Demographic and Fertility Characteristics of Contraceptive Clusters in Burundi
Abstract
Examining women's reproductive experiences over time reveals a more dynamic view of women's behaviors and needs than current status measures alone. This study uses sequence and cluster analyses, which are designed for identifying patterns and subgroups in longitudinal data. We apply these methods to contraceptive calendar data in Burundi to identify discrete clusters of women based on contraceptive and pregnancy behaviors over the past 5 years. We identify six unique clusters; three characterized by no use of contraception (85 percent of women) and three by use (16 percent). The Quiet Calendar cluster (42 percent) comprise women who neither experience pregnancy nor use contraception. Family Builder 1 (25 percent) and 2 (18 percent) both include women who experience two pregnancies, but differ in unmet need and lifetime experience with contraception. Modern Mother (8 percent), Consistently Covered Mother (6 percent), and Traditional Mother (2 percent) clusters differ by type of contraception used following pregnancy. Factors associated with cluster membership are need for family planning, lifetime experience with contraception, marital status, pregnancy intention, and age. This clustering approach provides a new, more holistic way to measure the diverse needs across unique subpopulations and can inform the development of multifaceted, adaptable strategies to meet women's dynamic fertility needs over the reproductive life course.
INTRODUCTION
Fertility remains high in Burundi, having only gradually declined from 6.9 children per woman in 1987 to 5.5 children per woman in 2016–2017 (MPBGP et al. 2017). Almost a quarter (23 percent) of married women aged 15–49 use a modern method—reflecting a small and gradual increase from 18 percent in 2010. Similarly, the demand for family planning has modestly increased from 54 percent in 2010 to 58 percent in 2016–2017. The modern contraceptive method mix is dominated by injectables (49 percent) and implants (26 percent) (Avenir Health 2018). Burundi is one of 69 priority countries that has made commitments toward FP2020 (Brown et al. 2014), but sluggish growth in contraceptive use suggests more effort is needed not only to meet the country's own family planning program targets for increased contraceptive prevalence but also to sufficiently meet women's needs. Three in 10 women in union have an unmet need for family planning (MPBGP et al. 2017). Analysis of modern contraceptive prevalence (mCPR) and ideal family size indicate current services are inadequate for meeting existing needs and that there is “room for additional growth in mCPR without changes in demand” (Avenir Health 2019; Track20 2018). A more nuanced investigation into patterns of women's contraceptive and fertility behaviors over time may provide new insights into opportunities to increase modern contraceptive prevalence and reduce unmet need in Burundi.
Demographic and Health Surveys (DHS) administer a retrospective contraceptive calendar as a part of most surveys. These calendars cover the 5 years preceding the survey. Calendar data have become the basis for much research on fertility behavior, including the calculation of discontinuation rates and other contraceptive dynamics (Ali, Cleland, and Shah 2012). These data provide a granular, month-by-month view of women's self-reported contraceptive use and pregnancy experience over time. Therefore, they have also been applied to the analysis of postpartum family planning (Moore et al. 2015), birth intervals (Moultrie, Sayi, and Timæus 2012), and perinatal mortality and pregnancy termination (Bradley, Winfrey, and Croft 2015).
Market segmentation researchers have tried to make cross-sectional data useful to reproductive health programs by identifying distinct, homogeneous groups within a population (i.e., market segments) that have different needs and inclinations to use contraceptive services. The aim of market segmentation is to tailor messages and services to distinct groups of potential and existing family planning clients who have different motivations to use or avoid services. Segmentation methods often use latent class analysis approaches on current status from cross-sectional data and tend to prioritize attitudes over behavior. As examples, several studies have found trust to be a motivating factor (Dabney et al. 2019; Dalglish et al. 2018). In Niger, groups of women were distinguished based on who did or did not “trust family planning and the health system,” while in Senegal and Uganda trust in peers facilitated service use. Meanwhile, others form segments based on positive views of contraception or gender attitudes (Wang et al. 2009; Dalglish et al. 2018; Camber Collective 2015). One study in the Philippines differentiated young “intenders” from low-income traditionalists and conventional skeptics (Wang et al. 2009).
Underutilized behavioral data on reproductive experiences can complement such attitudinal data, since behaviors may better reflect real-world facilitators and barriers that individuals face to carry out motivations and intentions. Thus, market segmentation researchers could also group women by observed behaviors, instead of distinguishing women by only attitudes, to tailor interventions. These observed reproductive behaviors are best captured by longitudinal data, such as those in DHS calendars, which can provide more insight on the details of contraceptive behavior and dynamics over time than can current status measures (MacQuarrie et al. 2014; Finnegan, Sao, and Huchko 2019). Unfortunately, latent class analysis and similar statistical techniques typically used in market segmentation are usually ill-suited to longitudinal categorical data. Instead, these methods are intended for the analysis of multiple factors measured at a single time point and are not optimized for repeated measures over time or sequences such as those found in longitudinal data where autocorrelation may be present.
However, sequence and cluster analysis methods can be used to identify patterns and subgroups using longitudinal, behavioral data (Aisenbrey and Fasang 2010; Dias and Willekens 2005; Furnas 2016; Gemmill 2019), facilitated by the availability of recent statistical packages (Gabadinho et al. 2011a; Studer 2013). These methods are designed for use with categorical sequence data in which the types and timing of transitions between states are an explicit analytical focus (Gabadinho et al. 2011a, 2011b). This makes these methods applicable to life course trajectories, such as career trajectories, relationship histories, and family formation processes (Aassve, Billari, and Piccarreta 2007; Furnas 2016; Gemmill 2019; Pollock 2007). Another advancement is ability to perform cluster analysis on weighted data, necessary when using complex survey data rather than census or simple random survey data (Studer 2013). We apply these methods to calendar data in Burundi.
This study identifies discrete subpopulations of women in Burundi based on patterns in their contraceptive and pregnancy experiences over time. We do not use typical cross-sectional measures, but instead put to new use retrospective, longitudinal data from the DHS contraceptive calendar. Specifically, we apply sequence and cluster analysis to identify discrete clusters that characterize women's dynamic contraceptive and pregnancy behaviors over the previous 5 years. We supplement the sequence data with additional demographic, fertility, and family planning data collected elsewhere in the survey to create a comprehensive profile of women in these clusters. To our knowledge, this is the first such application of these methods to nationally representative, longitudinal contraceptive use and pregnancy data.
