the care of military trauma patients (No. 1948–2018) and this manuscript adheres to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement for retrospective studies.16
2.2 Setting and data resources
IDF-MC Advanced Life Support (ALS) teams are led by either physicians or emergency medical technician-paramedics (EMT-P) and provide prehospital trauma care to both civilians and military personnel injured during military operations and civilian trauma or terror attacks occurring in the vicinity of IDF bases. The IDF-TR archives detailed records of prehospital trauma care provided by IDF medical teams from the point of injury through emergency department arrival.17 The registry compiles information from casualty cards along with structured and free-text data recorded by on-scene providers using a web-based platform.
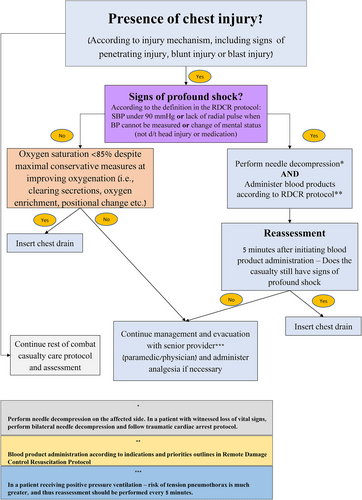
2.3 IDF-MC Clinical Practice Guidelines for chest injury management
The IDF-MC treatment algorithm for the management of chest injuries in the prehospital setting is depicted in Figure 1. The protocol begins with an initial assessment for the presence of chest injury via physical examination. If chest injury is suspected, signs of respiratory or hemodynamic compromise are evaluated. Profound shock is currently defined as either a systolic blood pressure (SBP) <90 mmHg, deterioration of mental status not explained by medication or head injury, or absence of a radial pulse when blood pressure cannot be assessed.18, 19 For the majority of the study period, tachycardia >130 beats per minute also served as a criterion for classifying profound shock.19 If signs of profound shock are present, NCD is performed on the affected side(s), along with blood product administration. Vital signs are reassessed post-needle insertion and blood product administration. If signs of shock persist, chest tube insertion on the affected side is advised. In the absence of profound shock, if significantly decreased oxygen saturation (SpO2 < 85%) is observed despite conservative airway management (i.e., positional change, clearing of secretions, oxygen enrichment, etc.), chest tube insertion on the affected side is also recommended. The protocol stresses that positive pressure ventilation (PPV) increases TPX risk, but the presence of PPV does not guide or change the indications for intervention. Notably, prior to 2022, the protocol also included assessment for clinical signs of pneumothorax, such as decreased breath sounds and asymmetric chest expansion to guide intervention, but these signs were removed in the protocol's revision due to high subjectivity and low sensitivity when performed in the field. Additionally, bilateral chest decompression using NCD or chest tube placement was indicated during the study period for traumatic cardiac arrest to address potentially reversible causes, as previously discussed.20
2.4 Study population, data resources, and chart review
- Lack of documentation for any vital signs (HR, SBP, or SpO2).
- Chest decompression performed by civilian medical personnel.
- Patients treated during the IDF humanitarian aid missions in the Syrian Civil War, who often arrived for prehospital medical care several hours or days after injury. Due to this subpopulation's delayed presentation and distinct injury patterns, their inclusion could skew the representativeness of the broader prehospital trauma patient population.21
- Indication for intervention.
- Vital signs documented pre- and post-intervention.
- Changes in vital signs suggesting clinical improvement and resolution of the indication for intervention (e.g., resolution of profound shock, SpO2 >85%, survival after traumatic cardiac arrest).
Any discrepancies were resolved through evaluation by a third author (OA).
2.5 Variables and definitions
Data extracted from the IDF-TR included demographics, injury setting, mechanism, vital signs, prehospital interventions, and outcomes. Patients were categorized by the type of chest decompression received: NCD, chest tube placement, or both. Profound shock was defined as either an SBP of <90 mmHg and/or a heart rate (HR) >130 beats per minute. Positive pressure ventilation was defined by documentation of either bag-mask ventilation or a definitive airway intervention (i.e., endotracheal intubation or cricothyroidotomy). The primary outcome was post-intervention improvement in vital signs resolving the initial indication for chest decompression, as outlined above.
