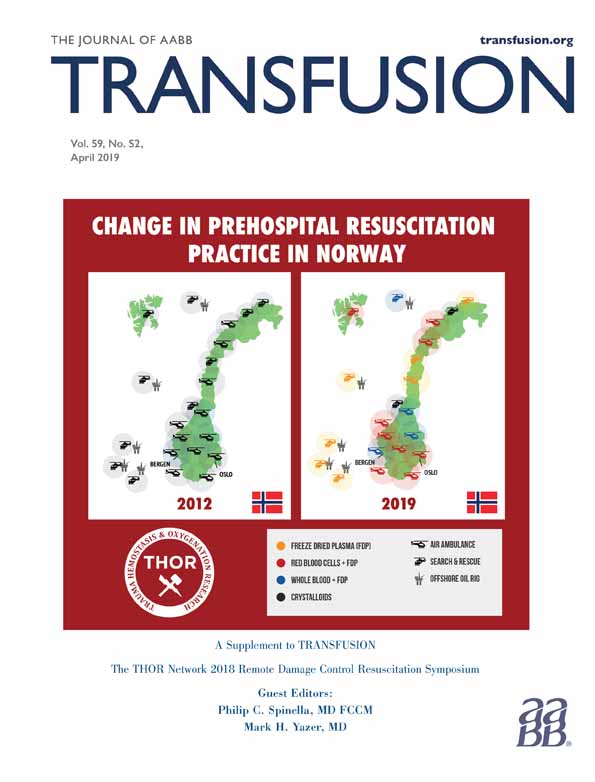
Outcomes of traumatic hemorrhagic shock and the epidemiology of preventable death from injury
Abstract
The majority of potentially preventable deaths after trauma are related to hemorrhage and occur early after injury, with the largest number of deaths occurring before hospital arrival. Approximately one-fourth of trauma deaths may be potentially preventable through early medical and surgical interventions. Interventions dedicated to bleeding control and hemostatic resuscitation have demonstrated merit in decreasing hemorrhagic injury mortality. Advancing these novel strategies to the casualty in the prehospital phase of care, particularly in tactical or austere environments, may prove beneficial for hemorrhage mitigation to temporize the window of survival to definitive care. Future studies of resuscitation and survival after traumatic injury must include analysis of prehospital deaths to fully understand the outcomes of early interventions.
ABBREVIATIONS
-
- CNS
-
- central nervous system
-
- TCCC
-
- tactical combat casualty care
Death from injury was described as the neglected epidemic of modern medicine by the Institutes of Medicine in 1966.1 Despite dramatic advances in acute trauma care over the past several decades, including resuscitation of massive hemorrhage, damage control surgery, and technological advances in critical care, the health burden of injury on our society, in both peacetime and wartime, remains substantial. From a public health perspective, injury remains the leading cause of death accounting for 59% of all deaths among individuals up to the age of 45 and is responsible for a domestic cost of more than $406 billion in medical care and lost productivity each year.2 The majority of injury death occurs prehospital without access to sophisticated medical care.3-5 Being disproportionately represented in a relatively young population, injury stands as the single largest cause of years of life lost and productivity lost in the United States.6 In 2015, a total of 214,000 persons in the United States suffered fatal injury; more than 2,800,000 persons were hospitalized and 27,600,000 persons were treated in emergency departments for nonfatal injuries. Medical treatment and loss of work productivity costs for civilian fatal and nonfatal injuries in the United States totaled more than $671 billion.7 According to a Centers for Disease Control and Prevention report in 2008, a total of 62% of all people who died from injuries and 75% of people who died from gunshot wounds were pronounced dead outside of a hospital.8
Understanding the epidemiology of death after trauma is vital to improving the outcomes of the injured patient. The concept of the distribution of mortality after injury along a chronological axis was initially characterized by Trunkey based on his experience and research in his seminal work describing the trimodal distribution of trauma death. This distribution of death after traumatic injury is classically described with death occurring during immediate, early, and late time frames after injury.9 Despite the empiric presentation that the majority of injury death occurs prehospital, little quantitative data were developed to support this contention.
In a latent review of 425 consecutive injury death autopsies, Trunkey and Lim10 demonstrated that the most substantial etiology of mortality across the spectrum of injury was hemorrhage, which was responsible for 35.2% of deaths. From this and other similar early work evolved concepts of injury prevention, expedited evacuation, the trauma center concept and the nascent architecture of regionalized trauma care, which served as the precursor to our current trauma systems across the United States.
