Integrating vascularity into the pattern classification of pilomatricomas on ultrasound provides a more competent approach for discriminative evaluation
Abstract
Background
Pilomatricoma has various manifestations on color Doppler ultrasound, and a differential diagnosis is challenging. The objective of this study was to investigate which characteristics of skin lesions on color Doppler ultrasound are effective in distinguishing pilomatricoma from epidermoid cyst and dermatofibrosarcoma protuberans.
Materials and methods
Records of patients with pilomatricomas (n = 63), epidermoid cysts (n = 76), and dermatofibrosarcoma protuberans (n = 19) who underwent color Doppler ultrasound evaluation and surgical excision were reviewed. The anatomical distribution and color Doppler ultrasound characteristics of these lesions were analyzed. The 63 pilomatricomas were categorized into five types based on their color Doppler ultrasound characteristics, and the roles of these five types in the differential diagnosis of the aforementioned diseases were studied.
Results
Pilomatricomas, epidermoid cysts, and dermatofibrosarcoma protuberans exhibited some similar characteristics. Dominantly markedly hyperechoic or hyperechoic appearance, posterior acoustic shadowing, and the presence of vascularity were the major characteristics of pilomatricomas. The pilomatricomas could be categorized into five types, with type II having a diagnostic performance of sensitivity of 65.08%, specificity of 98.95%, area under the receiver operating characteristic curve (AUC) of 0.743, positive predictive value of 97.62%, and negative predictive value of 81.03% for the diagnosis of the aforementioned skin diseases.
Conclusion
A combination of dominantly markedly hyperechoic or hyperechoic appearance, posterior acoustic shadowing, and the presence of vascularity exhibits higher diagnostic performance for the differential diagnosis of pilomatricomas, epidermoid cysts, and dermatofibrosarcoma protuberans.
1 INTRODUCTION
The skin is the largest organ of the human body, histologically comprising the epidermis, dermis, hair follicles, and appendages.1-3 Many focal lesions originate from these parts of the skin. Among skin focal lesions, pilomatricoma, also known as calcifying epithelioma of Malherbe or trichomatricoma, is a benign tumor derived from the matrix cells of the hair follicles.3-5 It is predominantly found in females during childhood and youth, but can also occur in adults.3-5 Pilomatricoma is typically identified through inspection and palpation when a patient presents with a soft-tissue swelling. Further evaluation is often conducted using high-frequency (7 to 15 MHz) ultrasound (HFUS) associated with color Doppler flow imaging (CDFI).1, 4 On color Doppler ultrasound, pilomatricoma exhibits diverse echogenic patterns.4-7 While pilomatricomas with typical features evaluated using HFUS and CDFI demonstrate excellent diagnostic performance, misdiagnosis frequently occurs for pilomatricomas with atypical sonographic features. These atypical features can resemble other conditions such as infantile hemangioma, trichilemmal cyst, breast cancer, epidermoid cyst, chronic granuloma, and dermatofibrosarcoma protuberans.4-14 Accurate diagnosis is crucial for appropriate management.15, 16 The objective of this study was to investigate the different types of features seen in pilomatricomas on color Doppler sonographies, compare these features with those of epidermoid cysts and dermatofibrosarcoma protuberans, and determine the diagnostic performance of HFUS and CDFI for pilomatricomas.
2 MATERIALS AND METHODS
2.1 Study design and population
In this retrospective study, consecutive patients who had undergone excision of skin focal lesions between January 2013 and November 2023 at a tertiary hospital were retrieved from the informatics database to form the target population. All patients with histopathology of pilomatricoma, epidermoid cyst, and dermatofibrosarcoma protuberans were identified and their pathology results were correlated with the HFUS examination records and patients' medical history. Relevant information was recorded, and the HFUS images were reviewed. The inclusion criteria were patients who had undergone HFUS evaluation within 2 weeks before the surgical resection of the lesions. The exclusion criteria were patients who had not undergone HFUS or had poor quality HFUS images. If a patient had undergone multiple HFUS examinations, only the most recent images and results were included. If a patient had multiple lesions, only the malignant lesion or one representative lesion was included. Based on these criteria, 158 patients with 158 HFUS-detected lesions originating from the skin were included, while three patients with four lesions were excluded. The baseline characteristics of the patients and the HFUS findings of pilomatricomas, epidermoid cysts, and dermatofibrosarcoma protuberans are summarized in Table 1.