2.6 Statistical analysis
Continuous variables are presented using the median and corresponding interquartile ranges (IQR), while categorical variables are expressed as counts and percentages of the total. Comparison of categorical variables utilized chi-square and Fisher's exact tests, and quantitative variables were compared using the Kruskal–Wallis test. Statistical significance was set at a p-value <.05 for all tests. All statistical analyses were performed using R software version 4.3.1 (R Foundation for Statistical Computing, Vienna, Austria).
3 RESULTS
3.1 Study population and injury characteristics
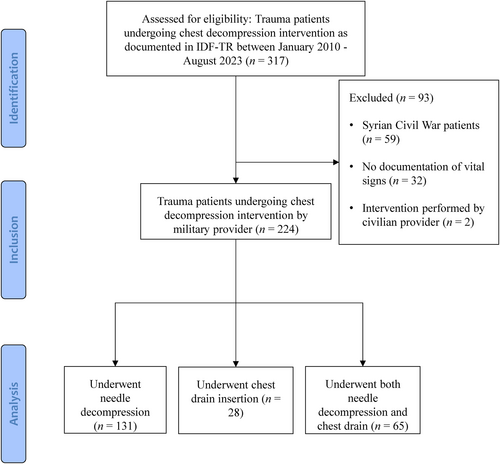
During the study period, treatment of 15,449 patients was documented in the IDF-TR, of which 317 (2.1%) patients underwent chest decompression interventions. Following exclusion, the final cohort included 224 patients (Figure 2). The median age of patients was 22 years (IQR 20–31) and 201 (89.7%) were males. The primary mechanisms of injury were gunshot wounds (n = 82; 36.6%), and motor vehicle accidents (n = 77; 34.4%) with 133 patients (59.4%) sustaining penetrating injuries. Torso injuries were noted in 181 patients (80.8%), with chest injuries documented in 151 individuals (67.4%), back injuries in 44 (19.6%), and abdominal injuries in 47 (21.0%). Regarding vital signs, 157 patients (70.1%) were unresponsive upon the initial assessment. The median maximal HR recorded was 106 beats per minute (IQR 0–130), the median maximal SBP was 97.5 mmHg (IQR 0–120), and the median oxygen saturation was 91.0% (IQR 76.5–98.0). Baseline demographics and injury characteristics of the cohort are detailed in Table 1. Table S1 provides a comparison between patients in the study cohort and those with documented chest injuries who did not undergo chest decompression interventions during the same period and were therefore not included in our cohort. Patients in the study cohort were more frequently injured in military settings, had a higher prevalence of penetrating injuries and gunshot wounds, and were more often unresponsive on the (alert, responds to Voice, responds to pain, unresponsive) AVPU scale compared to those who did not receive interventions.
| Age—median (IQR), years | 22 (20–31) |
| Male sex—N (%) | 201 (91.0) |
| Event type—N (%) | |
| Military | 110 (49.1) |
| Non-military | 114 (50.9) |
| Injury mechanism—N (%)a | |
| Explosion | 16 (7.1) |
| Falls | 6 (2.7) |
| Gunshot wounds | 82 (36.6) |
| Motor vehicle accidents | 77 (34.4) |
| Shrapnel/piercing object | 14 (6.3) |
| Blunt object strike | 9 (3.5) |
| Other | 3 (1.3) |
| Penetrating injury—N (%) | 133 (59.4) |
| Injured body regions—N (%) | |
| Head | 72 (32.1) |
| Eyes | 2 (0.9) |
| Face | 25 (11.2) |
| Neck | 13 (5.8) |
| Upper extremity | 60 (26.8) |
| Lower extremity | 70 (31.3) |
| Torso | 181 (80.8) |
| Chest | 151 (67.4) |
| Abdomen | 47 (21.0) |
| Pelvis | 23 (10.3) |
| Back | 44 (19.6) |
| Other | 19 (8.5) |
| AVPU—N (%)b | |
| A | 26 (11.6) |
| V | 11 (4.3) |
| P | 14 (6.3) |
| U | 157 (70.1) |
| Maximal heart rate—median (IQR), beats per minutec | 106 (0–130) |
| Minimal systolic blood pressure—median (IQR), mmHgd | 97.5 (0–120) |
| Minimal oxygen saturation—median (IQR), %e | 91.0 (76.5–98.0) |
- Abbreviation: IQR, interquartile range.