Burundi is an appropriate setting in which to apply these methods for several reasons. First, a relatively high total fertility rate and contraceptive prevalence above 20 percent ensure that women's calendar sequences are likely to contain the experiences of interest. Second, prior quality assessments of contraceptive calendars in Burundi's surveys have shown them to yield reasonably reliable data on reproductive events (Bradley, Winfrey, and Croft 2015; MacQuarrie et al. 2018; Pullum and Staveteig 2017). Finally, continued investments and improvements in the policy and service context suggest governmental and nongovernmental actors may be positioned to incorporate evidence on women's needs and experiences to improve reproductive health programming (Kuang and Brodsky 2016; Track20 2015).
METHODS
Data
This study uses contraceptive calendar data from the 2016–2017 Burundi DHS, a survey representative at the national and subnational levels. Households are selected through a multistage, clustered sampling process in which enumeration areas are selected based on probability proportional to size and households are randomly selected within the selected enumeration areas. All eligible women in each household are selected for interview. The 2016–2017 Burundi DHS achieved an eligible woman response rate of 98.8 percent (MPBGP et al. 2017). These data are publicly available free of charge to researchers at https://dhsprogram.com/Data/.
The contraceptive calendar records monthly event data, or state data, including pregnancies, births, terminations, episodes of contraceptive use, and nonuse of contraception for the 5 years preceding the survey. Women's calendar sequences contain multiple states, reflecting as many of these events that women experience and their timing, duration, and sequence. These data are collected for all women of reproductive age (aged 15–49) in the 2016–2017 Burundi DHS (n = 17,269). We placed three restrictions on the data, namely restrictions on the period of observation, the number of states, and the age of women in the sample.
First, we omit the month of the interview and the two prior months, since some women who recently became pregnant may not yet recognize that they were pregnant, causing pregnancies to be underreported in the months closest to the time of interview. We observe exactly 59 months of data for each woman in her calendar sequence, with month 1 being the earliest point in the woman's calendar (approximately 5 years before the interview) and month 59 being the most recent month (three months before the interview).
-
No use of contraception
-
Use of a short-term, modern method of contraception
-
Use of a long-acting or permanent method (LAPM) of contraception
-
Use of a traditional method of contraception
-
Pregnancy, birth, or termination.
Short-term modern methods are pills, injectables, condoms, lactational amenorrhea method, emergency contraception, and the Standard Days Method. LAPM consist of intrauterine devices, implants, plus female and male sterilization. Traditional methods include periodic abstinence/rhythm, withdrawal, and other traditional or folkloric methods.
Third, we exclude women who were younger than aged 15 at the start of their calendar sequences. Prior research in Burundi indicates that the vast majority of girls this young are neither sexually active nor biologically fecund and seldom use contraception (MacQuarrie, Mallick, and Allen 2017; Pullum, Croft, and MacQuarrie 2018), so their calendar sequences would not have included the states most of interest to this analysis. Because we are interested in identifying distinct behavioral patterns present in the full population of women of reproductive age, we do not further restrict the analytic sample, such as by union status, sexual activity, or other factors. Our three restrictions yield a weighted analytic sample of 13,293 women.
Sequence and Cluster Analysis
In the first stage of analysis, we conduct sequence and cluster analysis in R using the TraMineR and WeightedCluster packages to identify primary clusters of contraceptive and pregnancy behavior (Alexis Gabadinho et al. 2011a; Studer 2013). All analyses are weighted to account for sampling probability, nonresponse, and the complex sampling design of the survey.
In the first stage of sequence analysis, we apply statistical tools to determine how similar each calendar sequence is to all other sequences in the dataset, that is, measuring pairwise distances, or differences, between pairs of sequences. We use optimal matching to calculate distances in our dissimilarity matrix, which (unlike Hamming distance-matching procedures) allows for states to be inserted and deleted as well as substituted in computing these distances. This flexibility allows us to better account for the sporadic timing of pregnancies in the sequences by potentially aligning these events over time. To measure pairwise distances between sequences, we use a constant cost matrix that assumes uniform costs for all substitutions, insertions, or deletions. Constant costs assume that the cost, or difficulty, of each transition between states are equal. For example, the difficulty of transitioning from using a short-term method to discontinuing it is equal to the difficulty of transitioning from not using a method to becoming pregnant.
Finally, we conduct cluster analysis to group together women whose calendar sequences exhibit similar patterns of contraceptive use and pregnancy experience (as measured by the dissimilarity matrix) using a k-medoid clustering algorithm (i.e., partitioning around medoids, or PAM). These parameters and the number of clusters in the final model were guided by scores on a series of six quality metrics (Gemmill 2019; Studer 2013). These are five metrics for which a higher score indicates a more optimal model: average silhouette width (weighted) (ASWw), Hubert's gamma (HG), point biserial correlation (PBC), pseudo R2 (R2), and the pseudo R2-squared (R2sq); and one metric (Hubert's C (HC)) for which a lower score indicates a more optimal model. Quality metrics are shown in Figures A1 and A2. The constant cost matrix performed equivalently to a transition rate cost matrix on four metrics and marginally better than the transition rate cost matrix on two metrics (R2 and R2sq). The k-medoid clustering algorithm performed better than an alternative, hierarchical (Ward's) clustering algorithm at all numbers of clusters, though the differences were negligible on two quality metrics (R2 and R2sq).