As initially described by Dr. Trunkey, “immediate” deaths occur within 1 hour of injury and are considered unpreventable through available medical interventions. Immediate deaths are most frequently caused by catastrophic whole-body, central nervous system (CNS), cardiac, or great vessel injury. Such immediate deaths are best addressed through an inclusive trauma system integrating injury prevention and contemporary safety interventions. “Early” deaths after trauma usually occur within the first few hours after injury. During this early interval, frequently injured patients have survived a period long enough to receive care from emergency medical services and hospitals. Most deaths in this time interval can be attributed to major CNS injuries or hemorrhage.11, 12 As little can be done to ameliorate the effects of primary CNS injury, clinical efforts are directed toward optimization of brain perfusion and minimizing secondary brain injury. Assuming these tenets, the mortality of injured patients who succumb to CNS injury is largely not preventable. On the other hand, some of the deaths secondary to hemorrhage during this interval are potentially preventable and highlight opportunities to advance medical interventions and trauma systems. The interval between injury and definitive control of the focus of bleeding is most critical for this group of injured patients. The third “peak” in trauma deaths corresponds to trauma patients who die days or weeks after injury, usually due to infection, multiple organ failure, or the latent effects of devastating brain injury. Similarly, optimal care in the early hours after injury may prevent the progression of such sequelae. These improvements in outcome are conceptually secondary to improved resuscitation of hemorrhagic shock and the coagulopathy of trauma with the attendant decreases in organ failure inducing tissue ischemia. Improvements in critical care have improved injury outcomes and minimized the mortality from these clinical entities as evidenced by recent publications which have demonstrated a decrease in deaths during this late third peak.13, 14 It is especially notable that death after trauma is largely an acute phenomenon with approximately 50% of deaths occurring during the first 2 hours after injury, another 25% to 30% within the first 6 hours, and the remainder distributed over the subsequent days to weeks.9, 15
Reducing the time between injury and lifesaving interventions is a critical factor in optimizing injury survival. While the exact length of time that an individual patient can survive depends on their specific injuries, 1 hour has been frequently cited as a goal to deliver an injured patient to a facility capable of surgical management of bleeding in both in the civilian sector and on the battlefield.16-18 Although objective data to support the targeted 1-hour prehospital time have been consistently refuted, few question the fact that earlier interventions save lives in a certain subset of severely injured casualties. Based on substantial clinical experience with injury, in 1975, Cowley19 published his perspective on the development of a comprehensive emergency medical system in the Maryland State Medical Journal. His quote that “the first hour after injury will largely determine a critically injured person's chances for survival” developed into the concept of the “golden hour,” which has remained as a dogmatic guiding tenet of trauma care for emergency medical services for over the past years. Cowley coined the legendary term to promote the urgency between injury and care in establishing the Baltimore Shock Trauma Center, recognizing that trauma patients who reached definitive care sooner had a better chance of survival. A contemporary military analysis assessed the impact of a mandate made in 2009 by Secretary of Defense Gates to reduce the time between combat injury and receiving definitive care to 60 minutes. Reaching this goal required substantial additional aeromedical evacuation assets and the emplacement of additional forward surgical resources. Nonetheless, the initiative demonstrated improved outcomes based on the mandate and substantiated that prehospital transport time and treatment capability were important factors for casualty survival on the battlefield.16
Advances in both military and civilian trauma systems have focused attention on those deaths determined to be potentially preventable through medical means. Although numerous methods of defining “preventable death” have been established, there is no standard definition that has proven universally acceptable, highlighting the challenges of developing such metrics. Regardless of the definition of preventable, hemorrhage consistently emerges as the substantive pathophysiology associated with potentially preventable trauma mortality. In a large contemporary autopsy study of combat deaths from 2001 to 2011, 87% of the 4574 deaths occurred before arrival at a medical treatment facility, and of the prehospital deaths, 24% were considered potentially survivable based on a process of expert review of anatomic criteria established in the study20 (Fig. 1).
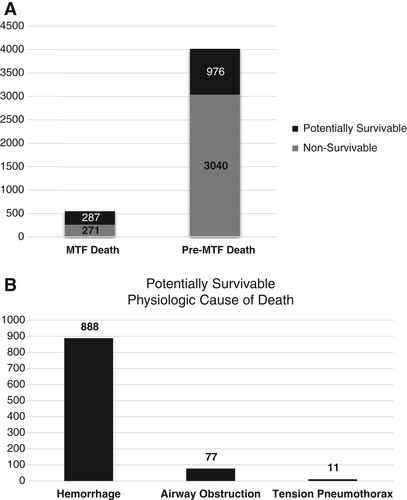
 ) potentially survivable; (
) potentially survivable; ( ) nonsurvivable. (B) Injury/physiologic focus potentially survivable acute mortality (n = 976). MTF = medical treatment facility.