- a Missing data for 17 patients.
- b Missing data for 16 patients.
- c Missing data for seven patients.
- d Missing data for 108 patients.
- e Missing data for 82 patients.
3.2 Prehospital interventions
NCD was performed on 131 patients (58.5%), while 28 patients (12.5%) received chest tube placement, and 65 (29.0%) patients underwent both NCD and chest tube placement. Positive pressure ventilation was recorded for 153 (68.3%) patients. Volume resuscitation utilizing either crystalloids or blood products was administered in 141 (62.9%) patients. Table 2 summarizes additional prehospital interventions performed apart from chest tube or NCD.
| Prehospital interventions—N (%) | |
| Tourniquet | 27 (12.1) |
| Wound packing | 13 (5.8) |
| Endotracheal intubation | 118 (52.7) |
| Cricothyroidotomy | 22 (9.8) |
| Freeze-dried plasma | 73 (32.6) |
| Whole blood | 29 (12.9) |
| Crystalloids | 77 (34.4) |
| Positive pressure ventilation—N (%) | 153 (68.3) |
| Volume resuscitation—N (%) | 141 (62.9) |
| Prehospital mortality—N (%) | 100 (44.6) |
3.3 Indications for chest decompression
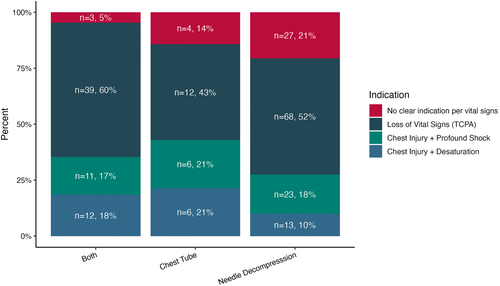
Figure 3 depicts the indications for NCD or chest tube placement as per the IDF-MC chest injury protocol. The most common indication was traumatic cardiac arrest, accounting for 119 (53.1%) cases. Signs of profound shock following chest injury were noted in 40 cases (17.9%) and chest injury with an oxygen saturation below 85% was observed in 31 cases (13.8%). In 34 patients (15.2%), it was concluded that the interventions did not meet the IDF-MC guideline criteria for chest decompression based on the patients' measured vital signs or the descriptive data assessed during chart review.
3.4 Changes in vital signs
Objective resolution of intervention criteria—evaluated by post-intervention changes in HR, SBP, or oxygen saturation—was recorded in only three cases (1.3% of all cases and 2.9% of cases excluding traumatic cardiac arrest), detailed in Table S2. Improvements in oxygen saturation to levels above the intervention threshold (SpO2 ≥ 85%) were documented in two cases following NCD. In one patient, a notable reduction in HR (<130 bpm) alongside an increase in oxygen saturation was documented post-intervention. Notably, in five cases of intervention following traumatic cardiac arrest (n = 119), a temporary return of vital signs was observed; but none of these patients survived to hospital arrival. These particular cases were thoroughly explored in a previous study.20
4 DISCUSSION
Despite spanning more than a decade and including 224 cases, only three cases (1.3%) of objective improvement in vital signs beyond intervention thresholds following NCD or chest tube placement were noted, potentially indicating resolution of TPX. These findings joined with recent literature highlighting both the rarity of TPX pathophysiology in the field along with the potential risks associated with decompression interventions, may suggest a more conservative approach for decompressive chest interventions in prehospital trauma care.