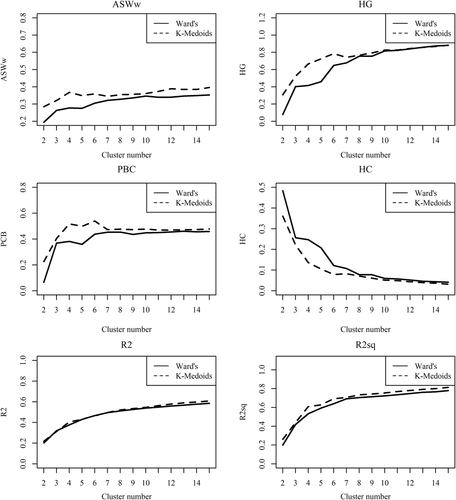
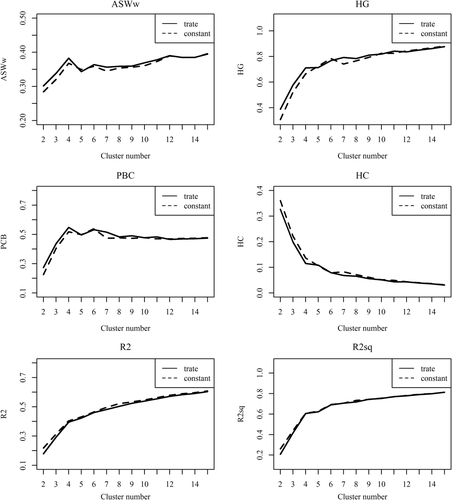
The presence of local peaks (high scores on the quality metrics at a given number of clusters) or troughs (in the case of the HC metric) led us to a final model with six clusters. A secondary local peak (or trough) is detected at four clusters on most of the quality metrics. However, this peak is not as high as the local peak at six clusters and would be insufficient to elaborate the full diversity of women's contraceptive experiences in their calendar experiences (by combining women into fewer clusters). The quality metrics also show diminishing returns to a model with more than six clusters.
These clusters group women solely on the basis of the contraceptive behaviors and pregnancy experiences observed in their 59-month calendar sequences. Each woman is assigned to a single cluster and no woman is omitted. Thus, each cluster contains women with similar features in their calendar sequences and clusters are differentiated from one another by specific defining features. We apply labels to these clusters based on these defining features. A consultative meeting was held among four researchers from the study team and three research colleagues from outside the study team to develop cluster names, based on consensus from their observations of the medoid (most representative) and range of calendar sequences that comprise each cluster. We use medoid plots and sequence index plots to visually describe the sequences in each cluster.
Regression Analyses
In the second stage of our analysis, we estimate multivariable logistic regression models separately for each of the six clusters to further elaborate on the demographic, fertility, and family planning experiences of women in those clusters. Multinomial models conducted for sensitivity analysis yielded similar results. We present the logistic regression results both for ease of interpretation and to allow for description of all six clusters (rather than setting one of the clusters as a reference cluster). These covariates complement the data contained in the calendar sequences upon which the clusters are identified. They describe a combination of experiences preceding, during, and immediately following the calendar sequence (at the time of the survey).
The main covariates in the regression models are age at the start of the calendar sequence in 5-year age groups (reference: aged 30–34), marital status at the time of survey (never in union (reference), currently in union, and formerly in union), number of children ever born (whether currently alive or not) at the start of the calendar sequence, need for family planning at the time of the survey (no need (reference), met need, or unmet need), experience of unintended pregnancy, and lifetime use of family planning. Use of either traditional or modern methods constitutes met need. Experience of unintended pregnancy describes women's experience at any point during the 5-year calendar or in the 3 months between the end of the calendar sequence and the time of the interview. Pregnancies are categorized as well-timed (wanted then (reference)), mistimed (wanted later), or unwanted (did not want any more), and did not experience a pregnancy during this time period. Lifetime experience of contraceptive use is a dichotomous variable expressing whether women report having ever used family planning. This variable is included in the regression models for the first three clusters only. It is omitted from the last three cluster models because, as will be shown, these clusters are characterized by contraceptive use and lifetime experience of contraception is, by definition, a characteristic of membership in these clusters.
Regression models also include socioeconomic variables as controls. These are rural/urban residence, educational attainment (none, primary, and secondary or higher), and household wealth quintile (based on an inventory of assets and housing materials in the household's possession at the time of the survey).
No causal direction is implied. Rather, regression models are used to identify associated attributes only. Regression analyses are conducted in Stata MP 16. All analyses are weighted to account for sampling probability, and nonresponse and svyset commands are used to account for the complex sampling design.
RESULTS
Sample Description
Table 1 presents the characteristics of women in the analytic sample, in terms of the factors in the regression models. The sample is relatively young, with the highest proportion aged 15–19 (24 percent) and the lowest proportion aged 40–44 (9 percent) at the start of the calendar sequence. Most women are currently married at the time of the survey (72 percent). About one-third of the sample had no children at the start of their calendars (34 percent). The remaining two-thirds are roughly evenly distributed (19–24 percent) across the other categories of one to two, three to four, or five or more children.
| Percentage | Weighted n | |
|---|---|---|
| Contraceptive cluster | ||
| Quiet Calendar | 41.5 | 5,521 |
| Family Builder 1 | 24.9 | 3,308 |
| Family Builder 2 | 18.1 | 2,400 |
| Modern Mother | 7.6 | 1,007 |
| Consistently Covered Mother | 5.6 | 750 |
| Traditional Mother | 2.3 | 308 |
| Age at the start of calendar sequence | ||
| 15–19 | 24.2 | 3,219 |
| 20–24 | 22.6 | 3,006 |
| 25–29 | 18.3 | 2,431 |
| 30-34 | 14.6 | 1,941 |
| 35–39 | 11.5 | 1,533 |
| 40–44 | 8.8 | 1,165 |
| Marital status at time of survey | ||
| Never in union | 17.3 | 2,293 |
| Currently in union | 71.6 | 9,512 |
| Formerly in union | 11.2 | 1,487 |
| Number of children at start of calendar sequence | ||
| 0 | 34.3 | 4,563 |
| 1–2 | 23.9 | 3,172 |
| 3–4 | 19.2 | 2,555 |
| 5+ | 22.6 | 3,003 |
| Experienced unintended pregnancy during or since calendar sequence | ||
| No pregnancy | 33.1 | 4,395 |
| Well-timed pregnancy | 42.6 | 5,661 |
| Mistimed pregnancy | 16.7 | 2,221 |
| Unwanted pregnancy | 7.6 | 1,016 |
| Need for family planning at time of survey | ||
| No need | 54.9 | 7,292 |
| Unmet need | 22.9 | 3,040 |
| Met need | 22.3 | 2,960 |
| Ever used family planning | ||
| No | 55.9 | 7,429 |
| Yes | 44.1 | 5,864 |
| Residence | ||
| Urban | 12.5 | 1,666 |
| Rural | 87.5 | 11,627 |
| Highest education level | ||
| No education | 44.8 | 5,955 |
| Primary | 36.8 | 4,896 |
| Secondary or higher | 18.4 | 2,441 |
| Household wealth quintile | ||
| Poorest | 20.3 | 2,696 |
| Poorer | 20.2 | 2,688 |
| Middle | 20.1 | 2,671 |
| Richer | 18.9 | 2,513 |
| Richest | 20.5 | 2,725 |
| Total | 100.0 | 13,293 |
Women have most commonly experienced a well-timed pregnancy (43 percent) during or since their calendar sequences, followed by experiencing no pregnancy (33 percent). Less common is experiencing an unintended pregnancy, with mistimed pregnancies (17 percent) exceeding unwanted pregnancies (8 percent). About half of the sample currently has no need for family planning, and one-quarter each experiences unmet need and met need for family planning. The majority (56 percent) has never used family planning.
