Suspicious breast lesions incidentally detected on chest computer tomography with histopathological correlation
Abstract
Objective
To evaluate incidental breast lesions on chest computed tomography with histopathological correlation. It is important for general radiologist to characterize a breast lesion as benign, indetermined, or sufficiently suspicious to warrant further work-up.
Methods
A total of 35.000 chest CT examinations were performed between January 2016 and December 2020. 27 patients (mean age 70 years, age range 48–87 years) with incidental breast lesions were identified in this retrospective study. Two radiologists scored incidental breast lesions independently regarding their morphology, and the results were compared to histopathology which was obtained by an ultrasound-guided core needle biopsy or a surgical excision.
Results
Out of 35.000 chest CT examinations, a total of 31 incidental breast lesions in 27 patients were detected. Among the 31 lesions, 23 were malignant and 8 benign. The malignant lesions included 17 carcinomas and 6 metastases (4 lymphomas and 2 melanomas). The benign lesions contained 2 hematomas, 4 fat necrosis, and 2 fibrosis lumps.
Conclusion
Chest computed tomography as a standard imaging technique is helpful for evaluation of suspicious breast lesions. This may ultimately influence patient management and lead to further imaging.
1 INTRODUCTION
Several imaging techniques are available for the diagnosis of breast cancer. Mammography is the preferred screening method for breast cancer detection; however, incidental findings of the breast often present on multidetector computed tomography scans (CT), carried out for different reasons.
A disadvantage of thoracic CT scans is the radiation exposure to the breast tissue. The effective dose during a thoracic CT scan is with 4–7 mSv significantly higher than the effective dose obtained during a conventional mammography with 0.2–0.3 mSv.1
In the last years, the usage of CT examination has been increased enormously in all diagnostic sections.2 New CT techniques give unprecedented spatial and temporal resolution, thus identifying previously unseen structures and pathologies.3 Therefore, diagnostic accuracy can be improved and incidental breast lesions are visualized more often. These might include primary or secondary malignancies, or benign lesions, including benign calcifications, fibroadenomas, or lipomas.4, 5 Studies have shown detection rates for incidental malignant breast lesions of 0.3% on unenhanced CT and 0.6% on contrast-enhanced CT scans.6, 7 In an initial clinical study, there was no relevant distinction between the use of a CT scan in comparison with a mammogram in differentiating benign from malignant lesions.3 When comparing a dedicated contrast-enhanced (ce) breast CT scan with mammography, studies have shown that detection rates for malignant lesions were significantly better on contrast-enhanced breast CT.8 Microcalcifications were seen better on ce breast CT than on nonenhanced breast CT but similarly on mammography.8, 9 Also, malignant lesions showed a more profound enhancement than benign lesions. In dense breast tissue and in lesions located close to the pectoralis muscle, a noncontrast CT scan is better than mammography for the detection of breast lesions.8 It might be possible to incidentally detected early breast cancer by CT; however, the purpose of CT is not breast evaluation.
Previous studies have reported a prevalence of malignant breast lesion among incidental findings of up to 28%.7, 10, 11 Therefore, it is important for radiologists to examine the breast tissue more thoroughly on routine chest CT examinations and characterize incidental lesions as either clearly benign, indeterminate, or suspicious with necessity for biopsy.
The aim of this study was to re-evaluate CT examinations regarding incidental breast lesions and to compare their abnormalities with histopathological results.
2 MATERIALS AND METHODS
2.1 Study design
35,000 chest CT examinations were performed between January 2016 and December 2020 in our hospital. A total of 27 patients included 24 women (88,9%) and three men (11,1%), mean age of 70 years (age range, 48–87 years), with incidental unclear breast lesions detected during a chest CT, were enrolled in this retrospective study.
Each lesion was subsequently examined using B-mode ultrasound with color coded Doppler sonography, ultrasound elastography, and digital mammography. All suspicious lesions were histopathologically analyzed following US-guided core needle biopsy or surgical excision. Only histopathologically confirmed lesions were included in this study. Patients with previously detected breast lesion were excluded.
CT scans were analyzed by two independent radiologists (resident and senior radiologist, with more than two years experience in thoracic CT), blinded to the histopathological results of the breast evaluation regarding diameter, shape, and location of the lesions or if calcification were present.