) nonsurvivable. (B) Injury/physiologic focus potentially survivable acute mortality (n = 976). MTF = medical treatment facility.Of the casualties with potentially survivable injuries, 91% of the deaths were associated with a source of hemorrhage. Further stratification noted the site of lethal bleeding as follows: torso 67%, junctional 19%, and extremity 14%. The focus of bleeding in the torso hemorrhage death casualties was predominantly thoracic in 36% and abdominopelvic in 64%. Similar classification of the junctional hemorrhage deaths demonstrated 61% were associated with axilla and groin injuries whereas 39% were associated with cervical injuries.20 Another study utilizing the same method analyzed 558 combat casualties who succumbed to their injuries after reaching a military treatment facility. These died-of-wounds casualties were noted to occur at a rate of 4.6% over the study period, which is strikingly similar to the civilian trauma center case fatality rate of 4.1%. Of the 287 (51.4%) died-of-wounds casualties deemed potentially survivable, 80% of the mortality was directly associated with a source of acute hemorrhage early in the hospital course.21 In 2016, The National Academies of Science, Engineering, and Medicine produced a comprehensive analysis of trauma systems in the United States entitled “National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury,” which deemed that a unified effort is needed to ensure the delivery of optimal trauma care to save the lives of Americans injured within the United States and on the battlefield. This analysis extrapolated the burden of potentially preventable death in the US population utilizing then military mortality evaluation concept. These analyses developed estimates of potentially preventable deaths in the US civilian population of approximately 40,790 in 2014.22
By comparison, analyses of civilian trauma deaths where blunt mechanism of injury is more prevalent, clinical studies also demonstrate that hemorrhage is the most substantial contributor to early trauma deaths. A 1998 analysis of trauma center mortality demonstrated that nearly all of the traumatic mortality directly attributable to hemorrhage occurred within 24 hours from injury.23 A comparable review of in-hospital deaths classified as preventable or potentially preventable demonstrated that 40% were caused by hemorrhage.24 Similarly, another metropolitan trauma center performed a review of 753 consecutive trauma deaths in their hospital. Of these deaths, 53% occurred within 12 hours and 74% within 48 hours. Of this population, 37% of the mortality was attributable to acute hemorrhage.25 A study of civilian prehospital deaths in a large urban county designated 29% of the mortality as potentially preventable, with 64% of those deaths deemed potentially survivable attributed entirely or partially to hemorrhage.26
The prevalence of prehospital deaths in recent conflicts in the southwest Asia remained essentially unchanged compared to previous US wars. The lack of effective management strategies to mitigate life-threatening hemorrhage secondary to trauma has long been recognized as a knowledge and capability gap requiring remediation. In a classic military manuscript, Bellamy27 reviewed the nature of ground combat deaths in a hypothetical model that incorporated data from World War II, the Korean War, and the Vietnam War into a prediction of the causes of death in combat. Approximately 44% of deaths were associated with limb hemorrhage, thereby highlighting extremity bleeding as one of the substantive causes of potentially preventable death on the battlefield. A turning point in military prehospital trauma care came in 1996 when a review of battlefield deaths and the medical requirements to support special operations forces led to the development of a new paradigm for combat casualty care on the battlefield.28 The core principles of tactical combat casualty care (TCCC) were based on the premise of eliminating preventable deaths and combining good medicine with good tactics. Phased care in the tactical environment included care under fire, tactical field care, and tactical evacuation (TACEVAC) care. Casualty and medic actions during the care-under-fire phase were directed toward tactical advantage and mission completion. Simple life-saving interventions targeting hemorrhage control are emphasized in this primary phase of TCCC, with only tourniquets and hemostatic dressings recommended as standard medical care in this phase. These early iterations of TCCC guidelines recommended immediate application of limb tourniquets as the first-line treatment of extremity hemorrhage. Over the ensuing decade, the U.S. military gradually adopted widespread implementation of extremity tourniquets for all deployed forces, ultimately resulting in an 85% decrease in deaths attributed to limb hemorrhage.20 This battlefield lesson was subsequently translated to the civilian population, fostered by the strong advocacy of the Hartford Consensus29, 30 and by the evolution of community bleeding control courses, “Stop the Bleed.”31, 32
While efforts to control isolated extremity hemorrhage after injury have been uniquely successful within the past decade, mitigation of junctional and torso hemorrhage in the prehospital environment remain elusive. A contemporary study to characterize the impact of prehospital time and junctional injury severity on survival utilizing the National Trauma Data Bank research data set found that in patients sustaining junctional injury, increasing severity of anatomic disruption was associated with more significant hemorrhage and mortality. In this study, a mortality rate of 45% was exhibited in high-grade junctional injury groups at prehospital times less than 30 minutes and remained substantial throughout subsequent prehospital time intervals.33 In a parallel study, the same investigators sought to illustrate the association between prehospital time and torso injury severity on survival. This analysis demonstrated that significant torso injury was associated with higher rates of death, particularly in penetrating injury. In fact, the observed mortality rate for high-grade torso injury with hemorrhage was more than 40% in as little as 15 minutes after injury.34 Both of these studies underscore the critical nature of prehospital time in trauma patients with difficult to control bleeding sources. Understanding that evacuation times of less than 30 minutes may not be realistic or attainable, particularly in tactical or austere environments, efforts should be directed toward the development and evolution of novel strategies to mitigate hemorrhage from torso and junctional sources in the prehospital environment and temporize the window of survival.
