Seborrheic Keratosis-Like Melanoma: Novel Insights Into Clinical, Dermoscopic, and Reflectance Confocal Microscopy Diagnosis of an Atypical Melanoma Variant
Funding: The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
ABSTRACT
Background
Studies have found that few lesions clinically diagnosed as seborrheic keratosis (SK) revealed Cutaneous melanoma (CM) on histopathology. When CM mimics SK, they are defined as seborrheic keratosis-like melanoma (SKLM), and a delayed diagnosis and treatment can occur.
Methods
We conducted a retrospective descriptive, monocentric study of the epidemiological, clinical, videodermoscopy (VDS), and reflectance confocal microscopy (RCM) characteristics of histopathologically proven SKLM diagnosed between 2018 and 2024.
Results
The study population consisted of 60 patients: 44 males (73.3%) and 16 females (26.7%) with lesions located in 73.3% of cases on the trunk. Concerning histological type, superficial spreading melanoma was the more frequent (86.7%). More than 50% of tumors had a Breslow thickness <0.8 mm. The findings from the VDS examination using the revised Argenziano Seven Point Checklist revealed that 100% of cases presented at least one dermoscopic melanoma-specific criterion and, for this reason, had an indication for surgical excision. Typical RCM patterns associated with melanoma diagnosis were observed, including irregular honeycomb/cobblestone pattern (82.1%), irregular DEJ nests (78.6%), dermal inflammation (53.6%), irregular dermal nests (53.6%), dendritic cells in sheets/tangled lines (50%), and atypical round cells (39.3%).
Conclusion
Our study provides valuable insights into the dermoscopic, RCM, and histological features of SKLM based on the largest monocentric cohort. The distinctive dermoscopic patterns, along with the confocal features, aid in the differentiation from other pigmented lesions.
1 Introduction
Studies have found that few lesions clinically diagnosed as seborrheic keratosis (SK) revealed Cutaneous melanoma (CM) on histopathology. When CM mimics SK, they are defined as seborrheic keratosis-like melanoma (SKLM), and a delayed diagnosis and treatment can occur [1]. Other benign tumors, as well as potentially pre-cancerous or malignant conditions, may resemble the characteristic clinical features of SK, and a prompt recognition of such tumors using noninvasive diagnostic tools is mandatory to reduce misdiagnosis and facilitate clinicians in the management process [2-6]. The role of dermoscopy, videodermoscopy (VDS), and reflectance confocal microscopy (RCM) in enhancing diagnostic accuracy for cases of SKLM has been explored in limited studies [6-10]. Our retrospective analysis encompassed clinical, dermoscopic, and RCM characteristics of SKLM to identify specific features aiding clinicians in differentiating SKLM from SK using non-invasive diagnostic techniques.
2 Materials and Methods
We conducted a retrospective descriptive, monocentric study of the epidemiological, clinical, VDS, and RCM characteristics of histopathologically proven SKLM. We collected the histopathologic charts of CM diagnosed between January 2018 and November 2024, presenting on the clinical query the diagnosis of suspected SK from the Oncologic Dermatology Unit, IRCCS Azienda Ospedaliero-Universitaria of Bologna, Policlinico of Sant'Orsola. We obtained clinical and pathologic data from the charts for each patient. Sixty SKLM cases were selected. Patients were informed about the study, and a written informed consent for publication of the photographs used in this manuscript was obtained. Clinical and VDS images (×20 and ×40 magnification) obtained using FotoFinderMedicam 800HD (FotoFinder, Germany) were reviewed by two dermatologists with expertise in the field to confirm the definition of SKLM (G.V. and C.B.). We leveraged the Argenziano revised Seven Point Checklist to define standardized dermoscopic characteristics [11]. The seven-point checklist is one of the established methods to diagnose melanoma dermoscopically. This algorithm is based on the recognition of seven melanoma-specific criteria, each of which is classified as major or minor. The presence of one of the three major melanoma-specific dermoscopic features (Atypical network, Blue-white veil, and atypical vascular pattern) is scored as 2 points, and the presence of one of the four minor features (irregular dots/globules, irregular blotches, and regression structures) is scored as 1 point. Under the revised seven-point algorithm, excision is recommended if the total score is ≥1, with a sensitivity of 87.8% and a specificity of 74.5%. Among all lesions, 28 were referred for RCM evaluation. RCM investigation was performed with a Vivascope (MAVIG GmbH, Munich, Lucid-Tech Inc., Henrietta, NY, USA) microscopy. Each skin lesions were systematically evaluated by RCM: one X–Y horizontal mapping (4 × 4-mm mosaic) was performed at each epidermal layer beginning with the stratum corneum through the entire epidermis and until the papillary dermis (maximal depth of imaging: 200–250 µm). Lesion images were evaluated by two expert dermatologists in the field (F.V. and E.D.) according to eight established RCM melanoma criteria (Honeycomb/cobblestone pattern, DEJ pattern, ringed meshwork, dendritic cells, atypical round cells, DEJ nests, dermal nests, inflammation, and cerebriform nests) previously validated [9]. Finally, hematoxylin-eosin slides of the 60 cases were independently reviewed by two pathologists (C.B. and C.M.).