The local ethics committee approved the retrospective design of this study (Approval number 17–694–104) and written informed consent (including for the images) was obtained from all subjects who were enrolled in the study.
2.2 CT imaging
Two multidetector CT scanner (Somatom Sensation 16 and Somatom Flash Dual Source; Siemens, Erlangen, Germany) were used. Scans were performed either with a standard dose protocol (120 mAs) after application of 70–120 ml of a nonionic contrast agent (Accupaque 350, Bayer-Schering AG) or with a noncontrast low-dose protocol (40 mAs). For image analysis, multiplanar reformations (MPR) with a slice thickness of 3.0 −5.0 mm (kernel: B60f and B40f) were used. All CT datasets were digitally stored in our Picture Archiving and Communication System (PACS).
2.3 Fundamental ultrasound and Mammography
Ultrasound was performed on all patients in a supine position on a LOGIQ E9 scanner (GE Healthcare) using a linear multifrequency transducer (6–15 MHz) by an experienced radiologist (more than two years’ experience in breast ultrasound). First, the whole breast was examined bilaterally using B-mode sonography in sweep technique with standard image documentation. Lesions were documented biplanar.
Tissue density was evaluated using color coded strain and shear wave elastography.12-15 A shear wave elastography imaging method includes point shear wave speed measurement to quantify the tissue stiffness, and it is a highly operator independent technique.16 The principle of strain elastography imaging method involves the manual compression of tissue. This causes tissue displacement or tissue strain. In harder tissue, the strain will be less,16 thus indicating the possible existence of a tumor. The resulting elastography images were displayed using a 256-color map of strain with a scale from red (highest strain, soft) to blue (low strain, hard).
Color coded Doppler sonography (CCDS) and power Doppler (PD) ultrasound were used to evaluate native vascularization. Flow parameters were adjusted to the lowest possible pulse repetition frequency (PRF < 1000 Hz) and the best possible color imaging without blooming artifacts.
Digital mammography of females was performed bilaterally using craniocaudal and mediolateral oblique views. In male patients, only the mediolateral oblique view was used.
Digital ultrasound and mammography images were also stored in a PACS, available for retrospective analysis.
2.4 Clinical outcome
All patients were followed-up for at least six months at a breast care center.
3 RESULTS
3.1 Demographics and study cohort
CT examinations were carried out as a single region or whole body scan. The keyword “breast” was found in 44 radiological reports. Twenty-seven patients, including 24 women (88.9%) and 3 men (11.1%), were found to have one or more incidental breast lesions detected by CT. Out of the 24 women, 18 (75%) had a malignant breast lesion, including 16 (89%) carcinoma. Six female patients were diagnosed with a benign lesion, including four fat necroses. Altogether, 31 lesions were identified and included in this study. Four out of 27 (15%) patients had two histopathologically identical malignant lesions in the same breast. The underlying indications for the CT scans are listed in Table 1.
| Intense thoracic pain | Invasive carcinoma of no special type (NST) |
|---|---|
| Follow-up after CNS-Lymphoma Mediastinal widening on X-ray | Hematoma |
| Suspected severe pneumonia | Invasive carcinoma of no special type (NST) |
| Follow-up after melanoma | Metastasis of melanoma |
| Thoracic pain by spinal metastasis | Invasive carcinoma of no special type (NST) |
| Follow-up after T cell lymphoma | T cell lymphoma |
| Follow-up after squamous cell carcinoma and melanoma | Invasive carcinoma of no special type (NST) |
| Post-traumatic | Fat necrosis |
| Pathological acetabular fracture, spinal pain | Fat necrosis |
| Staging in cerebral metastasis, axillary lymphadenopathy | Invasive carcinoma of no special type (NST) |
| Staging abdominal lymphoma | B cell lymphoma |
| Dialysis, elevated hemidiaphragm | Fibrosis lamb |
| Staging in lymphoma, pathological lymph node | Solid papillary carcinoma |
| Pneumonia | Invasive carcinoma of no special type with ductal carcinoma in situ |
| Intense thoracic pain | Lobular carcinoma |
3.2 Assessment findings
All 27 patients underwent a clinical breast examination followed by ultrasound and mammography. Out of the 31 lesions, 13 (42%) were palpable. In 12 out of 27 patients, suspicious lymph nodes were identified on CT.
