Effect of major trauma on the expected number of births in Finnish women: A nationwide population-based public data and register analysis
Abstract
Background
The effect of major trauma on subsequent fertility is poorly described. If women have lower fertility after trauma, they would have a lower risk of anti-D mediated hemolytic disease of the fetus and newborn in a future pregnancy following the transfusion of RhD-positive blood to RhD-negative women during their resuscitation.
Study Design and Methods
Data was obtained from the Care Register for Health Care, National Medical Birth Register, and open access data from Statistic Finland to evaluate the effect of major trauma (traumatic brain injuries, spine, pelvic, hip/thigh fractures) on the age-specific number of births during years 1998–2018. The total number of births before a specific maternal age for different trauma populations was calculated and these were compared to the corresponding number of births in the general population.
Results
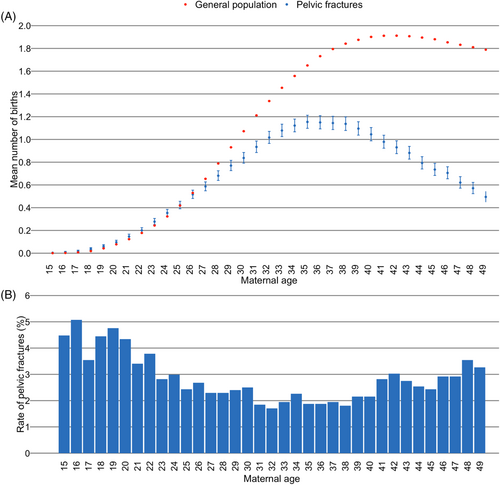
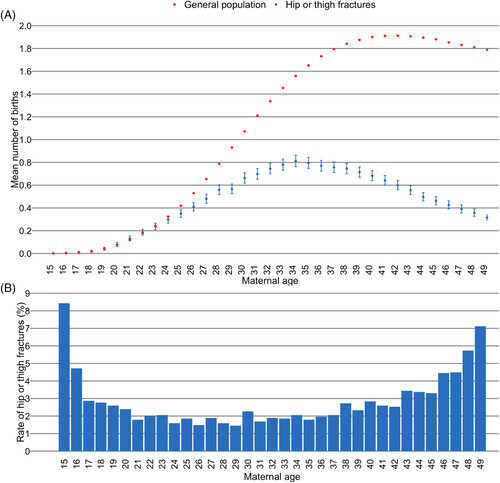
There were 50,923 injured women in this study. All injured women, including when analyzed by the nature of their injury, demonstrated lower expected numbers of births starting at approximately 28 years of age compared to the general population of women in Finland. At age 49, the expected number of births in the general population was approximately 1.8, whereas for all injured women 0.6, women with TBIs and spine fractures 0.6, women with pelvic fractures 0.5, and women with hip or thigh fractures 0.3.
Discussion
Injured women are predicted to have lower fertility rates compared to the general population of Finnish women. The lower fertility rate should be considered when planning a blood product resuscitation strategy for injured women.
Abbreviations
-
- CIs
-
- confidence intervals
-
- HDFN
-
- hemolytic disease of the fetus and newborn
-
- ICD-10
-
- International Classification of Diseases 10th revision
-
- LTOWB
-
- low titer group O whole blood
-
- MBR
-
- National Medical Birth Register
-
- RBC
-
- red blood cells
-
- TBI
-
- traumatic brain injuries
-
- WCP
-
- women of childbearing potential
1 INTRODUCTION
As blood products are increasingly becoming the first-line fluid of choice for military and civilian trauma resuscitation,1-6 supply constraints on universal donor products might limit their availability. When transfusions are administered to patients whose ABO blood group is unknown, such as in the prehospital or early in-hospital phases of the resuscitation, group O red blood cells (RBC) and low titer group O whole blood (LTOWB) must be utilized to ensure compatibility between the recipient's naturally occurring anti-A and/or anti-B and the donor RBCs. It is somewhat more controversial as to which RhD group should be selected for transfusions in this situation.