The sample is largely rural (88 percent) and has either no education (45 percent) or primary education only (37 percent). The sample is evenly distributed across household wealth quintiles.
Contraceptive Clusters
We identify six distinct clusters, illustrated by their medoid—the most representative sequence for each cluster (Figure 1). The three most common clusters, including 85 percent of women, are characterized by no use of contraception while the remaining three clusters (16 percent of women) are characterized by contraceptive use. The six clusters are: (1) Quiet Calendar (42 percent), characterized by women who did not experience pregnancy or use any methods of contraception; (2) Family Builder 1 (25 percent) and (3) Family Builder 2 (18 percent), which are both characterized by women who did not use any method and experienced two pregnancies, but vary in terms of timing during the calendar sequence; (4) Modern Mother (8 percent), characterized by women who adopted short-term modern methods toward the end of year 2 after a period of nonuse and one pregnancy; (5) Consistently Covered Mother (6 percent), characterized by women who adopted LAPMs after a period of nonuse and one pregnancy; and (6) Traditional Mother (2 percent), characterized by those who adopted traditional methods at the end of year 2 after nonuse and one pregnancy.
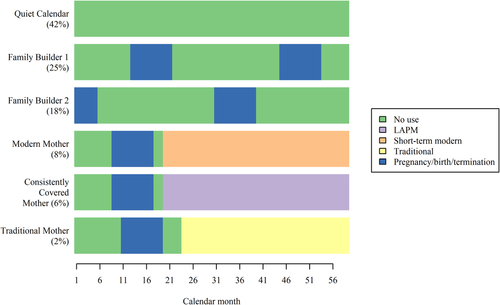
Sequence index plots show the individual sequences for every woman in each cluster (Figure 2). They show little deviation in sequences among members in each cluster when compared with the medoids. In aggregate, Quiet Calendar women spent an average of 56 months of the 59 months in a nonuse state, only 2.5 months in a state of pregnancy, and less than 1 month using short-term modern methods, LAPMs, or traditional methods. Women in the Family Builder 1 cluster spent an average of 37 months not using contraception and nearly 16.5 months in a state of pregnancy. Similarly, women in the Family Building 2 cluster spent an average of 42 and 14 months in these respective states. In both of these clusters, contraceptive use of any kind, combined, spanned less than 6 months on average.
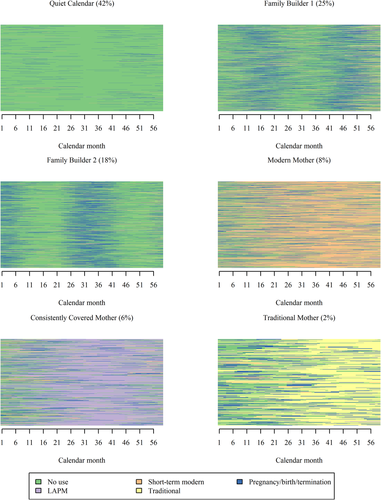
This contrasts sharply with the three clusters characterized by contraceptive use. A total of 36 months, on average, was spent using short-term modern methods in the Modern Mother cluster, 38 months using LAPMs in the Consistently Covered Mother cluster, and 34 months using traditional methods in the Traditional Mother cluster. The average time spent using no contraception in these three clusters ranges from 11 months (Consistently Covered Mother) to 13.5 months (Traditional Mother), and the average time in pregnancy ranges from 7 months to 10 months, respectively, with the remaining time spent using other contraceptive methods.
Demographic, Fertility, and Family Planning Attributes
The sequence and cluster analysis defined the six clusters described above on the basis of contraceptive use and pregnancy experience in women's 59-month calendar sequences, alone. Table 2 presents the results of separate logistic regression models, showing the demographic, fertility, and family planning experiences associated with membership in each of the six clusters.