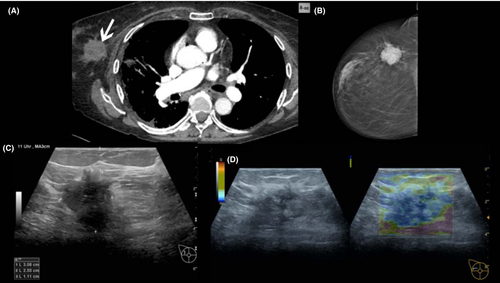
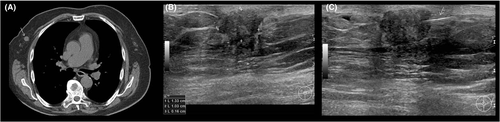
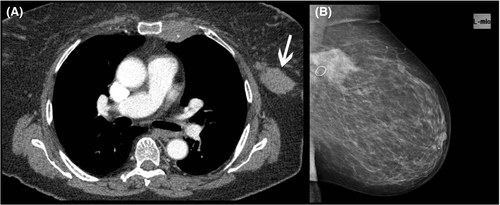
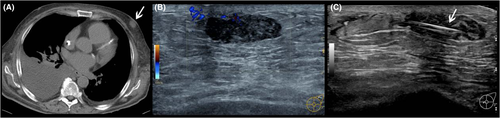
All 31 incidental breast lesions were histopathologically analyzed, following ultrasound-guided core needle biopsy (n = 25) or surgical excision (n = 6). Twenty-three out of 31 masses were found to be primary and secondary breast malignancies (Figures 1-4), and eight were benign (Figure 5). The pathological results are summarized in Table 2.

| No | Radiologist 1 | Radiologist 2 | Pathology | Histological grade | Receptor profile | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diameter | Shape | Location | Calcification | Diameter | Shape | Location | Calcification | ER | PR | HER2 | |||
| 1 | 3,5 | 2 | 1 | yes | 3,3 | 2 | 2 | yes | Invasive carcinoma of no special type (NST) | G2 | - | - | - |
| 2 | 3 | 1 | 1 | yes | 3,2 | 1 | 1 | yes | Hematoma | B2 | |||
| 3 | 1 | 2 | 3 | yes | 1,2 | 2 | 1 | yes | Invasive carcinoma of no special type (NST) | G1 | + | + | + |
| 4 | 1,7 | 1 | 3 | no | 1,5 | 1 | 1 | no | Metastasis of melanoma | ||||
| 5 | 3,5 | 2 | 1 | no | 3,2 | 2 | 1 | no | Invasive carcinoma of no special type (NST) | G2 | + | - | + |
| 6 | 4,8 | 1 | 1 | no | 4,6 | 1 | 1 | no | T cell lymphoma | ||||
| 7 | 1,1 | 2 | 2 | no | 1,3 | 2 | 2 | no | Invasive carcinoma of no special type (NST) | G2 | + | - | - |
| 8 | 1 | 1 | 1 | yes | 1 | 1 | 1 | yes | Fat necrosis | B2 | |||
| 9 | 2,8 | 2 | 1 | yes | 3 | 2 | 1 | yes | Fat necrosis | B2 | |||
| 10 | 2,3 | 2 | 1 | no | 3,5 | 2 | 3 | no | Invasive carcinoma of no special type (NST) | G2 | - | + | - |
| 11 | 0,9 | 1 | 1 | no | 1 | 1 | 2 | no | B cell lymphoma | ||||
| 12 | 1,8 | 1 | 1 | no | 2 | 1 | 1 | no | Fibrosis lump | B2 | |||
| 13 | 1,4 | 2 | 1 | no | 1,2 | 2 | 1 | no | Solid papillary carcinoma | G3 | + | - | + |
| 14 | 1,5 | 2 | 2 | no | 1,3 | 2 | 1 | no | Invasive carcinoma of no special type with ductal carcinoma in situ | G2 | + | + | + |
| 15 | 0,3 | 1 | 1 | no | 0,5 | 1 | 1 | no | Lobular carcinoma | G2 | + | - | + |
| 16 | 1,5 | 2 | 1 | no | 1,2 | 2 | 1 | no | Lobular carcinoma | G2 | + | - | - |
| 17 | 2 | 2 | 2 | yes | 1,8 | 2 | 2 | yes | Fat necrosis | B2 | |||
| 18 | 2 | 2 | 1 | no | 1,9 | 2 | 1 | no | Invasive carcinoma of no special type (NST) | G1 | + | - | - |
| 19 | 1,8 | 2 | 2 | no | 2 | 2 | 2 | no | Invasive carcinoma of no special type (NST) | G3 | - | - | - |
| 20 | 2,2 | 2 | 1 | no | 2,1 | 2 | 1 | no | Invasive carcinoma of no special type (NST) | G2 | + | - | + |
| 21 | 0,7 | 2 | 2 | no | 0,9 | 2 | 2 | no | Invasive carcinoma of no special type (NST) | G3 | - | - | - |