| Characteristics | Pilomatricomas (n = 63) | Epidermoid cysts (n = 76) | Dermatofibrosarcoma protuberans (n = 19) | p-value |
|---|---|---|---|---|
| Age (year) | <0.001 | |||
| Mean (Range) | 12 ± 14.5 (1–71) | 39 ± 20.2 (1–86) | 35 ± 13.2 (17–58) | |
| Sex | 0.001 | |||
| Male | 29 (46.0%) | 57 (75.0%) | 14 (73.7%) | |
| Female | 34 (54.0%) | 19 (25.0%) | 5 (26.3%) | |
| Size (mm) | <0.001 | |||
| Mean (Range) | 12 ± 6.9 (4–46) | 26 ± 20.7 (8–89) | 39 ± 20.2 (15–90) | |
| Shapes | <0.001 | |||
| Round /Ovoid | 23 (36.5%) | 5 (6.6%) | 3 (15.8%) | |
| Elliptical | 17 (27.0%) | 51 (67.1%) | 9 (47.4%) | |
| Irregular | 23 (36.5%) | 20 (26.3%) | 7 (36.8%) | |
| Echogenic patterns | <0.001 | |||
| Anechoic | 1 (1.6%) | 0 | 0 | |
| Hypoechoic | 8 (12.7%) | 59 (77.6%) | 13 (68.4%) | |
| Isoechoic | 6 (9.5%) | 14 (18.4%) | 6 (31.6%) | |
| Hyperechoic | 48 (76.2%) | 3 (3.9%) | 0 | |
| Hyperechoic foci | <0.001 | |||
| Present | 61 (96.8%) | 12 (15.8%) | 17 (89.5%) | |
| Absent | 2 (3.2%) | 64 (84.2%) | 2 (10.5%) | |
| Posterior acoustic features | <0.001 | |||
| Shadowing | 32 (50.8%) | 1 (1.3%) | 0 | |
| Enhancement | 4 (6.3%) | 59 (77.6%) | 12 (63.2%) | |
| No evident change | 27 (42.9%) | 16 (21.1%) | 7 (36.8%) | |
| Margin | <0.001 | |||
| Circumscribed | 24 (38.2%) | 53 (69.8%) | 8 (42.1%) | |
| Lobulated/irregular | 17 (26.9%) | 17 (22.3%) | 9 (47.4%) | |
| III-defined | 22 (34.9%) | 6 (7.9%) | 2 (10.5%) | |
| Vascularity | <0.001 | |||
| Absent | 10 (15.8%) | 74 (87.4%) | 0 | |
| Present | 53 (84.2%) | 2 (2.6%) | 19 (100%) |
- Note: Unless otherwise indicated, data are numbers of skin lesions, and numbers in the parentheses are percentages.
The data obtained from patients who had undergone HFUS evaluation, surgical operation, and all study-related procedures and data collection were conducted in accordance with the World Medical Association Declaration of Helsinki (revised in 2013). The study was approved by the Ethics Committee of The First Affiliated Hospital of Hainan Medical University (2023-KYL-039), and informed consent was waived due to the anonymized retrospective study design.
2.2 Acquisition of HFUS images of the skin focal lesions
A large number of patients with focal lesions in the superficial soft tissues were referred to a tertiary hospital for HFUS imaging. Multi-parameter US systems, including Siemens Acuson S2000, Mindray DC 8, Aloka Prosound α−7, Aloka Prosound α−10, Mindray Resona 7, Mindray Eagus R9, Phillips EPIQ5, GE Logiq 9, and GE Logiq E9, were used for the examination of focal lesions by physicians experienced in ultrasound, with 2 to 28 years of experience. During the examination, the US systems were set to small parts mode (small part or superficial), and a linear array transducer with frequencies ranging from 12 to 15 MHz was used. The patients were instructed to position themselves adequately to fully expose the target region. The soft tissues were carefully scanned to detect any lesions, and the location was marked on the sonographic image. The size of a lesion was measured at its greatest dimension in the longitudinal section and its greatest dimension in the cross section. Representative images were saved in the informatics database of the Picture Archiving and Communications System (PACS).