The use of chest decompression interventions in our study (~2%) is slightly higher than previous reports, with previous analyses of trauma systems and Emergency Medical Services (EMS) databases reporting rates of between 0.2% and 1.7%22-25 of all included trauma patients. The true prevalence of TPX among trauma patients, and specifically in a military setting, is likely several folds lower, as demonstrated by its rarity among military trauma fatalities. McPherson and colleagues26 utilized imaging finding criteria to assess the prevalence of TPX among Vietnam War fatalities, concluding that TPX was the cause of death in 3%–4% of casualties. In the Eastridge3 study, which assessed US combat fatalities from 2001 to 2011, TPX was determined to be the cause of death in 0.2% of cases. While advancements in torso protection, alongside updates to treatment protocols and equipment, may contribute to these reduced TPX rates, it is also plausible that TPX represents a very rare occurrence, even among severely injured individuals.27, 28
Studying the effectiveness of prehospital measures targeting TPX is challenging, as patients with resolved TPX and those who did not exhibit TPX physiology before intervention may present similarly upon hospital arrival and subsequent workup. Therefore, evaluating the success rates of interventions such as NCD in reversing tension physiology has been studied by evaluating clinical improvement or imaging signs of pleural decompression. Our study, which focused on the improvement of measured vital signs following chest decompression, found a very low rate of substantial clinical improvement. Newton et al.,24 sought to examine the outcomes of NCD in a Canadian helicopter emergency medical service by assessing several clinical response metrics including a rise in SBP (>90 or 20 mmHg increase from initial measurement), HR (≥ 10 bpm improvement), oxygen saturation (≥10% increase), and return of spontaneous circulation following traumatic cardiac arrest or decreased peak inspiratory pressure. Among 163 patients included in the study, clinical improvement was reported for 37%, with blood pressure improvement fulfilling the abovementioned criteria in 19% of cases. In an analysis of the Pennsylvania Trauma Outcome Study (PTOS) database between 2000 and 2020, which identified 1337 patients undergoing prehospital NCD, ~38% of patients with prehospital hypotension had resolution of hypotension upon admission and ~17% had improvement of an abnormal prehospital HR.25 The markedly lower clinical improvement rates in our study may be explained by several factors. First, nearly 60% of our patient population sustained penetrating injuries, with 36.3% suffering from gunshot wounds and an additional 7.4% injured due to explosions. These rates are relatively high in comparison to the abovementioned studies and may suggest a higher overall injury severity and the presence of conditions such as noncompressible hemorrhage that could impede the effectiveness of chest decompression. Second, nearly half of the injuries occurred in military settings, with emergent intervention in this austere setting presumably being more challenging and associated with lower success rates even in the presence of TPX. Third, the fact that over half of the interventions were performed on patients experiencing traumatic cardiac arrest—a condition with notoriously poor prehospital outcomes20—further complicates the assessment of intervention effectiveness. Lastly, our criteria for improvement, aiming to identify cases of resolved TPX, mandated resolution of severe hemodynamic or respiratory compromise, and thus may have been stricter in classifying clinical improvement.
The literature suggests that the pathophysiology and presenting signs of TPX in spontaneously breathing and positive pressure-ventilated patients vastly differ. Roberts et al.10 conducted a comprehensive systematic review investigating the clinical presentation of TPX, coming to the conclusion that the presentation largely depends on the ventilatory status (i.e., spontaneous vs. positive pressure ventilation). In spontaneously breathing patients, chest pain, dyspnea, and respiratory distress are common, with hypoxia requiring supplemental oxygen and tachycardia being common in both ventilatory states. However, a rapid onset of these signs was more common among patients with assisted ventilation. PHTLS14 guidelines also suggest difficulty in positive pressure ventilation as an additional sign suggesting TPX. In our cohort, 68.3% of patients received PPV, but the low occurrence of clinical improvement did not allow for additional analyses of the association between PPV and this outcome.