| 22 | 3 | 2 | 1 | no | 3,2 | 2 | 1 | no | Invasive carcinoma of no special type with ductal carcinoma in situ | G2/G3 | - | - | - |
| 23 | 1,5 | 2 | 1 | no | 1,5 | 2 | 2 | no | Invasive carcinoma of no special type (NST) | G2 | + | - | - |
| 24 | 3 | 1 | 3 | no | 2,9 | 1 | 4 | no | Metastasis of melanoma | ||||
| 25 | 2 | 1 | 1 | no | 2 | 1 | 1 | no | B cell lymphoma | ||||
| 26 | 1 | 1 | 1 | no | 1 | 1 | 1 | no | Fat necrosis | B2 | |||
| 27 | 2,3 | 1 | 1 | no | 2,4 | 1 | 1 | no | Fibrosis lump | B2 | |||
| 28 | 1 | 2 | 4 | no | 1 | 2 | 4 | no | Invasive carcinoma of no special type (NST) | G3 | + | + | - |
| 29 | 0,8 | 1 | 3 | no | 1 | 1 | 1 | no | B cell lymphoma | ||||
| 30 | 3,3 | 2 | 2 | no | 3,2 | 2 | 2 | no | Invasive carcinoma of no special type (NST) | G2 | - | + | - |
| 31 | 2 | 2 | 3 | no | 2 | 2 | 1 | no | Hematoma | B2 | |||
Note
- Shape: well defined (1), irregular margin (2). Location: upper-outer quadrant (1), upper-inner quadrant (2), lower-outer quadrant (3), lower-inner quadrant (4).
- Abbreviations: ER, estrogen receptor; HER2, human epidermal growth factor receptor 2; PR, progesterone receptor.
3.3 Lesion characteristics
The mean size of the masses was 2 cm (range 0.3–4.8 cm). On the 27 CT scans, six (22.2%) contained calcifications. Out of these, four (15%) were associated with a mass lesion: one malignant and three benign.
Criteria for malignancy on CT were spiculated masses with irregular margin, irregular shape, and various enhancement pattern. On ultrasound, cloudy hypoechoic pattern with acoustic shadowing with vertical growth, hypoechogenic angular margins, and microlobulations were suspicious for malignancy. Furthermore, irregular vascularization on color coded Doppler sonography and an increased tissue stiffness on ultrasound elastography were characteristics of malignant masses. On mammography, criteria for malignancy were high-density masses with/without calcification pattern. Benign lesions were defined as well circumscribed with even margins, marginal calcifications, or attenuation values of less than 20 Hounsfield units. Indeterminate and malignant breast lesions were defined as spiculated masses with irregular margin and shape and various enhancement pattern.
3.4 Lymph nodes
The axilla was displayed on all CT scans. Criteria for lymph node metastases were a round shape, loss of central fatty hilum and eccentric thickening of the cortex and ill-defined capsular margins. Reactive lymph nodes typically feature an oval shape with a ratio of long axis/short axis >2, a cortical width of up to 3 mm with persisting central fatty hilum. Out of 27 patients 12 (44%) had suspicious lymph nodes: eight ipsilateral and four bilateral. Malignancy was confirmed histopathologically.