| Quiet Calendar (42%) | Family Builder 1 (25%) | Family Builder 2 (18%) | Modern Mother (8%) | Consistently Covered Mother (6%) | Traditional Mother (2%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Odds ratio | p-value | Odds ratio | p-value | Odds ratio | p-value | Odds ratio | p-value | Odds ratio | p-value | Odds ratio | p-value | |
| Age at the start of calendar sequence (ref: 30–34) | ||||||||||||
| 15-19 | 0.86 | 0.282 | 1.35 | 0.011 | 0.85 | 0.182 | 0.98 | 0.907 | 1.70 | 0.022 | 0.21 | 0.000 |
| 20-24 | 0.54 | 0.000 | 1.32 | 0.006 | 0.95 | 0.635 | 1.08 | 0.667 | 1.97 | 0.000 | 0.63 | 0.082 |
| 25-29 | 0.65 | 0.000 | 1.24 | 0.015 | 1.02 | 0.796 | 0.99 | 0.943 | 1.30 | 0.071 | 0.77 | 0.209 |
| 35-39 | 1.48 | 0.001 | 0.85 | 0.103 | 0.98 | 0.866 | 0.74 | 0.037 | 0.84 | 0.288 | 0.85 | 0.477 |
| 40-44 | 4.20 | 0.000 | 0.24 | 0.000 | 0.84 | 0.314 | 0.51 | 0.001 | 0.45 | 0.000 | 1.25 | 0.426 |
| Marital status (ref: never in union) | ||||||||||||
| Currently in union | 0.12 | 0.000 | 6.09 | 0.000 | 1.07 | 0.745 | 3.20 | 0.000 | 7.14 | 0.000 | 7.02 | 0.001 |
| Formerly in union | 0.39 | 0.000 | 3.10 | 0.000 | 1.01 | 0.975 | 2.39 | 0.005 | 4.17 | 0.001 | 0.70 | 0.677 |
| Number of children at start of calendar sequence (ref: none) | ||||||||||||
| 1-2 | 0.54 | 0.000 | 1.03 | 0.765 | 1.09 | 0.267 | 1.55 | 0.008 | 4.05 | 0.000 | 0.84 | 0.535 |
| 3-4 | 0.58 | 0.000 | 1.09 | 0.409 | 0.87 | 0.181 | 1.53 | 0.027 | 5.83 | 0.000 | 0.89 | 0.704 |
| 5+ | 0.53 | 0.000 | 1.09 | 0.457 | 0.93 | 0.578 | 1.70 | 0.011 | 6.12 | 0.000 | 1.04 | 0.905 |
| Experience of unintended pregnancy during or since calendar sequence (ref: well-timed pregnancy) | ||||||||||||
| No pregnancy | 16.31 | 0.000 | 0.02 | 0.000 | 0.01 | 0.000 | 1.14 | 0.364 | 2.08 | 0.000 | 1.16 | 0.453 |
| Mistimed pregnancy | 0.27 | 0.000 | 1.75 | 0.000 | 1.05 | 0.521 | 0.62 | 0.000 | 0.83 | 0.198 | 1.56 | 0.015 |
| Unwanted pregnancy | 0.52 | 0.000 | 1.67 | 0.000 | 0.94 | 0.495 | 0.76 | 0.097 | 0.80 | 0.276 | 1.38 | 0.196 |
| Need for family planning at time of survey (ref: no need) | ||||||||||||
| Unmet need | 0.91 | 0.294 | 0.81 | 0.002 | 1.65 | 0.000 | 1.32 | 0.087 | 0.72 | 0.110 | 0.98 | 0.962 |
| Met need | 0.10 | 0.000 | 0.79 | 0.002 | 0.58 | 0.000 | 9.68 | 0.000 | 6.78 | 0.000 | 10.24 | 0.000 |
| Ever used family planning (ref: no) | ||||||||||||
| Yes | 0.20 | 0.000 | 1.37 | 0.000 | 0.73 | 0.000 | ||||||
| Residence (ref: urban) | ||||||||||||
| Rural | 1.15 | 0.241 | 1.25 | 0.007 | 0.85 | 0.133 | 0.62 | 0.001 | 1.19 | 0.320 | 0.77 | 0.239 |
| Education (ref: none) | ||||||||||||
| Primary | 1.03 | 0.703 | 1.03 | 0.680 | 1.04 | 0.460 | 0.92 | 0.414 | 0.87 | 0.214 | 1.40 | 0.072 |
| Secondary or higher | 1.82 | 0.000 | 1.03 | 0.810 | 0.68 | 0.005 | 0.75 | 0.067 | 0.87 | 0.544 | 1.80 | 0.012 |
| Household wealth index (ref: poorest) | ||||||||||||
| Poorer | 0.91 | 0.328 | 1.10 | 0.239 | 1.07 | 0.436 | 0.84 | 0.170 | 1.01 | 0.925 | 1.14 | 0.657 |
| Middle | 0.86 | 0.112 | 1.05 | 0.558 | 1.03 | 0.746 | 0.79 | 0.073 | 1.48 | 0.007 | 1.08 | 0.780 |
| Richer | 0.92 | 0.379 | 0.99 | 0.842 | 1.09 | 0.305 | 0.72 | 0.011 | 1.29 | 0.111 | 1.89 | 0.008 |
| Richest | 1.21 | 0.104 | 0.89 | 0.240 | 0.83 | 0.106 | 1.10 | 0.536 | 1.27 | 0.257 | 1.74 | 0.038 |
| Observations | 13,293 | 13,293 | 13,293 | 13,293 | 13,293 | 13,293 | ||||||
Quiet Calendar
Women in the Quiet Calendar cluster are typically not in their 20s at the start of their calendar sequences; rather they are either adolescents (aged 15–19) or older than aged 35, are never married, and have no children.
After controlling for socioeconomic variables, currently and formerly married women have 88 and 61 percent lower odds (p < 0.001), respectively, of being a member of the Quiet Calendar cluster than do never married women (Table 2). In other words, never married women have higher odds of belonging to the Quiet Calendar cluster. This pattern contrasts with that in most other profiles, in which either currently or formerly married women have higher odds of membership.
Women with any number of children at the start of their calendar sequences are significantly less likely to belong to the Quiet Calendar cluster than are women with no children, with similar odds (42–47 percent lower odds, p < 0.001) across each category. As with marital status, this pattern is unique to the Quiet Calendar cluster.
Women who have experienced no pregnancy during or following their calendar sequences have significantly higher odds of belonging to the Quiet Calendar cluster (OR = 16.3, p < 0.001). Similarly, women who have never used family planning in their lifetimes have 80 percent lower odds of being in the Quiet Calendar cluster than do women who have used family planning (p < 0.001). Quiet Calendar women are likely to have no need for family planning, as evidenced by 90 percent lower odds (p < 0.001) of membership among women with met need and no significantly different odds among women with unmet need. Further bivariate analysis reveals a striking lack of sexual activity in this cluster: 30 percent of Quiet Calendar women have never had sex and another 29 percent have not had sex in the previous 3 months. Additionally, 21 percent of women in this cluster report they are infecund or menopausal—rates more than 10 times higher than in any other cluster—and thus have no need for family planning.
In sum, the Quiet Calendar cluster lives up to its name, with constituent women having few reproductive experiences and no use of or need for family planning.
