Transfusion quantities associated with 24-h mortality in trauma patients
Mark H. Yazer and Steven G. Schauer contributed equally as senior authors.
The views expressed in this article are those of the authors and do not reflect the official policy or position of the U.S. Army Medical Department, Department of the Army, Department of Defense, or the U.S. Government.
Abstract
Introduction
Data on the correlation between transfusion volumes and trauma mortality are limited. The association between the total number of red blood cell (RBC) and low titer group O whole blood (LTOWB) units, as well as the total volume of all transfused products that were administered up to 4-h after admission and 24-h mortality was determined.
Methods
The Trauma Quality Improvement Program (TQIP) datasets from 2020 to 2022 were reviewed to identify patients aged ≥15 who received any volume of blood products. Receiver operating characteristic (ROC) were constructed along with the calculated area under the ROC curve (AUROC) to determine the association between the quantity of transfusion and 24-h mortality.
Results
There were 144,379 encounters that met inclusion, with 22,467 patients who died within the first 24 h. There was a 90% probability of 24-h mortality following the transfusion of 56 RBC/LTOWB units (AUROC 0.673), with the 90% specificity, Youden's index, and 90% sensitivity surrounding this probability occurring after the transfusion of 8, 4, and 2 units, respectively. In terms of the volume of transfusion, there was a 90% probability of 24-h mortality following the transfusion of 36,000 mL of all blood products combined (AUROC 0.662), with the 90% specificity, Youden's index, and 90% sensitivity surrounding this probability occurring after the transfusion of 4400, 2000, and 500 mL, respectively.
Conclusions
Both the total number of RBC and LTOWB units transfused and the total volume of all blood products transfused demonstrated poor predictive association with the risk of 24-h mortality in the civilian trauma population.
1 INTRODUCTION
1.1 Background
Traumatic hemorrhage is the leading cause of potentially preventable death.1 Efforts to improve the timing, ratio, and early availability of blood have improved the outcomes of patients in hemorrhagic shock in the last 20 years.2 One of the most important concepts in damage control resuscitation is the ability to rapidly provide patients with potentially large quantities of blood products. However, while multiple scores exist to help predict which patients might need a massive transfusion, once started, it can be unclear if the resuscitation is becoming futile and if the scarce blood resources are being optimally used.3
Several studies have attempted to correlate the number of conventional components transfused, or the rate at which they are transfused, with mortality in trauma patients with varying degrees of success.4-6 For example, in a study of 2299 trauma patients age >16 years old, the 30-day survival amongst those who received a total of at least 50 units of blood (median 77 units) was 35%7; a “universally fatal threshold” derived from the total number of blood products transfused within the first 4-h of admission was not apparent in a logistic regression model. Interestingly in this study,7 even patients who received at least 100 units had 15%–25% 30-day survival. In a different study of 207 trauma patients, the risk of survival equaled the risk of death when 11 RBC units (excluding other blood products) had been transfused within the first 4 h after admission, while at 16 RBC units transfused within the same timeframe, the risk of death was higher than that for survival.8 Once again, although higher transfusion volumes were correlated with higher mortality rates, a critical futility threshold was not observed, with approximately a third of patients who received at least 20 units of RBCs surviving to discharge. A multicenter retrospective study that included 221 trauma patients found ~10%–20% survival at 5- and 30-days after receipt of at least 60 RBC units over two calendar days, with higher survival rates found in injured patients with smaller-volume transfusions.9 While these civilian studies correlated transfusion volumes with longer term survival, several military studies examined the correlation using potentially more relevant shorter survival time point.10 For example, a study of 2608 mostly combat injured soldiers found that administering 20 RBC or whole blood units within 24 h had moderate predictive value for 24-h mortality (34.9% sensitivity and 78.6% specificity),11 while a second military study of nearly 12,000 injured patients did not find a consistent futility threshold that predicted 24-h mortality based on the volume of all blood products transfused.12 In the latter study, 7/10 (70%) of patients who received between 164 and 290 blood products in 24 h survived for at least 24 h. This study also found that amongst 58 injured patients who received 100 or more units of all blood products, nearly 4/5 were alive at 24 h further suggesting that in this population (i.e., primarily military-aged males), futility cannot be entirely defined by transfusion volume alone.12 Although none of these studies found a definite transfusion volume futility point, there appeared to be a negative correlation between the number of blood products transfused and survival, that is, a greater number of transfusions seemed to correlate with decreased survival, as would be expected. However, the heterogeneous nature of the type of blood products studied, the time period over which the transfusions were administered, and the population studied makes comparing outcomes between studies difficult.