Ideally, RBCs and LTOWB units that are administered to women of childbearing potential (WCP) whose RhD group is unknown should be RhD-negative. This is because some WCPs who turn out to be RhD-negative themselves will become alloimmunized against the RhD-antigen and the resulting antibody, anti-D, can cause hemolytic disease of the fetus and newborn (HDFN) in a future pregnancy.7 Unfortunately, only a small percentage of RBC and LTOWB donors are both group O and RhD-negative. Since far more donors are RhD-positive than RhD-negative,8 some centers use RhD-positive group O RBCs and LTOWB to meet the needs of urgently bleeding patients whose blood group is unknown early in the resuscitation.9-11
There are myriad events that must occur between the time an injured WCP receives an RhD-positive RBC or LTOWB during her resuscitation and having a pregnancy affected by HDFN in the future. These events have been described elsewhere,12-14 and they include a requirement that the woman actually be of childbearing age and potential, RhD-negative, survive the trauma, become D-alloimmunized, become pregnant with an RhD-positive fetus, and that the fetus experiences some degree of HDFN. Thus, even if the woman develops anti-D as a result of her transfusion during her resuscitation, several other events must still occur in order for a future fetus to be affected by HDFN.
The question of post-trauma fertility has been investigated previously. A retrospective analysis of all injured WCPs between the ages of 15–49 in Finland between 1998 and 2018 found that some women with pelvic fractures and hip or thigh fractures had lower probabilities of giving birth in the 5 years following their trauma compared to women with wrist fractures.15 The goal of that study was to analyze the short-term effects of trauma on fertility, however, given the increasing mean age at which women give birth, it is also important to consider the long-term effects of trauma on fertility rates.16 To this end, a study15 involving two Finnish databases on births and health care was reanalyzed using the maximum length of follow-up that was possible to provide a more comprehensive estimate of their long-term post-injury fertility so that a more accurate fertility rate percentage can be used in risk calculations of HDFN following exposure to RhD-positive RBCs or LTOWB in trauma.
2 STUDY DESIGN AND METHODS
In this retrospective nationwide register-based cohort study, data obtained from the Care Register for Health Care, and the National Medical Birth Register (MBR) were combined with the open-access population data of Statistics Finland on the annual number of different aged women living in Finland. The Care Register for Health Care has a coverage of more than 95%,17 and the National MBR has a coverage of nearly 100%.18, 19 The study period was from January 1, 1998 to December 31, 2018.
Data on all WCPs (15–49 years of age) with traumatic brain injury (TBI), spine fracture, pelvic fracture, or hip or thigh fracture occurring during the study period were identified from the Care Register for Health Care. The Care Register for Health Care includes information on emergency department visits, inpatient care, outpatient control visits, and all surgeries performed in Finland and reporting is mandatory by Finnish law. International Classification of Diseases 10th revision (ICD-10) codes were used to identify the injured WCPs, and they were classified into four types of trauma: TBI, spine fracture, pelvic fracture, and hip or thigh fracture. The specific ICD-10 codes with definitions for each major trauma group included in this study are shown in Table S1. Due to challenges in distinguishing new traumas from follow-up clinic visits/appointments, a woman was included in this study based on her first trauma hospitalization in each category, thus a woman might be included multiple times in different categories if she experienced different types of traumas at different time points.
The data from the Care Register for Health Care were then combined with the data from MBR, which contains data on all pregnancies, delivery statistics, and the perinatal outcomes of births. The data used for this analysis included all births by WCPs during the study period. A birth was defined as an event where a newborn was delivered regardless of the number of babies that were born, for example, regardless of whether a woman delivered a singleton or triplets, this event would be considered to be one birth. To be classified as a birth in the MBR, the newborn had to have weighed at least 500 g or have had a gestational age of at least 22 weeks. Stillbirths that meet the weight or gestational age criteria are also considered births in the MBR. Using the information on the traumas from the Care Register for Health Care, and the dates of the registered births before each age for these injured women, calculating the expected age-specific number of births was possible. The age-specific number of births was calculated separately for all trauma groups (TBI, spine fracture, pelvic fracture, and hip or thigh fracture), and combined value for these trauma groups (“All traumas”). This calculated value was compared to the expected age-specific number of births for women in the general population in Finland. These general population data were obtained from Statistic Finland,20 and the annual total number of births was obtained from the MBR.
2.1 Statistical analysis
Continuous variables were reported as mean with standard deviation or as median with interquartile range based on the distribution of the data. Categorized variables were presented as absolute numbers and percentages with 95% confidence intervals (CIs). The CIs for rates were calculated using Poisson regression.