Family Builder 1 and Family Builder 2
Family Builder 1 and 2 resemble one another in that their representative sequences are characterized by no use of contraception and the experience of two pregnancies. They differ only in terms of the timing of the pregnancies within their sequences: Women in Family Builder 1 had their pregnancies more recently than Family Builder 2 women. The typical interbirth interval is also somewhat comparable in both clusters: a median of 31.9 months between the most recent two pregnancies for Family Builder 1 and 34.7 months for Family Builder 2. In spite of their similarities, women in these clusters differ along several other dimensions (Table 2).
The Family Builder 1 cluster consists of young women. The odds of membership are 24–35 percent higher for those younger than aged 30 (p < 0.05) and 76 percent lower for those aged 40–44 (p < 0.001) compared with the middle age group. Currently married women have six times the odds and formerly married women have three times the odds of belonging to the Family Builder 1 cluster compared with never married women (p < 0.001). Neither age nor marital status is associated with membership in the Family Builder 2 cluster.
Women who experienced unintended pregnancies during or since their calendar sequence have 1.7 to 1.8 times the odds (p < 0.001) of being in the Family Builder 1 cluster compared with women with well-timed pregnancies. This is not the case for women in Family Builder 2.
The Family Builder 1 cluster further consists of women who have no current need for family planning, as indicated by about 20 percent lower odds (p < 0.01) of cluster membership than women with either met or unmet need. In contrast, the odds of belonging to the Family Builder 2 cluster are lower (OR = 0.58, p < 0.001) among women with met need but 65 percent higher (p < 0.001) among those with unmet need (compared with those with no need). Women who have used contraception at some point in their lifetimes have 37 percent higher odds (p < 0.001) of being in the Family Building 1 cluster and 27 percent lower odds (p < 0.001) of being in the Family Builder 2 cluster.
Need for family planning, use of family planning, and experience of unintended pregnancies are the clearest dimensions by which membership in the Family Builder 1 and 2 clusters differ from one another.
Modern Mother
In general, the Modern Mother cluster consists of women who were unlikely to be older at the start of their calendar sequences and are likely to reside in urban areas, be currently or formerly married, and have had children at the start of their calendar sequences. Women are unlikely to be in this cluster if they had experienced an unintended pregnancy and have currently met their need for family planning.
Women older than aged 35 have reduced odds (p < 0.05) of being in the Modern Mother cluster compared with women aged 30–34. Meanwhile, currently married women have more than three times the odds (p < 0.001) of belonging to the Modern Mother cluster and formerly married women nearly two and a half times the odds (p < 0.01) compared with never married women.
The pregnancy recorded in a Modern Mother's calendar sequence is typically not her first. Women with either one to two children or three to four children at the start of their calendar sequences have about 1.5 times the odds (p < 0.05) of belonging to the Modern Mother cluster and women with five or more children have 1.7 times the odds (p < 0.05) of being in this cluster, compared with women with no children. Women who have experienced a mistimed pregnancy since the start of their calendar sequences (but not an unwanted one) have 38 percent lower odds (p < 0.001) of being in the Modern Mother cluster than women with a well-timed pregnancy in the past 5 years. Although having met need is associated with lower odds of membership in the Quiet Calendar and both Family Builder clusters, women with met need have 9.7 times the odds (p < 0.001) of being in the Modern Mother cluster when compared with their counterparts with no need.
Consistently Covered Mother
Overall, the Consistently Covered Mother cluster consists of currently and, to a lesser extent, formerly married women who have several children, have not experienced a pregnancy during or since their calendar sequence, and have had their current family planning needs met.
Compared with women aged 30–34, women younger than aged 24 have increased odds (p < 0.05) of membership in the Consistently Covered Mother cluster and women older than aged 40 have reduced odds (p < 0.001) of cluster membership. Currently and formerly married women have between four and seven times the odds (p < 0.001) of cluster membership compared with never married women. The odds of membership in the Consistently Covered Mother cluster increases steadily with the number of children born, ranging from four times higher among women with one to two children to more than six times higher among those with five or more (p < 0.001) children, when compared with women with no children.
Although LAPM use followed a pregnancy in the representative sequence for this cluster, women who had experienced no pregnancy have twice the odds (p < 0.001) of belonging to the Consistently Covered cluster than women with a well-timed pregnancy, when controlling for other factors in the model.
Having met need at the time of the survey is associated with 6.8 times higher odds (p < 0.001) of membership in the Consistently Covered Mother cluster than was having no need, although women with unmet need do not differ significantly from women with no need regarding cluster membership.
Traditional Mother
In general, the Traditional Mother cluster consists of nonadolescent women who are currently married and whose need for family planning is being met. Adolescent women aged 15–19 have 79 percent lower odds (p < 0.001) of membership in the Traditional Mother cluster than do women in the middle age group. Currently married women have seven times the odds of belonging to the Traditional Mother cluster compared with never married women, though no association is detected for formerly married women. The odds of belonging to the Traditional Mother cluster are 10.2 times higher (p < 0.001) for women with a met need for family planning than for those who have no need and 1.6 times higher (p < 0.001) among those who have had a mistimed pregnancy compared to a well-timed pregnancy.
Age, Unmet Need, and Cluster Membership
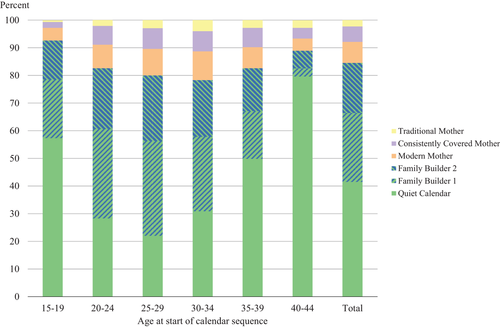
As shown in Table 2, the Quiet Calendar cluster has a distinctive age pattern when compared with other clusters. The bivariate distribution of clusters across age groups, presented in Figure 3, further illustrates this finding. It shows that the Quiet Calendar cluster is commonly experienced by both adolescent and older women. In contrast, in the Family Building clusters and those characterized by contraceptive use, the prevalence of membership increases with age until it begins to decrease again in a middle (Family Builder clusters) or older (all three contraceptive clusters) age group.