Several other studies that analyzed TQIP data have found that transfusion volume alone is not a reliable indicator of mortality.13-15 We sought to determine if there was a number of RBC and/or LTOWB units transfused, or the total volume of all blood products transfused, within the first 4 h after admission that was associated with futility as it relates to 24-h mortality.
2 METHODS
2.1 Ethics
We submitted a request and obtained data from the American College of Surgeons Trauma Quality Improvement Program (TQIP) database, including the additional facilities keys. The Colorado Multiple Institutional Review Board (IRB) reviewed protocol number COMIRB-23-1732 and determined it met the definition of research not involving human subjects. Strengthening of the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines was followed.
2.2 TQIP description
The TQIP database has been maintained by the American College of Surgeons since 2008 and has mandatory data collection for level 1 trauma centers. Other centers that do not meet level 1 criteria can also voluntarily contribute data.16 The goal of the program is to provide data to aid trauma centers in standardizing trauma care, providing local and national quality improvement, and providing the data needed to develop best practices guidelines. There are over 800 participating centers where trained registrars enter data for trauma encounters that meet entry criteria.17, 18
2.3 Case selection and variables
We included patients who were ≥15 years of age and received any volume of any blood product within the first 4 h after admission. All products administered within the first 4 h are captured in the TQIP database as a core metric. TQIP captures blood products by volume (mL). To analyze on a per-unit basis, we used a volume of 350 mL for RBC and 485 mL for LTOWB.
2.4 Data analysis
We performed all statistical analyses using Microsoft Excel (version 365, Redmond, Washington) and JMP Statistical Discovery from SAS (version 17, Cary, NC). We utilized descriptive and inferential statistics to describe the population. Continuous and ordinal variables are presented with medians and interquartile ranges and compared using the Wilcoxon rank sum test. Categorical variables are presented as percentages and numbers and compared using the Chi-squared or Fisher's exact test. We constructed receiver operating characteristic (ROC) curves thresholds that represent 90% probability, 90% specificity, Youden's index, and 90% sensitivity for 24-h mortality based on the number of RBC and LTOWB units administered in the first 4 h after admission and on the total volume of all blood products (rounded to nearest 100 mL) administered during that period. The correlation between the quantity of transfusion and 24-h mortality was also analyzed separately for patients with blunt and penetrating injuries. Youden's index maximizes sensitivity and specificity for a continuous variable to create a dichotomous value by taking the sensitivity + the specificity – 1 and choosing the maximum value. The probability value presented represents the probability of an event occurring over the probability of an event not occurring at the given threshold on the ROC.
3 RESULTS
From 2020 to 2022, there were 3,575,106 encounters in the TQIP database, of which 144,379/3,575,106 (4%) met inclusion for this analysis. Within this cohort, 22,467/144,379 (15.6%) died within the first 24 h (Figure S1). Table 1 demonstrates the demographics of the patients who survived and those who died within 24 h of admission. The median [IQR] age among those who survived compared with those who died within 24 h was higher (42 [28–61] vs. 38 [26–58] years, respectively, p < .001) with a lower proportion of firearm injuries (23% vs. 39%, respectively) but a higher proportion of falls (18% vs. 8%, respectively). The median [IQR] composite injury severity scores were lower among survivors compared with those who died (19 [10–29] vs. 26 [17–38], respectively, p < .001). The volume of blood products administered was lower for survivors for all products compared with those who died within 24-h (Table 2).