The expected number of births for each age was calculated using the size of the base population of WCPs living in Finland on the 31st of December of a particular year and the number of annual births was obtained from the MBR. The total number of women of any given age in each year is an open data point that is accessible from Statistic Finland.20 During the study period, the size of the study population decreased from 1,389,409 in 1998 to 1,285,100 in 2018. The total number of women of different ages was calculated for all years separately. To calculate the number of births each woman has had at a specific age, the “previous births”-variable was used, which is a data point that is routinely available in the MBR. This variable is the numerical value of all the previous births for the specific woman. Using this variable allowed for the enumeration and inclusion of births that occurred before the start of the study period. The latest pregnancy before each age was the only one counted, and the previous births variable was used to calculate the expected number of births for this woman before each age. The annual total number of women of different ages and the annual total number of births before each age is shown in Table S2. The age-specific expected number of births was calculated by dividing the total number of births before a specific age by the total number of women with that age in Finland during the study period.
All women with a major trauma (TBI, spine fracture, pelvic fracture, hip or thigh) registered in the Care Register for Health Care were included and their data were linked with the births found in the MBR. For both the injured women and the general population of women, the total number of expected births that each woman had had before she turned a specific age was calculated for the entire cohort of injured women and was also stratified into the four categories of trauma analyzed in this study. Calculating the number of expected births over the reproductive lifespan of each woman (age 15–49; for example, if a woman was injured when she was 20 years old then the expected number of births was calculated for her beginning when she was 15 years old) was limited by the endpoint of the dataset (for example, if a woman was 20 years old when she was injured in 2010, the number of expected births was calculated until she was 28 years old because the dataset ended in 2018) or until she turned 49 years old, whichever endpoint came first. Figure S1 demonstrates five different scenarios that illustrate the relationship between the woman's age at the time of her trauma and the length and nature of the pregnancy follow-up in the dataset. The age-specific number of expected births for injured women was calculated by dividing the total number of births before she turned a specific age by the total number of women who were already that specific age in the dataset. The length of follow-up after trauma reflects the number of years following the trauma and the end of the dataset in 2018 or until she turned 49 years old, whichever came first.
The results of each study are reported according to the STROBE guidelines.21 Statistical analysis was performed using R version 4.0.3 software.
2.2 Ethics
Both the MBR and the Care Register for Health Care used the same unique pseudonymized identification number for each patient. The pseudonymization was performed by the Finnish data authority, Findata. The authors did not have access to the pseudonymization key as it is maintained by Findata. In accordance with Finnish legislation, informed written consent was not required because of the retrospective register-based study design and because the patients were not contacted. Permission to use this dataset was granted by Findata after evaluation of the study protocol (Permission number: THL/1756/14.02.00/2020).
3 RESULTS
In total there were 50,923 injured women included in this study, with a mean (SD) age at the time of injury of 30.4 (11.0) years old, and a mean of 10.6 years of follow-up (Table 1). The mean number of expected births stratified by age was similar between the injured women and the age-matched general population of women until approximately age 28, when the mean number of expected births amongst the injured women began to lag behind that of the general population (Figure 1). From that age onwards, the women in the general population had higher mean expected numbers of births compared to injured women of the same age. Note that the CIs of the two groups do not overlap from approximately age 28 years old onwards, indicating a statistically significant difference in the mean number of births.