2.3 Interpretation of the HFUS images of the skin focal lesions
In the present study, all the selected sonographic images of the skin focal lesions obtained from the target patients were downloaded from the PACS by an assistant physician who did not analyze these images. Two physicians-in-ultrasound (radiologists), a junior with 2 years and a senior physician with 17 years of experience using HFUS for superficial organs, interpreted and evaluated the images together with consensus. They were blind to the final histopathological diagnosis. The definition and references for echogenicity are as follows: the epidermis is hyperechoic, the dermis is less hyperechoic, the subcutaneous fat is a complex structure composed of hyperechoic collagen septa and hypoechoic fatty lobules. Accordingly, the superficial muscle is defined as isoechogenicity; markedly hyperechogenicity is associated with posterior acoustic shadowing; hyperechogenicity is associated with or without mild posterior acoustic shadowing; isoechogenicity is associated without posterior acoustic shadowing; hypoechogenicity is associated with mild posterior acoustic enhancement; anechogenicity has posterior acoustic enhancement. During the study of the skin focal lesions, the location (head, face, neck, trunk, upper extremity, and lower extremity), shape, margin, size, echogenic texture, hyperechoic foci (calcification), posterior acoustic features, vascularity, and associating findings to abutting tissue were identified and analyzed. The status of lymph nodes in the adjacent region was noted. If a lesion had two or more echogenic patterns, the dominantly larger part of the echogenic patterns was adopted as the lesion's echogenic pattern. The distribution of echogenicity was categorized as homogeneous and heterogeneous pattern. Scattered punctate hyperechoic foci without posterior acoustic shadowing were regarded as microcalcification. Sixty-three pilomatricomas were categorized into different types based on echogenic features and vascularity (blood perfusion) on gray sonography and color Doppler flow imaging (CDFI). The diagnostic performances of different types of pilomatricomas for the 158 cases of skin focal lesions were determined, with histopathology serving as the reference.
2.4 Statistical analysis
Continuous variables with normal distribution were reported as mean ± standard deviation, while those with non-normal distribution were reported as median (interquartile range). Categorical variables were reported as numbers (percentage). Descriptive statistics were used to summarize the primary findings of the study. Independent sample t-tests were used to analyze continuous variables. Receiver operating characteristic (ROC) curve analysis was performed, and the area under the ROC curve (AUC) was calculated. The Youden index was used to determine the optimal cut-off value for sensitivity and specificity. The positive predictive value (PPV), negative predictive value (NPV), AUC, and odds ratio (OR) were calculated. Statistical analyses were conducted using SPSS software for Windows, version 23 (IBM Corp, Armonk, NY, USA) and/or Medcalc statistical software version 15.2.2 (Medcalc software BVBA, Ostend, Belgium). A two-tailed p < 0.05 was considered statistically significant.
3 RESULTS
3.1 Color Doppler ultrasound characteristics and distribution of the skin lesions
Baseline characteristics of patients and HFUS and CDFI characteristics of pilomatricomas, epidermoid cysts, and dermatofibrosarcomas protuberans are summarized in Table 1. Pilomatricoma mainly occurs on the face, neck, head, and arm, while epidermoid cyst mainly occurs on the buttocks, face, neck, and head. Dermatofibrosarcoma mainly occurs on the ventral trunk and leg. The distribution details of these lesions are listed in Table 2.