| 24 h alive n = 119,296 | 24 h dead n = 22,467 | p-value | |
|---|---|---|---|
| Demographics | |||
| Agea | 42 (28–61) | 38 (26–58) | <.001 |
| Male | 74% (89,635) | 78% (17,619) | <.001 |
| Mechanism of injury | |||
| Collision | 47% (56,535) | 48% (10,741) | <.001 |
| Fall | 18% (21,452) | 8% (1805) | |
| Firearm | 23% (27,185) | 39% (8771) | |
| Stabbing | 10% (12,095) | 4% (963) | |
| Other | 2% (2029) | 1% (187) | |
| Composite injury severity scorea | 19 (10–29) | 26 (17–38) | <.001 |
| Serious injury by body region | |||
| Head/neck | 32% (38,924) | 45% (10,108) | <.001 |
| Face | 2% (2158) | 2% (459) | .012 |
| Thorax | 47% (57,004) | 62% (14,043) | <.001 |
| Abdomen | 32% (39,343) | 32% (7164) | .008 |
| Extremities | 37% (45,172) | 25% (5756) | <.001 |
| Skin | 2% (2955) | 7% (1493) | <.001 |
- a Median (interquartile range).
| 24 h alive; n = 119,296 | 24 h dead; n = 22,467 | p-value | |
|---|---|---|---|
| Volume of transfused blood products (mL), median (IQR) | |||
| LTOWB | 0 (0–0) | 0 (0–0) | <.001 |
| Red blood cells | 604 (300–1200) | 1200 (550–3000) | <.001 |
| Plasma | 170 (0–630) | 500 (0–1634) | <.001 |
| Platelets | 0 (0–200) | 0 (0–251) | <.001 |
| Cryoprecipitate | 0 (0–0) | 0 (0–0) | <.001 |
| Receipt of at least one unit of blood products | |||
| LTOWB | 18% (21,271) | 23% (5208) | <.001 |
| Red blood cells | 84% (101,681) | 90% (20,319) | <.001 |
| Plasma | 50% (60,897) | 63% (14,279) | <.001 |
| Platelets | 28% (33,730) | 37% (8323) | <.001 |
| Cryoprecipitate | 6% (7670) | 12% (2719) | <.001 |
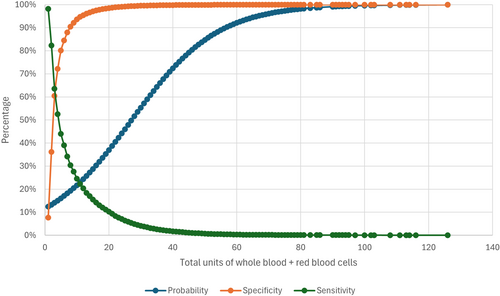
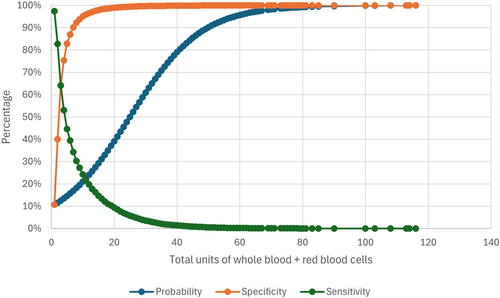
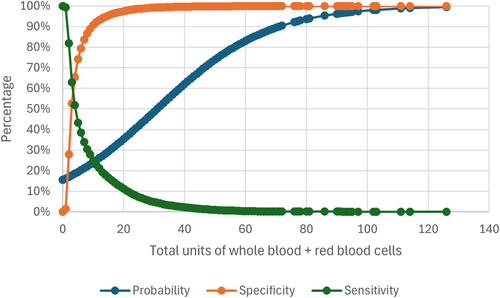
For the overall cohort, when the total number of RBC and LTOWB units transfused within the first 4 h of admission was correlated with 24-h mortality, the 90% probability of 24-h mortality occurred at 56 units, with the 90% specificity, Youden's index, and 90% sensitivity occurring at 8 units, 4 units, and 2 units, respectively, with an AUROC of 0.673 (Table 3, Figure 1). Similar findings were noted when stratifying patients by blunt and penetrating trauma (Figures 2 and 3).