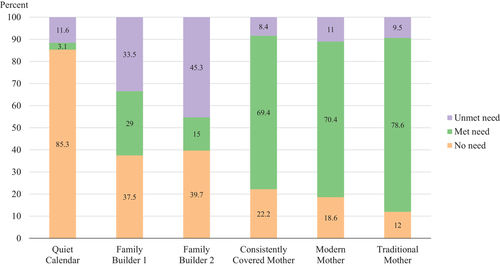
Unmet need is a significant factor for predicting membership in each cluster, as shown in Table 2. The results of bivariate analysis of need status, distributed across the six clusters (Figure 4), complements the results of the multivariate analysis presented in Table 2. They reiterate that women with no need for family planning are concentrated in the Quiet Calendar cluster and are least likely to belong to the clusters characterized by contraceptive use. Unmet need is highest in the two Family Builder clusters, while met need is most prevalent in the three contraception clusters. Although total levels of need are similar in the two Family Builder clusters, unmet need is substantially greater in the Family Builder 2 cluster than in the Family Building 1 cluster.
DISCUSSION
This study identified six unique clusters of reproductive behavior in Burundi, three of which are characterized by contraceptive use and three of which are characterized by the absence of contraceptive use. This study further identified demographic, fertility, and family planning attributes associated with membership in these clusters.
A large majority of women (85 percent) belong to one of the noncontraception clusters, with a minority (16 percent) belonging to one of the three contraceptive clusters. These findings are consistent with estimates of current contraceptive use in other studies of Burundi (Avenir Health 2018; Ba et al. 2019). Factors most consistently associated with cluster membership are need for family planning, lifetime experience of contraceptive use, marital status, pregnancy experience, and age. The number of children ever born at the start of a woman's calendar sequence is associated with membership in only half of the clusters: Quiet Calendar, Modern Mother, and Consistently Covered Mother. Cluster membership is seldom differentiated by socioeconomic variables.
The Quiet Calendar stands apart from the other clusters in many ways: Along with no use of contraception over the past 5 years, Quiet Calendar women are unmarried, have no children or pregnancies, no need for family planning, and no history of contraceptive use. The size of this cluster (42 percent) may be a surprise in a high fertility setting such as Burundi. Although we understand that fertility desires and associated behavioral patterns are dynamic (e.g., Bernardi, Mynarska, and Rossier 2015; Speizer and Lance 2015)—and this study's own data indicate both dynamism within most clusters and that women likely move between clusters at different points in their lives—the Quiet Calendar cluster is an exception. The steady lack of activity over an extended period of time (5 years) is striking. It suggests that health programs may need to reconsider ways to reach women with no imminent need for family planning or maternal health services to make sure they still have the access they need for general preventive and curative health care.
The two noncontraception clusters that are characterized by family building, Family Builder 1 and 2, appear at first glance to be nearly identical, differing only by the timing of the pregnancies relative to the time of interview. The choice to use optimal matching over Hamming matching parameters was made because it minimizes these types of differences between sequences that can be resolved simply by realigning events, for example, offsetting the Family Builder 1 sequences to the left or Family Builder 2 to the right. Nonetheless, this similarity raises the question as to whether their identification as separate clusters is an anomaly of the statistical procedures used and based on sampling variance in the times at which women were interviewed relative to their pregnancies, or whether they are indeed programmatically meaningful, distinct groups of women. The regression analyses in this study support the latter conclusion.
Women in Family Builder 1—the cluster in which the experience of two pregnancies is more recent—experience unintended pregnancies to a greater extent than women in Family Builder 2. They also tend to have no need (neither met nor unmet) for family planning at the time of the survey and have lifetime experience using contraception. In contrast, Family Builder 2 women generally experience unmet need and have never used contraception. Family Builder 2 is characterized by women who have less experience with contraception, either are not using or do not intend to use contraception and have current unmet need for family planning. These findings comport with those of additional analyses indicating that Family Builder 1 women articulate more clearly defined fertility intentions at the time of the survey than do Family Builder 2 women and are more likely than Family Builder 2 women to participate in joint contraceptive decision making (Juan, Allen, MacQuarrie, Juan, and Gemmill 2020). These findings also signal that a certain degree of ambivalence about fertility intentions is possible in the Family Builder 2 cluster, suggested by nonnumeric responses to ideal number of children and a disconnect between a stated desire to delay or avoid subsequent childbearing alongside no intention to use contraception (MacQuarrie, Juan, and Gemmill 2020). In sum, Family Builder 1 women are inclined to use contraception at points in their lives when they need it but are presently focused on having children, although they have struggled with planning the timing of childbearing. For women in Family Builder clusters that have unmet need for family planning, health programs should play a critical role in supporting women in their pursuit of their preferred contraceptive methods, including during the postpartum period.
The three contraceptive clusters are each characterized by the type of contraception used—short-term modern methods, LAPMs, or traditional methods. Interestingly, women in these clusters are not segmented based on other dimensions of contraceptive behavior, such as discontinuation, experimentation or switching among methods, timing of method adoption, or interruptions in or continuity of use. Further, for each cluster based on type of contraception, the medoid sequence indicates adoption of contraception part way into her sequence rather than at the start of the sequence. This may be partly due to the optimal matching algorithm, which aligns events over time, and because births were more common earlier in sequences than was contraceptive use. This also comports with trends in the direction of increasing contraceptive prevalence over time in Burundi (MPBGP et al. 2017). However, it contrasts with other research indicating that discontinuation and switching are important features of women's contraceptive experiences (Ali, Cleland, and Shah 2012; Finnegan, Sao, and Huchko 2019). These aspects of contraceptive behavior may be obscured because we analyze data from the general population of all women of reproductive age, rather than the minority of women who are contraceptive users.
In addition, we identify no clusters in which contraception is used for spacing between pregnancies. In both Family Builder clusters, it is characteristic not to use contraception between pregnancies. In all three contraceptive clusters, contraceptive use follows the experience of pregnancy. This reiterates findings from another study indicating that women's pregnancy experiences predict subsequent contraceptive behavior in Burundi, suggesting that most women in Burundi only use contraception regularly after experiencing pregnancy (Bakibinga et al. 2016). The degree of pregnancies in these clusters and the two Family Builder clusters both reflects the high fertility in Burundi (Gerland, Biddlecom, and Kantorová 2017; MPBGP et al. 2017) and highlights the importance of continued investment in maternal health services and postpartum family planning (Track20 2018).