Based on the understanding that hemorrhage represents the most substantial etiology of potentially preventable deaths after trauma, efforts to develop mitigation strategies have evolved markedly in the past decade. The principle of damage control resuscitation was developed through an observation that combat casualties with massive hemorrhage that received more aggressive correction of coagulopathy immediately after injury had improved survival.35 Increasing plasma:red blood cell (RBC) ratio from 1:8 to 1:1.4 was associated with a threefold decrease in mortality from 60% to 19%. Notably, casualties resuscitated with low ratio were significantly more likely to die from ongoing hemorrhage than those managed with balanced plasma:RBC ratios. The concept of damage control resuscitation has subsequently been refined predicated on optimizing physiology and preventing of the lethal elements contributing to postinjury hemorrhagic mortality: hypothermia, acidosis, and coagulopathy. Incumbent in the damage control resuscitation strategy are the techniques of hypotensive resuscitation (permissive hypotension) and hemostatic resuscitation (amelioration of the coagulopathy of trauma).36, 37
While the concept of damage control resuscitation evolved across the battlefields of Iraq and Afghanistan, research to substantiate the observed successes of fresh whole blood and balanced ratio transfusion practices drew additional attention to the timing of hemorrhagic deaths.38 Consistently, studies supported the fact that for patients who arrive at a trauma center, death from hemorrhage occurs within approximately 2 hours of hospital arrival.39-41 Prospective trauma resuscitation studies in hemorrhaging patients showed that the median time to hemorrhagic death was 2.0 to 2.6 hours, with at least 50% of all deaths occurring within 3 hours of hospital arrival.38
In contrast to the well-characterized outcome of injury mortality after reaching the hospital, there is a paucity of evidence that substantively defines injury-associated death in the civilian prehospital environment or across the continuum of care. One important analysis that included both prehospital and in-hospital traffic injury mortality demonstrated an overall 35% decrease in motor vehicle crash–related deaths over a period of 36 years. For those patients who died prehospital, the rate of death occurred at a logarithmically defined rate that was greatest in the early minutes after injury. Although total traffic deaths decreased over the period of the study, there was an increase in prehospital fatalities relative to hospital fatalities demonstrated.42 These data are consistent with military studies and support the need to focus on prehospital deaths with respect to hemorrhage control, resuscitation, and trauma system design.
Shorter prehospital time has been associated with improved survival in both military16 and civilian trauma patients.33, 34 In addition, recognizing that more rapid transport to surgical hospitals is not always possible, recent trauma system advances have also focused on bringing additional resuscitation capabilities (remote damage control resuscitation) to the seriously injured in the form of prehospital blood transfusion; advanced hemostatic interventions; and light, maneuverable surgical teams.16, 43 Prehospital transfusion in particular has been associated with improved survival in combat casualties.44 Not all studies of prehospital transfusion have demonstrated a survival benefit. However, an analysis of the time to transfusion among evacuated US military combat causalities in Afghanistan demonstrated that blood product transfusion within 36 minutes of injury was associated with improved survival. Beyond this interval, mortality benefits from prehospital transfusion were not significant.45 More recent efforts in battlefield resuscitation have focused on delivering whole blood to severely injured casualties within minutes of injury by combat medics equipped with cold-stored universal donor low-titer group O whole blood as well as the capability to collect fresh whole blood from preidentified donors.46 These and other evolving efforts hold much promise for the future of remote damage control resuscitation.
Future development of remote damage control resuscitation will be predicated on an enhanced understanding of prehospital potentially preventable injury death. Further analysis is needed to develop a coordinated, multidisciplinary, multi-institutional effort within the civilian clinical sector to identify and characterize the causes of premortality from trauma and identify potential high-yield areas for research and development in prehospital medical care, injury prevention, and trauma systems.
In conclusion, the majority of potentially preventable deaths after trauma are related to hemorrhage and occur early after injury, with the largest number of deaths occurring before hospital arrival. Approximately one-fourth of trauma deaths may be potentially preventable through early medical and surgical interventions. Interventions dedicated to bleeding control and hemostatic resuscitation have demonstrated merit in decreasing hemorrhagic injury mortality. Advancing these novel strategies to the casualty prehospital phase of care, particularly in tactical or austere environments, may prove beneficial for hemorrhage mitigation to temporize the window of survival to definitive care. Future studies of resuscitation and survival after traumatic injury must include analysis of prehospital deaths to fully understand the outcomes of early interventions.
CONFLICT OF INTEREST
The authors have disclosed no conflicts of interest.