| 90% probability | 90% specificity | Youden's index | 90% sensitivity | AUROC | |
|---|---|---|---|---|---|
| Overall | |||||
| Units of RBC and LTOWB | 56 | 8 | 4 | 2 | 0.673 |
| Volume of all products (mL)a | 36,000 | 4400 | 2000 | 500 | 0.662 |
| Blunt trauma | |||||
| Units of RBC and LTOWB | 50 | 7 | 4 | 2 | 0.700 |
| Volume of all products (mL)a | 31,200 | 3900 | 1800 | 500 | 0.692 |
| Penetrating trauma | |||||
| Units of RBC and LTOWB | 71 | 10 | 6 | 2 | 0.620 |
| Volume of all products (mL)a | 46,600 | 5600 | 3000 | 500 | 0.606 |
- Abbreviations: AUROC, area under the receiving operator characteristic; LTOWB, low titer group O whole blood.
- a Rounded to nearest 100 mL.
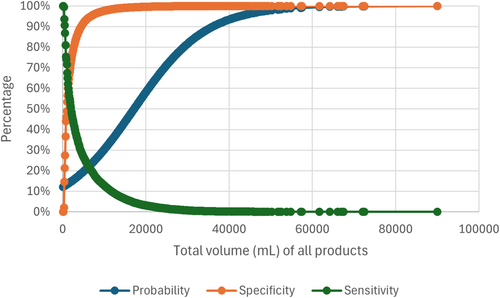
For the overall cohort, when the total volume of all blood products that were transfused within the first 4 h of admission was correlated with 24-h mortality, the 90% probability of 24-h mortality occurred at 36,000 mL, with the 90% specificity, Youden's index, and 90% sensitivity occurring at 4400, 2000, and 500 mL, respectively, with an AUROC of 0.662 (Table 3, Figure 4). Similar findings were noted when stratifying patients by blunt and penetrating trauma (Figures S2 and S3).
4 DISCUSSION
In this study, we correlated the number of RBC and LTOWB units, as well as the total volume of all blood products that were transfused within 4 h after admission with 24-h mortality amongst injured civilian patients. Based on the AUROC, the total number of RBC and LTOWB units transfused and the total volume of all products transfused to blunt trauma patients had the highest correlation with 24-h mortality. Lower AUROC values were seen in the overall cohort and amongst the patients with penetrating injuries. The latter finding is unsurprising, given the large number of patients with blunt trauma in the overall data set. However, it is notable that all the AUROC values are relatively low, suggesting that transfusion is not the ideal sole marker for predicting 24-h mortality during trauma resuscitation, as had been previously demonstrated. Additionally, it is important to note the large volumes of blood products that were required to reach the 90% probability of 24-h mortality, which ranged from 56 RBC and LTOWB units in the overall cohort to 71 for the patients with penetrating injuries. Similarly, the total volume of all transfused products that predicted 90% mortality was >36 L. This coincides with the results of a previous study that found 100% mortality amongst trauma patients who had received 81–90 RBC units (~28,000–32,000 mL of RBC assuming each RBC unit contains 350 mL) in their first 4 h after admission.14 Thus, even after transfusing large volumes of blood products to injured patients, often volumes far in excess of the traditional definition of a massive transfusion, significant survival can still be achieved, and other measures of futility should be explored to determine when the resuscitation should be stopped.