4 DISCUSSION
74.2% of 31 incidental unclear breast lesions were malignant. Currently, CT imaging does not have a high enough resolution for confident detection of microcalcifications. Therefore, breast cancers identified by microcalcifications alone cannot be safely determined on CT.17
The incidence of secondary malignancies in our study was increased (19.4%), compared to a general incidence rate of 2% of all breast cancer.18 Secondary malignancies of the breast typically include sarcoma, lymphoma, and melanoma.19
With a prevalence of 50–80%, invasive ductal carcinoma (invasive carcinoma of no special type, NST) is the most common breast cancer type.20 In our study, NST was histopathologically confirmed in 61% of the patients. Two NST were associated with in situ carcinoma; however, no sole ductal carcinoma in situ (DCIS) was found. In our study, six lesions were located close to the chest wall or the axilla.
Due to the low spatial resolution of CT, detection rates of fine microcalcifications are significantly reduced compared to mammography.10 Harish et al. 17 showed that small (0.5 mm) calcifications, which have a higher probability for malignancy, are rarely detected on CT. Almost all calcifications currently detected on CT are benign, only based on the size, due to the limited spatial resolution.
Morphological features of lesions on B-mode ultrasound, such as shape, echotecture, margin, and posterior acoustic features, are important for distinguishing benign from malignant lesions. In our study, most of the breast carcinoma had irregular shapes and spiculated margins on US, consistent with malignancy.10, 21 Contrary, round or oval shaped lesions on ultrasound with circumscribed margins are considered to be benign.21 This could be confirmed on our study. Gray-scale sonography is an essential medical tool in the detection and characterization of breast tumors with a higher sensitivity compared to mammography (88% vs. 69%).22
CCDS serves as a useful tool for distinguishing malignant from benign solid breast lesions, investigating microvascularization and tumor angiogenesis.23 However, the clinical reliability is diminished by limited vascular detection sensitivity.24 Its role is complementary to the high-sensitive B-mode US. In our, analysis of tumor vessel morphology using CCDS shows a positive correlation with histological grade and aggressiveness of the lesions. Thus, it is useful as a primary assessment of the efficacy of neoadjuvant and antineoangiogenesis treatments. CCDS is a valuable problem-solving tool for various breast conditions, and its usefulness extends to male breasts as well.25
Various studies have shown the benefits of both shear wave and strain eleastography for characterization of breast pathologies with a high sensitivity and specificity.26 In combination with B-mode ultrasound, the diagnostic performance and accuracy can be increased.27
Twenty-five breast lesions were detected using a ce CT scan, and six lesions were visible on nonenhanced CT scans. Previous studies have showed that malignant lesions are significantly more conspicuous on ce breast CT compared to unenhanced breast CT or mammography.8 In our study, enhancement features of a lesion were not useful in predicting malignancy. The timing of intravenous iodine administration was not consistent for all scans, with a range from 25 s to 70 s after injection and the number of lesions was too small for statistical analysis.
Axillary lymph node status is one of the most important finding suspicious for breast cancer. Britton et al.28 used ultrasound to evaluate the axillary nodes before sentinel lymph nodes biopsy. Using CT scans, distant lymph nodes can be localized. However, previous studies have shown that the sensitivity and negative predictive value for detection of malignancy in lymph nodes are low.10 This is consistent with our study, in which malignancy in suspicious lymph nodes were histologically confirmed in only 12 out of 27 patients.
Another important risk factor for breast cancer beyond gender is increasing age. Rates of breast cancer are low in women under 40 and highest in women over age 70.29 In our study, the mean age was 70 years.
Our study is limited in its retrospective approach and by the relatively small number of patients included. Preferably, a multicenter study with a greater number of patients should be conducted in the future to further evaluate the results.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
5 CONCLUSION
Breast lesions can be incidental findings on chest CT. However, especially in gravely or chronically ill patients with repeated scans, they can be missed. Even though chest CT cannot provide all information necessary for classifying beast lesions, it seems to be helpful for evaluation of tumor suspicious changes in dense breast tissue. This may ultimately influence patient management and lead to further imaging. Therefore, a thorough examination of the breast, even on routine chest CT for other indications, is crucial.