| Location | Pilomatricoma | Epidermoid cyst | Dermatofibrosarcoma protuberans | |||
|---|---|---|---|---|---|---|
| Head | 4 | 6.34% | 9 | 11.80% | 0 | 0.0% |
| Face | 31 | 49.20% | 7 | 9.20% | 0 | 0.0% |
| Neck | 11 | 17.50% | 10 | 13.20% | 0 | 0.0% |
| Left arm/hand | 1 | 1.5% | 4 | 5.26% | 0 | 0.0% |
| Right arm/hand | 7 | 11.1% | 2 | 2.63% | 0 | 0.0% |
| Ventral trunk | 2 | 3.2% | 5 | 6.61% | 9 | 47.4% |
| Dorsal trunk | 3 | 4.76% | 6 | 7.89% | 5 | 26.3% |
| Lateral trunk | 0 | 0.00% | 2 | 2.63% | 1 | 5.3% |
| Buttocks | 2 | 3.20% | 22 | 28.94% | 0 | 0.0% |
| Perineum | 0 | 0.0% | 3 | 3.95% | 0 | 0.0% |
| Left leg/foot | 1 | 1.6% | 4 | 5.26% | 4 | 21.0% |
| Right leg/foot | 1 | 1.6% | 2 | 2.63% | 0 | 0.0% |
- Note: Data are numbers and percentages of skin lesions.
3.2 Pattern classification of the pilomatricomas based on color Doppler ultrasound
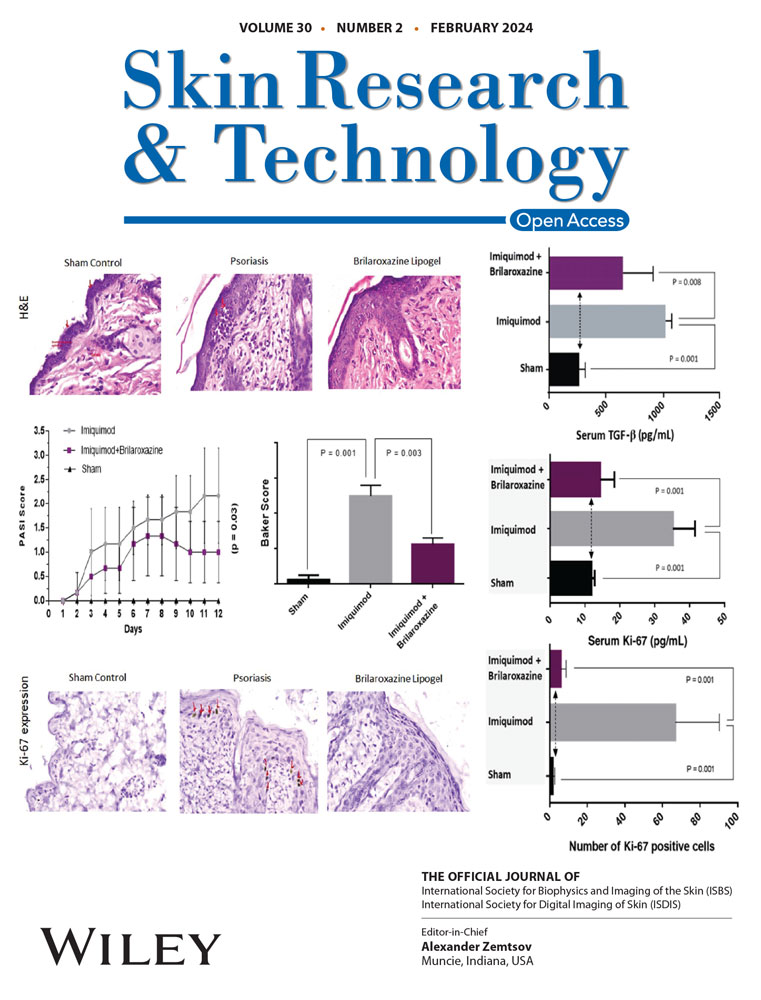
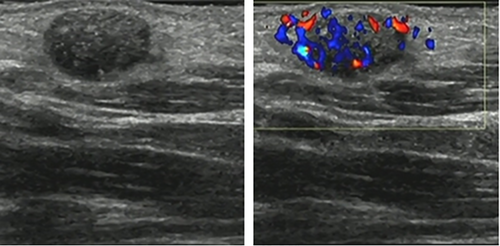
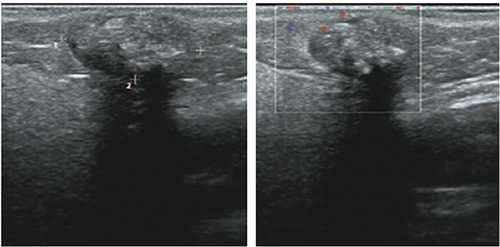
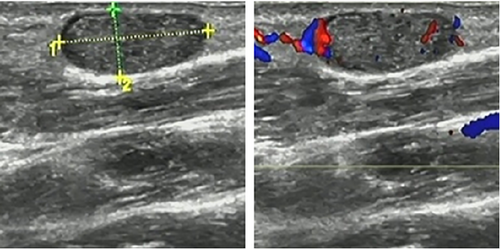
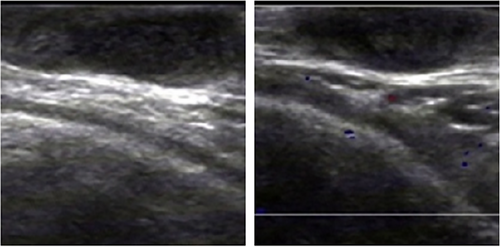
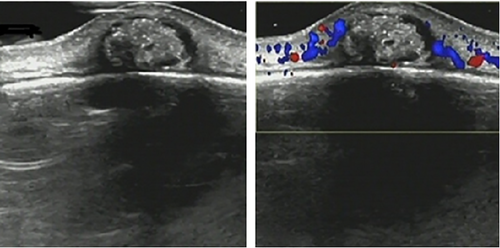
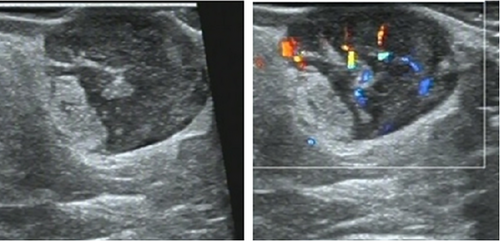
Sixty-three pilomatricomas were categorized into five types based on their echogenic features and vascularity on gray sonography and CDFI. Type I lesions were predominantly isoechoic or hyperechoic, with no evident change in posterior acoustic features and presence of vascularity (as illustrated in Figure 1). Type II lesions were predominantly markedly hyperechoic or hyperechoic, with posterior acoustic shadowing and presence of vascularity (as illustrated in on