3 Results
3.1 Epidemiological Data
The study population consisted of 60 patients with a histologically confirmed diagnosis of SKLM, including 44 males (73.3%) and 16 females (26.7%). Their age at presentation was <50 years old in 50% of cases, whereas among patients ≥50 years old, the majority were placed in the range 50–70 (26.7%). The anatomical sites were as follows: 73.3% of SKLM were located on the trunk, 20% on the limbs, and 6.7% on the head and neck. Concerning histological type, superficial spreading melanoma was found in 52 cases (86.7%), nodular melanoma in 6 cases (10%), and nevoid melanoma in 2 cases (3.3%). 40 cases displayed a radial growth phase (66.7%), whereas 20 cases (33.3%) displayed a vertical growth phase. Melanoma in situ was reported in 6.7% of cases. Regarding invasive CM, 32 cases (53.3%) had a thickness <0.8 mm, while 28 (46.7%) had a thickness of ≥0.8 mm. Staging according to the AJCC eighth edition demonstrated that 6.7% were classified as pTis, 50% as pT1a, 10% as pT1b, 13.3% as pT2, 13.3% as pT3, and 6.7% as pT4 (Table 1).
| Clinical and pathologic data | N (60) | % |
|---|---|---|
| Age–years | ||
| <50 | 30 | 50 |
| 50–70 | 16 | 26.7 |
| ≥70 | 14 | 23.3 |
| Gender | ||
| Female | 16 | 26.7 |
| Male | 44 | 73.3 |
| Location | ||
| Trunk | 44 | 73.3 |
| Head and neck | 4 | 6.7 |
| Limbs | 12 | 20 |
| Histopathologic subtype | ||
| Superficial spreading melanoma | 52 | 86.7 |
| Nodular melanoma | 6 | 10 |
| Nevoid melanoma | 2 | 3.3 |
| Growth pattern | ||
| Radial | 40 | 66.7 |
| Vertical | 20 | 33.3 |
| Breslow thickness | ||
| <0.8 mm | 32 | 53.3 |
| ≥0.8 mm | 28 | 46.7 |
| Regression | ||
| Present | 18 | 30 |
| Absent | 42 | 70 |
| Ulceration | ||
| Present | 4 | 6.7 |
| Absent | 56 | 93.3 |
| Stage (according to AJCC 8th ed.) | ||
| pTis | 4 | 6.7 |
| pT1a | 30 | 50 |
| pT1b | 6 | 10 |
| pT2 | 8 | 13.3 |
| pT3 | 8 | 13.3 |
| pT4 | 4 | 6.7 |
3.2 Dermoscopic and RCM Features
The findings from the VDS examination using the revised Argenziano Seven Point Checklist revealed that irregular pigmentation appeared in 52 cases, constituting approximately 86.7% of the total cases examined. An atypical pigment network was found in 30 lesions (50%), while atypical vascular patterns were found in 18 patients (30%). Additionally, irregular streaks were identified in 14 cases (23.3%), and regression structures in 20 lesions (33.3%). Furthermore, blue-whitish veil was described in 12 tumors (20%), and irregular dots/globules were found in 8 cases (13.3%). Moreover, the utility of the acknowledged algorithm is to diagnose melanoma dermoscopically. In our series, 100% of cases presented at least one criterion and for this reason had an indication for surgical excision (Figures 1A,B and 2A,B).
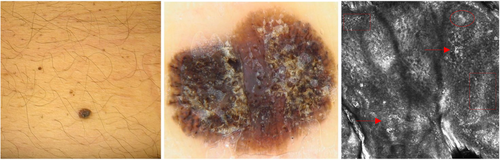
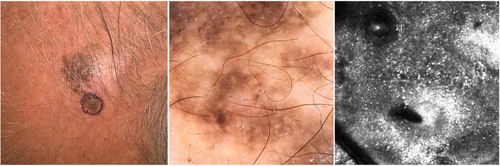
In most lesions, typical RCM patterns associated with melanoma diagnosis were observed, including irregular honeycomb/cobblestone pattern (82.1%), irregular DEJ nests (78.6%), dermal inflammation (53.6%), irregular dermal nests (53.6%), dendritic cells in sheets/ tangled lines (50%), and atypical round cells (39.3%) (Figures 1C and 2C). Results are fully displayed in Table 2.