Women in these three contraceptive clusters are currently meeting their need for family planning and (particularly for women in the Modern Mother and Consistently Covered Mother clusters) are unlikely to have experienced an unintended pregnancy. Although Modern Mother and Consistently Covered Mother women have had children prior to their calendar sequences (especially Consistently Covered Mothers), this is not so for Traditional Mothers, suggesting that life course factors also differentiate membership in contraceptive clusters (CT Innovation Lab 2018; Wang et al. 2009). Programs should continue supporting women in these clusters by ensuring that family planning needs are met at all stages of the reproductive life course.
The results from this study can inform the development of multifaceted and adaptable strategies to meet women's dynamic fertility needs over the reproductive life course. For example, our study population was distinctly stratified by history of contraceptive use and pregnancy. Based on these two dimensions alone, providers could feasibly tailor messaging or other types of interventions to enhance women's contraceptive use and autonomy. Indeed, descriptive studies such as ours reiterate that programs and providers should strive to diversify approaches that meet women where they are. The clusters described in this study are compatible with behavioral analysis tools like the “Think | BIG Tool,” which links behavioral profiles to programmatic strategies and identifies gaps in such programming (The Manoff Group 2020).
Moreover, future research can use our methodological approach to conduct analyses on select subpopulations; doing so might yield different and more nuanced patterns compared to those we observe here, which are based on all women of reproductive age. For example, applying this approach to a limited subsample of women whose sequences begin with contraceptive use may reveal interesting patterns in discontinuation, method switching, or use of contraception for spacing pregnancies. Overall, our results suggest that by highlighting the lived complexities of women's reproductive and contraceptive experiences, family planning programs can more effectively engage precision public health and medical practices that “deliver the right interventions to the right people at the right time” (The Rockefeller Foundation and WHO 2021).
The study has several limitations to note. First, we used a condensed set of five states. Analyzing all 18 contraceptive methods as separate states would have been too many states to easily interpret the results and would have increased computational complexity. Instead, we grouped types of contraceptive methods together as traditional; modern, short-term; and LAPM. Grouping contraceptive methods in this manner has two implications. First, it rests on the assumption that transitions within one type of contraception (e.g., from pill use to injectables) is less meaningful than transitions across types (e.g., from pill use to IUD use). While these categories are a common way to classify contraceptive methods, we did not test this empirically. One approach to testing this empirically would be to expand the number of contraceptive method states but restrict the sample to those women belonging to one of the three clusters defined by contraceptive use, to see if the same three clusters emerge or if additional clusters are revealed representing important variations within one or more of the three original clusters.
Similarly, and for the same reasons, we condensed pregnancies and their outcomes into a single “pregnancy, birth, or termination” state. We do not distinguish pregnancy states from their outcomes. There are firm empirical grounds for doing so, as every pregnancy transitions into a birth or termination. Grouping them together allows a focus on the transitions from pregnancy (and the outcome) into the postpartum contraceptive use or nonuse states. However, doing so obscures potential important differences in sequences containing pregnancies that result in live births from those that result in a nonlive birth outcome. A fruitful area for further analysis may be to explicitly examine, among women with pregnancies, the subsequent sequences of those who experience live and nonlive birth outcomes. It is also important to note that most DHS contraceptive calendars cannot differentiate types of termination, that is, miscarriage, induced abortion, or still birth.
A second implication of reducing the number of states is that we reduce the total number of transitions we are able to observe in any sequence. This may make it appear as if women's 5-year contraceptive histories are more stable and less dynamic than they may actually be.
In addition, our analysis of calendar sequences may be subject to the reliability of DHS calendar data. Assessments of calendar instruments, administered in DHS and non-DHS surveys, suggest that there may be some underreporting of contraception or pregnancies not ending in a live birth, or their timing could be misreported and that such errors are concentrated in the earliest periods of the calendar, among users of coital methods or of short duration, and among women with complex reproductive histories (Bradley, Winfrey, and Croft 2015; MacQuarrie et al. 2018; Tumlinson and Curtis 2021). In this study, type of contraception was more important to distinguishing clusters than was timing or duration of use—the dimensions most subject to reliability issues. Further, clusters based on contraceptive use comprise a minority of the sample. While there may be some misclassification of women into a cluster, threats to inference are likely minimal.
In this study, we successfully applied new sequence and cluster analysis techniques to DHS contraceptive data. This opens up an array of research questions to which these methods could be applied. In our study, we did not align women's sequences to start with a key reproductive or demographic event; rather we aligned women's sequences to be of equal length, all starting 62 months prior to the interview. Other research questions may require different analytical choices. For example, analysis of clustered patterns in postpartum adoption of contraception may allow sequence length to vary but align sequences to begin with a birth or the most recent birth. Analysis of patterns of first contraceptive use may align sequences to begin with marriage or the first birth or some other beginning “marker.” These analytical choices may be somewhat analogous to the choices required in other methods used with longitudinal data, such as survival analyses.
This study took an innovative approach to segmenting women, not based on current contraceptive status and attitudes, but based on their contraceptive and pregnancy behaviors over the past 5 years. This represents a new use of DHS calendar data and offers a new, dynamic perspective on women's reproductive health. This study also elaborated on the demographic, family planning, and fertility attributes associated with women in each of six discrete clusters of women in Burundi. In so doing, it provides a more holistic profile of women's behaviors and needs and can provide reproductive health programs with unique insights on the clientele they seek to serve. While the patterns we identify in Burundi are likely to differ from those to be found in other contexts, this approach to identifying unique subpopulations of women can be applied in any number of settings with contraceptive calendar data.
Open Research
Data Availability Statement
Standard recode datafiles for the 2016–2017 Burundi Demographic and Health Survey are made publicly available at https://dhsprogram.com/Data/.
References
ACKNOWLEDGMENTS
This work was supported by the U.S. Agency for International Development (USAID) under contract #720-OAA-18C-0083. The authors extend their appreciation to Minki Chatterji, National Institute on Drug Abuse, National Institutes of Health, and Mengjia Liang, United Nations Population Fund (UNFPA), for thoughtful comments on an earlier draft.