Figure 2). Type III lesions were predominantly markedly hyperechoic or hyperechoic, with posterior acoustic shadowing and absence of vascularity (as illustrated in Figure 3). Type IV lesions were predominantly hypoechoic, with posterior acoustic enhancement and presence of vascularity (as illustrated in Figure 4). Type V lesions had echogenic patterns other than the above types, such as being predominantly anechoic with posterior acoustic enhancement and presence or absence of vascularity, or predominantly markedly hypoechoic with posterior acoustic enhancement and absence of vascularity (as illustrated in Figure 5). The distribution of pilomatricomas in Type I, II, III, IV, and V were six cases (9.5%), 41 cases (65.1%), 7 cases (11.1%), 6 cases (9.5%), and 3 cases (4.8%), respectively. Type II pilomatricoma was the most common type.
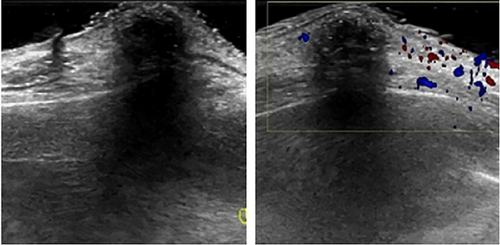

3.3 Main color Doppler ultrasound characteristics of the skin lesions
Scattered hyperechogenic foci were found in 61 pilomatricomas, 12 epidermoid cysts, and 17 dermatofibrosarcomas protuberans. A hypoechoic rim (peripheral hypoechoic halo) was found in five pilomatricomas and nine epidermoid cysts. Fistula sign or submarine sign was present in five cases of epidermoid cysts, and onion sign was present in one case, but these features did not appear in pilomatricomas and dermatofibrosarcomas protuberans. Figure 6 illustrates a pilomatricoma mistaken as an epidermoid cyst, Figure 7 illustrates an epidermoid cyst mistaken as a pilomatricoma, and Figure 8 illustrates a dermatofibrosarcoma protuberans mistaken as a pilomatricoma.