| Dermoscopic features | N (60) | % |
|---|---|---|
| Atypical pigment network | 30 | 50 |
| Blue-white veil | 12 | 20 |
| Atypical vascular pattern | 18 | 30 |
| Irregular streaks | 14 | 23.3 |
| Irregular pigmentation | 52 | 86.7 |
| Irregular dots/globules | 8 | 13.3 |
| Regression structures | 20 | 33.3 |
| RCM features | N (28) | % |
|---|---|---|
| Honeycomb/cobblestone pattern | ||
| Regular | 5 | 17.9 |
| Irregular | 23 | 82.1 |
| Dermo-epidermal junction pattern | ||
| Ringed | 3 | 10.7 |
| Meshwork | 13 | 46.4 |
| Clod | 1 | 3.6 |
| Combined | 1 | 3.6 |
| Non specific | 10 | 35.7 |
| Dendritic cells in sheets/tangled lines | 14 | 50 |
| Atypical round cells | 11 | 39.3 |
| Dermo-epidermal junction nests | ||
| Regular | 5 | 17.9 |
| Irregular | 22 | 78.6 |
| Dermal nests | ||
| Regular | 6 | 21.4 |
| Irregular | 15 | 53.6 |
| Inflammation | 15 | 53.6 |
| Cerebriform nests | 6 | 21.4 |
- Note: Dermoscopic examination was performed according to the Argenziano revised seven-point checklist.
4 Discussion
As a matter of fact, SKLM represents a rare occurrence in our clinical practice and requires the careful evaluation of dermatologists and dermatopathologists with expertise in the field. The association of SK features in CM has been thought to represent a collision phenomenon, while others have suggested induction of SK-like features in the epithelial component by the melanocytes [12]. The epidermal overgrowth could be induced by a network between melanocytes and keratinocytes involving the epidermal growth factor receptor (EGFR), the fibroblast growth factor receptor (specifically FGFR3), and other pathways [13-16]. For a better comprehension of such a phenomenon, and to characterize SKLM, we evaluated the main dermoscopic RCM and histopathological features of these tumors to identify the presence of possible clues for their identification. To date, only a few papers have investigated such aspects [6, 9, 17, 18]. A previous study described the presence of dermoscopic melanoma features only in 82% of cases [6]. This underlines the difficulty in diagnosing this clinical subtype of melanoma with the naked eye. In our series, using the revised 7-point checklist scoring system, 100% of cases presented at least one dermoscopic melanoma-specific criterion and, for this reason, had an indication for surgical excision, further validating such a great algorithm. Moreover, we performed RCM on 28 difficult lesions. Surprisingly, only a few studies investigated SK-like tumors’ RCM features. A possible explanation is derived from its limited application to this kind of lesion due to the presence of superficial hyperkeratosis. A recent study, based on smaller multicentric cohorts of 19 cases of SKLM, described the presence of an irregular honeycomb pattern in most cases combined with dendritic cells in sheets or tangled lines, atypical round cells, and irregular dermal nests [9]. Our data partially confirm previous reports, with a lower percentage of the irregular honeycomb/cobblestone pattern (82.1% vs. 94.7%) and dermal inflammation (53.6% vs. 89.5). Specific melanoma features were described in all cases, enabling a clear diagnostic assumption of melanoma. Histopathologically, most lesions revealed superficial spreading melanoma subtype (86.7%) with a low incidence of regression (30%) or ulceration (6.7%). More than 50% of the tumors were classified as ≤pT1a. Moreover, in a small percentage of tumors, it was possible to identify a specific pattern of SKLM defined by the presence of a dermal and expansive melanomatous component in a vertical growth phase mixed with an SK-like component of acanthotic-type (large pseudohorn cyst, exophytic and papillomatous appearance with hyperkeratosis, focal acanthosis and epidermal hyperplasia).
5 Conclusion
In conclusion, our study provides valuable insights into the dermoscopic, RCM, and histological features of SKLM based on the largest monocentric cohort. The distinctive dermoscopic patterns, along with the confocal features, aid in the differentiation from other pigmented lesions. However, distinguishing SKLM remains a diagnostic challenge both for clinicians and pathologists.
Acknowledgments
Open access publishing facilitated by Universita degli Studi di Bologna, as part of the Wiley - CRUI-CARE agreement.
Ethics Statement
The study and data acquisition protocol were approved by the Local Ethics Committee, and it was carried out in accordance with the Declaration of Helsinki.
Consent
Patients were informed about the use of their clinical information according to the Declaration of Helsinki principles and photos for a publication intent. Written informed consent was obtained from the patients for publication of the details of their medical case and any accompanying images.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data used during the current study are available from the corresponding author on reasonable request.