Currently accepted prehospital and in-hospital trauma guidelines, including PHTLS14 and TCCC15 and Advanced Trauma Life Support (ATLS),29 utilize various clinical signs and thresholds to direct emergent decompression interventions for chest injuries. The PHTLS guidelines advise chest decompression based on the presence of three criteria: (1) worsening respiratory distress or difficulty with bag-mask ventilation, (2) unilateral decrease or absence of breath sounds, and (3) decompensated shock, defined by an SBP <90 mmHg and narrow pulse pressure. The TCCC guidelines recommend suspecting and intervening for TPX in cases of significant torso trauma or blast injuries, marked by severe respiratory distress, tachypnea, asymmetric breath sounds, low oxygen saturation, shock, or cardiac arrest without lethal wounds, without mandating precise vital sign thresholds for action. Similarly, the ATLS29 guidelines recommend immediate decompression for suspected TPX through needle or finger decompression, based on clinical signs such as respiratory distress, absent unilateral breath sounds, or tracheal deviation. Interestingly, these guidelines, along with the IDF-MC protocol as of January 2024, do not distinguish between spontaneously breathing patients and those ventilated with positive pressure, despite the described differences in pathophysiology and clinical presentation. Thus, an approach that considers patients' ventilatory status may potentially be more applicable in pinpointing the select cases and timing of emergent interventions in the field for suspected TPX. As previously discussed, IDF-MC prehospital clinical practice guidelines favor the use of objective criteria such as vital sign thresholds for intervention with the aim of standardizing care across a wide range of providers with varying skillsets and experience.19 The infrequent improvement observed after chest decompression attempts in this study along with the potential risks attributed to these procedures suggest a need to reassess these criteria to target patient subpopulations with hemodynamic or respiratory compromise, along with clinical signs indicating TPX, based on ventilatory status.
We observed a high frequency of NCD placements in patients whose vital signs did not meet the IDF-MC criteria for chest decompression. Specifically, in 27 cases (21%), NCD was performed despite patients' vital signs not meeting the IDF-MC guideline criteria. This contrasts with chest tube placements, where only four cases (14%) lacked clear indications. This finding may suggest that NCD may be more commonly employed due to its perceived less invasive nature and easier technical skill to learn compared to chest tube placement.30 However, as discussed, NCD placement is not without its risks, which could be significant considering the recommended anatomical location of placement close to vital structures.6, 7 The inclination for NCD may stem from the desire to act quickly while minimizing risk, underscoring the need for reinforced training and adherence to protocols to ensure its judicious use.
4.1 Limitations
Our study has several important limitations. The study relies on data from a prehospital trauma registry, which may be subject to biases inherent in such databases, including inconsistent data entry and documentation of vital signs. Thereby, objective clinical improvement was assessed based on paired measurements of either HR, blood pressure, or oxygen saturation pre- and post-intervention. It is possible that in certain cases, clinical improvement was noted by on-scene providers, but vital signs backing this notion were either unmeasured or undocumented, resulting in an underestimation of the rate of clinical response as measured in this study. Due to reliance on a prehospital database, imaging findings or the course of hospital admission were unavailable, and these could potentially shed light on the presence or lack thereof of TPX, and the effectiveness of chest decompression procedures in reaching the intrapleural space.5 The nature of prehospital documentation and multiple interventions performed in succession or concurrently on such patients makes it difficult to isolate the effect of chest decompression on vital signs. Specifically, in cases where blood products or other volume resuscitation were initiated, it is unclear which intervention had a more profound effect on patient course and vital signs. Furthermore, injuries to body regions outside the torso were common in our cohort, suggesting that clinical deterioration in some cases may have been due to bleeding from other areas, potentially limiting the observed impact of chest decompression alone. However, we do not necessarily view this as a limitation to our study, which sought to evaluate the effectiveness of chest decompression as part of a broader prehospital trauma care framework for such patients who often suffer multi-trauma. Finally, we lack data on potential complications of chest decompression procedures identified later during in-hospital care.
5 CONCLUSIONS
Resolution of severe respiratory or hemodynamic compromise following chest decompression was rare following chest decompression interventions performed by military prehospital trauma providers. These results emphasize the need to reevaluate current guidelines, aiming to better identify cases of TPX that warrant immediate decompression and to assess the prioritization of decompression relative to volume restoration and hemostatic resuscitation.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interests. This work was conducted as part of the Israel Defense Forces Medical Corps Trauma and Combat Medicine Branch's efforts for quality control and improvement in trauma care and did not receive any designated funding.