3.4 Using patterns of pilomatricomas for differential diagnosis of the skin lesions
Using Type II as a reference for diagnosing pilomatricoma from the 158 skin lesions, the diagnostic performance in terms of sensitivity, specificity, AUC, PPV, NPV, and OR were 65.08%, 98.95%, 0.743, 97.62%, 81.03%, and 175.2, respectively. The diagnostic performances based on other references of Types are summarized in Table 3.
| Echogenic patterns | Youden index | Sensitivity | Specificity | AUC | PPV | NPV | OR |
|---|---|---|---|---|---|---|---|
| Type I | 0.11 | 9.52% | 96.84% | 0.555 | 66.67% | 61.74% | 3.23 |
| Type II | 0.49 | 65.08% | 98.95% | 0.743 | 97.62% | 81.03% | 175.18 |
| Type III | 0.09 | 11.11% | 100.00% | 0.543 | 100.00% | 62.91% | – |
| Type IV | 0.22 | 9.52% | 86.32% | 0.609 | 31.58% | 58.99% | 0.66 |
| Type V | -0.07 | 4.76% | 91.58% | 0.466 | 27.27% | 59.18% | 0.54 |
- Abbreviations: AUC, area under the ROC curve; NPV, negative predictive value; OR, odds ratio; PPV, positive predictive value.
4 DISCUSSION
Because pilomatricomas, epidermoid cysts, and dermatofibrosarcomas protuberans exhibit some imitating features on color Doppler ultrasound examination, differential diagnosis must be done in clinical practice. Magnetic resonance imaging (MRI) has high resolution in soft tissues, and it is often used for the diagnosis of skin focal lesions, such as the identification of dermatofibrosarcoma protuberans, but it is hard to make a reliable diagnosis of pilomatricoma,17, 18 Typical epidermoid cysts with unique features such as the fistula sign or submarine sign and onion sign can be confidently diagnosed using HFUS examination.19 However, typical epidermoid cysts with uncommon features may be mistaken for other lesions.20, 21 In our study, there were five epidermoid cysts with the fistula sign or submarine sign and one epidermoid cyst with an ambiguous onion sign, and these features did not appear in pilomatricomas and dermatofibrosarcomas protuberans.
Scattered punctate hyperechoic foci or dots are predominantly present in pilomatricomas, but they can also appear in epidermoid cysts and dermatofibrosarcomas protuberans.21 The echogenic texture of pilomatricomas is predominantly heterogeneous due to the presence of calcification and other changes, while epidermoid cysts and dermatofibrosarcomas protuberans mainly present as homogenous echogenicity. The presence of scattered punctate hyperechoic foci alone is not sufficient to support the differential diagnosis, as there can be overlap of these features.
Our study showed that posterior acoustic features are highly suggestive for differentiating between pilomatricomas and epidermoid cysts and dermatofibrosarcomas protuberans. Posterior acoustic shadowing is predominantly present in pilomatricomas and occasionally in dermatofibrosarcomas protuberans and epidermoid cysts, while posterior acoustic enhancement is predominantly present in epidermoid cysts and occasionally in pilomatricomas. These findings are consistent with previous studies.4-8, 21-23 Vascularity is typically absent in epidermoid cysts unless there is coexisting inflammation, while it is rich in dermatofibrosarcomas protuberans and frequently present in pilomatricomas.20, 22, 23 In our study, two epidermoid cysts were mistaken as pilomatricoma and inflammatory lesions.
Of the hypoechoic rim, we used the criterion from the Type 2 in the study by Pelizzari et al.5 Only five pilomatricomas were found to have a hypoechoic rim (7.9%, 5/63), while there were nine epidermoid cysts with a hypoechoic rim (11.8%, 9/76) in our study, as shown in Figures 4 and 7. Therefore, the presence of a hypoechoic rim is not a unique diagnostic factor for pilomatricoma, which differs from the findings of Choo et al.6 and Wei et al.21 The reason for this discrepancy may be the variation in inter-reader agreement for identifying a hypoechoic rim.