These results are similar to an earlier study that analyzed injured recipients of at least 20 RBC units in 24 h in the TQIP database between 2013 and 2018.13 In that study of 5135 patients, the number of RBC units transfused in the first 4 h after admission had an AUROC value of 0.59 for predicting in-hospital mortality, and the rate of RBC transfusion in the first 4 h after admission had an AUROC value of 0.65. The rate of RBC transfusion in the first 24 h after admission had the strongest correlation with in-hospital mortality, with an AUROC value of 0.85. That study found that a mean transfusion rate of ≥7 RBC units per h for 24 h after admission was consistently a marker of in-hospital mortality when the patients were stratified by mechanism of injury, RBC:plasma ratio, various survival times, and so on. The AUROC values for in-hospital mortality in that study of ultramassively transfused patients were similar to those seen for 24-h mortality in the current study, which did not set a minimum number of units or a minimum volume of transfusion for patient inclusion. However, the study of ultramassively transfused patients was performed before TQIP started capturing LTOWB as a separate variable in 2020. With the growing number of centers that are using LTOWB,17, 19 inclusion of this key resuscitation intervention is important. These findings once again suggest that transfusion itself is not an adequate gauge of either short-term (24-h) or long-term (in-hospital) mortality and that other factors, such as lactate and pH, could also be considered in these mortality prediction models.20
This study has several limitations. We focused on RBC and LTOWB units in our analysis because these are the primary components used in massive transfusion protocols and form the basis for determining how many plasma and platelet units to transfuse when using fixed ratio resuscitation with conventional components. While futility values for plasma and platelets were not separately quantified, their contribution was captured in the analysis of the total volume of blood products administered, thereby providing another metric for determining transfusion futility. As the data were drawn from a database, any coding or data entry errors could lead to inaccuracies in the results. Although it has been recommended to use mortality time points as early as 3- to 6-h after admission when studying hemostatic resuscitation strategies,10 24-h mortality was selected for this study because this was not an intervention study but rather a study to investigate whether transfusion volumes could be used to predict a slightly longer survival period. In any case, the majority of the patients who died in this study did so within the first 6-h after admission (Data S1), therefore, using a slightly longer time point for mortality captured more patients while still studying a relevant endpoint for a resuscitation. Additionally, a previous study suggested that the benefits of LTOWB may not be clearly noted until closer to 24-h after the resuscitation began.21 While some patients received LTOWB during their resuscitation, the overall volume was very low, perhaps reflecting the smaller volumes that were commonly used during the study period.17 It will be interesting to determine if transfusing a larger volume of LTOWB relative to the total volume of blood products administered leads to improved survival, as has been suggested in several recent publications,13, 21, 22 and if it is a more accurate predictor of transfusion futility. The 4-h timeframe used by TQIP to collect data on blood products transfused does not account for prehospital transfusions and is a somewhat arbitrary period of time after admission to stop recording transfusions. Furthermore, those that experienced a traumatic brain injury (TBI) were not excluded from this analysis. While the impact of potentially including patients with TBI is unknown, it is important to note that transfusion practices in TBI cases often differ from a standard massive transfusion protocol.23 Nevertheless, these 24-h mortality prediction models were built on a large number of patients from around the country and recipients of any volume of blood products were included thereby increasing the generalizability of these results.
These data indicate that blood transfusion parameters alone are poor predictors of 24-h patient survival in civilian trauma and that a significant number of patients survive for at least 24 h after receiving quantities of blood products that are far in excess of many traditional definitions of massive transfusion. Other parameters, perhaps a combination of physiological and laboratory-based values, should be explored to improve the ability to predict trauma resuscitation futility.
CONFLICT OF INTEREST STATEMENT
J.A.R., M.D.A., and S.G.S. have received funding from the Department of Defense in the form of grants to their institutions for unrelated efforts. We have no other conflicts to report.