| All traumasa | TBI group | Spine fracture group | Pelvic fracture group | Hip or thigh fracture group | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 50,923 | 40,028 | 5773 | 2878 | 2964 | ||||||
| Total number of women includeda | n | % | n | % | n | % | n | % | n | % |
| Age at the time of trauma (mean; SD) | 30.4 (11.0) | 30.0 (10.9) | 31.5 (10.8) | 30.4 (11.0) | 33.1 (11.9) | |||||
| 15–24 years | 19,909 | 39.1 | 16,193 | 40.5 | 1973 | 34.2 | 1141 | 39.7 | 926 | 31.2 |
| 25–34 years | 11,466 | 22.5 | 9078 | 22.7 | 1377 | 23.9 | 643 | 22.3 | 534 | 18.0 |
| 35–49 years | 19,548 | 38.4 | 14,757 | 36.9 | 2423 | 42.0 | 1094 | 38.0 | 1504 | 50.7 |
| Age at the time of delivery (mean; SD) | 28.4 (5.6) | 28.0 (5.6) | 28.5 (5.5) | 27.9 (5.4) | 28.7 (5.4) | |||||
| Total number of deliveries | 37,113 | 29,853 | 4138 | 2096 | 1456 | |||||
| Before trauma | 18,794 | 50.6 | 15,488 | 51.9 | 1903 | 46.0 | 997 | 47.6 | 652 | 44.8 |
| After trauma | 18,319 | 49.4 | 14,365 | 48.1 | 2235 | 54.0 | 1099 | 52.4 | 804 | 55.2 |
| Neonatal mortality | 232 | 0.6 | 179 | 0.6 | 31 | 0.7 | 17 | 0.8 | 8 | 0.5 |
| Multiple pregnancy | 532 | 1.4 | 442 | 1.5 | 46 | 1.1 | 26 | 1.2 | 22 | 1.5 |
| Length of follow-up after trauma (years) (mean; SD) | 10.6 (6.1) | 11.9 (6.1) | 10.4 (6.0) | 10.1 (6.1) | 11.2 (6.0) | |||||
- Note: The results are presented as absolute numbers with 95% confidence intervals.
- Abbreviation: TBI, traumatic brain injury.
- a All traumas included in this study (TBI, spine fracture, pelvic fracture, and hip or thigh fracture).
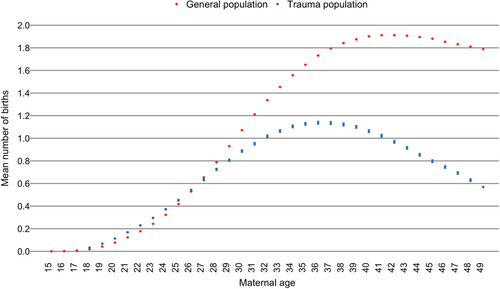
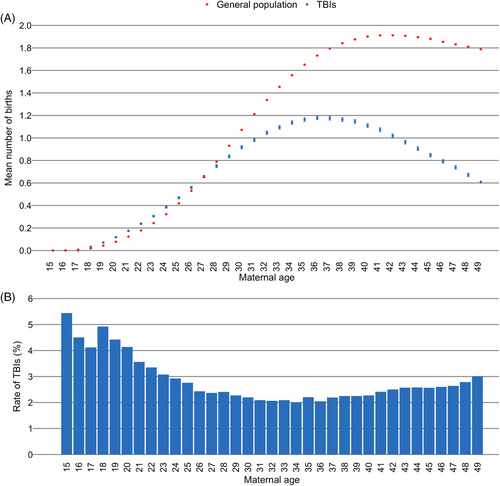
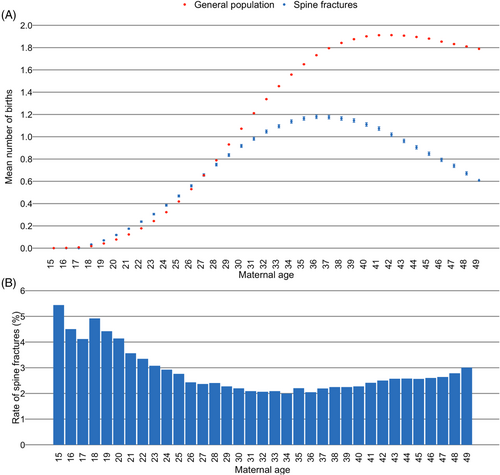
The demographics of the women with specific injuries are shown in Table 1. A similar pattern whereby the mean number of expected births amongst the injured patients falls below that of the general population of women was also observed when this parameter was analyzed by a specific injury mechanism (Figures 2-5). Shown below each figure is the proportion of all the specific injuries that were sustained by women of each age; for example, in Figure 2B, 5.3% of all of the TBI injuries happened to women aged 15 years old and in Figure 3B, 3.1% of all of the spine fractures occurred to women aged 23 years old. At the age of 49, which is considered to be the last year of fertility in this study, the expected number of births in the general population was approximately 1.8, whereas for all injured women the number of expected births was 0.6, and for women with TBIs it was 0.6, for women with spine fractures it was 0.6, for women with pelvic fractures it was 0.5, and for women with hip or thigh fractures the number of expected births was approximately 0.3.