Pilomatricomas are typically solid and rarely cystic or a mixture of solid and cystic components. However, Solivetti et al. reported two cases of cystic pilomatricomas in their study,4 Yu et al. reported a pilomatricoma with a bullous appearance,9 and in our study, only one pilomatricoma showed a predominantly cystic composition. This type of pilomatricoma can be easily misdiagnosed. In our study, we found that some pilomatricomas were difficult to assign to any of the echogenic patterns proposed by previous researchers,4, 5 and it was more appropriate to assign them to the patterns proposed by Choo et al.6 Based on these findings, we believe that a combination of HFUS and CDFI features of skin focal lesions may be useful for differential diagnosis. In this study, pilomatricomas were classified into five types, and vascularity was assessed as an important feature detected by CDFI. Vascularity was present in 84.2% of the pilomatricomas in our study, compared to 47.3% (80/169) in the study by Pelizzari et al.,5 50% (22/44) in the study by Choo et al.,6 and 4/32 in the study by Solivetti et al.4 However, the latter two studies did not include vascularity as a criterion for classification of pilomatricomas.4, 6
Our study results were consistent with the findings of Choo et al.6 that scattered dots were the most common pattern of calcification in pilomatricomas. However, we did not agree with the notion that features such as heterogeneous echotexture, internal scattered-dot echogenic foci, hypoechoic rim, or posterior acoustic shadowing alone could be essential criteria for differentiating pilomatricomas from other subcutaneous tumors. This is because the majority of pilomatricomas do not have a hypoechoic rim, as reported by Solivetti et al.,4 where the hypoechoic halo (hypoechoic rim) was observed in only 12.5% of cases (4/32), which was also validated in our study. Additionally, some skin lesions, such as ossified myositis, keloid with calcification, steatonecrosis with calcification, and calcified hemangioma, can also exhibit posterior acoustic shadowing.12 The reason for the difference in our study results compared to Choo et al.6 may be due to the variance in sample size and age of the study population. This is supported by the study conducted by Hosokawa et al., which found that pilomatricomas with a longer symptom duration were more likely to exhibit more severe posterior acoustic shadowing.7 It is well-known that pilomatricomas predominantly occur or are found in children and young individuals, while epidermoid cysts and dermatofibrosarcoma protuberans are more common in adults. This information can be useful for differential diagnosis.
In our study, pilomatricomas were mainly located on the face and neck, which is consistent with the reports by Solivetti et al.4 and Pelizzari et al.5 In contrast, dermatofibrosarcoma protuberans rarely occurs on the face and neck, as supported by Gong et al.,19 who reported that only 10% (4 out of 40) of dermatofibrosarcoma protuberans cases were located in the head and neck region. This information provides additional clues for differential diagnosis.
The description of echoic patterns of pilomatricomas in this study differed slightly from those in other studies. The reasons for this discrepancy may be the variation in inter-reader agreement and the definitions of different echogenicities. In this study, we adopted the definitions of different echogenicities in HFUS of the skin from the latest version of the “Position Statement,”16 which is expected to be more objective and precise.
There are some limitations to this study. The retrospective study design did not ensure that all HFUS and CDFI features of the lesions were recorded, which may have affected the characterization of different lesions. Only a small number of skin lesions were selected for the comparison study of pilomatricomas, and further studies with a wider range of skin diseases would enhance the robustness and rigor of feature characterization and conclusions.
In conclusion, pilomatricomas can be located in the cutaneous tissue, mimicking several other diseases. It is necessary to differentiate them from other skin lesions and focal lesions originating from the subcutaneous connective tissue and muscular tissue adjacent to the skin, and vice versa. The sonographic features of pilomatricomas are highly variable, but the main features include hyperechoic/isoechoic solid composition, scattered punctate foci, and posterior acoustic shadowing or no evident change, along with the presence of vascularity. Combining HFUS with CDFI to assess vascularity features can be valuable for the differential diagnosis of epidermoid cysts and dermatofibrosarcoma protuberans in adults.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.