4 DISCUSSION
In this study, all injured women, including when analyzed by the nature of their injury, demonstrated lower expected birth rates starting at around 28 years of age compared to the general population of women in Finland. These data add to the previous study on fertility rates following trauma by extending the period of follow-up after the trauma during which births were enumerated to provide a long-term estimate of fertility post-trauma.15
These results have important consequences on public health policy decisions. For one, since fewer injured women are expected to give birth after their trauma, their risk of developing HDFN from receipt of an RhD-positive transfusion during their resuscitation is correspondingly lower. Knowing the fertility rates following major trauma is an important part of selecting the RhD-type of the RBC and LTOWB units to be potentially provided to WCPs of unknown RhD-type during trauma resuscitation, especially during the prehospital and early in-hospital phases of the resuscitation; these data indicate that HDFN risk calculations based on the fertility rates of the general population might overestimate the HDFN risk since the actual expected fertility rates of injured women are lower starting around the time that women begin to have children. Therefore, the relative safety of administering RhD-positive transfusions for all WCPs, vis-à-vis the HDFN risk, is higher in the target population of interest because of the lower expected fertility rates. This relative safety can be used to justify using the often more abundant RhD-positive RBC and LTOWB units early in the resuscitation and saving the much scarcer RhD-negative units for less urgent transfusion situations in RhD-negative WCPs.
The main strength of this study is that it was based on national registry data that is known to feature high compliance in Finland thereby reducing selection bias and permitting the maximum number of women to be included and analyzed.17-19 In addition, the length of follow-up was at least twice as long as in the original study thereby permitting a longer-term assessment of fertility rates after trauma. However, this study has several limitations. Births that occurred before the start of the analysis and its conclusion would not have been included in this analysis. However, as the total fertility and crude birth rates have remained relatively stable, or perhaps have demonstrated a slight decline over time, in Finland during the study period,16 it is unlikely that the injured women with shorter follow-up time (due to experiencing their trauma close to the end of the database) would have had more children than those who were injured earlier and had longer follow up lengths. Similarly, it was assumed that women who did not give birth during the study period did not give birth at all; the effect of this assumption on the birth rates is expected to be low, and it was applied to both groups of women so any imprecision introduced from this assumption would affect both groups. The two databases analyzed in this study did not contain mortality information so it was not possible to determine which women died from their trauma, although the rate of WCP death from certain injuries is low.22, 23 Thus, the effect of the immortal time bias on lowering the fertility rates of injured women (because they died and could not have children) is expected to be correspondingly low. That some of the injured women might have been included in this study in multiple different injury categories (e.g., TBI and spine fracture) because they sustained multiple injuries at different times does not impact the expected birth rate because the comparison group is all the women of the same age in the general population, not the women in the other trauma categories. Because this was a descriptive study, it was not possible to determine the reason why injured women had lower expected fertility rates compared to the general population. Also, due to the crude nature of these data, it was impossible to correlate the dates of delivery with the dates of injury for all of the injured women, so we could not report whether the injury occurred before or after any of her pregnancies. This means that we were only able to focus on the overall fertility rate of these women. It is unknown which injured women were transfused during their resuscitation, and because these data will likely be used in calculations of the frequency of HDFN following the transfusion of RhD-positive blood products during trauma resuscitation, knowing the transfusion histories would have been helpful to allow us to focus on this population of interest. Several studies have reported the occurrence of sexual dysfunction including dyspareunia after trauma although it is not established that the trauma itself reduces fertility through sterilization procedures performed to arrest bleeding during acute resuscitation.24-26 Lastly, the injury entries in the database are based on ICD-10 codes, which means that the severity of injuries like fractures or TBI were unknown thereby preventing the drawing of more detailed correlations about fertility rate and severity of injury from these data. In addition, the findings presented in this study are based on data collected within a specific context and may not be directly applicable to other countries. Variations in the rates of RhD negativity and the types and frequencies of trauma sustained exist across different regions, and caution should be exercised when attempting to extrapolate these results to other populations.
These data indicate that injured women are predicted to have lower fertility rates starting around the time that women in Finland begin having children compared to the general population of Finnish women. These are important data to consider when planning prehospital and early in-hospital trauma resuscitation strategies because the relatively lower fertility rate post-injury helps to justify the use of RhD-positive blood products for all massively bleeding patients including WCPs.
CONFLICT OF INTEREST STATEMENT
The authors have disclosed no conflicts of interest.