Nasal obstruction and male gender contribute to the persistence of mouth opening during sleep in CPAP-treated obstructive sleep apnoea
Abstract
Background and objective
During continuous positive airway pressure (CPAP) treatment, some patients with obstructive sleep apnoea syndrome (OSAS) require an oronasal mask (ONM) to prevent excessive mouth leakage. Factors contributing to sleep-related mouth opening under CPAP treatment remain known. We compared mouth opening during sleep in patients treated with CPAP by nasal mask (NM) versus ONM.
Methods
Cross-sectional prospective study: patients treated with CPAP for at least 4 months underwent a sleep recording using a type 4 monitoring device (Brizzy-Nomics) that records mouth opening via a magnetometric distance meter. Clinical assessment included anthropometry, smoking status and the Mallampati score. Nasal obstruction was assessed by the Nasal Obstruction Symptom Evaluation questionnaire.
Results
Thirty-eight patients were included, 34 analysed (22 men; age = 57.4 (53; 62) years; body mass index = 32.6 (29.1; 35.2) kg/m2; median (25th; 75th)). Twenty-seven patients were treated with NM and seven with ONM. Patients with ONM were more often active smokers and trended to have greater nasal obstruction and lower forced expiratory volume in 1 s. They also exhibited a greater mouth opening during sleep (median (25th;75th) = 13.0 (11.0; 15.0) vs 6.0 (5.0; 10.0) mm, P < 0.001) and a higher oxygen desaturation index (9.5 (6.2; 15.5) vs 2.9 (1.0; 6.1) events/h, P = 0.009). In multivariate analysis, male gender and nasal obstruction were independently associated with mouth opening under ONM CPAP treatment.
Conclusions
After several months of CPAP treatment, some patients using ONM persist in keeping their mouths open at night. Nasal obstruction and male gender contribute to this phenomenon.
Abbreviations
-
- AHI
-
- apnoea–hypopnoea index
-
- CPAP
-
- continuous positive airway pressure
-
- FEV1
-
- forced expiratory volume in 1 s
-
- ONM
-
- oronasal mask
-
- OSAS
-
- obstructive sleep apnoea syndrome
-
- PSG
-
- polysomnography
-
- SpO2
-
- pulse oxygen saturation
Introduction
Continuous positive airway pressure (CPAP) is the first-line treatment for moderate to severe obstructive sleep apnoea (OSA).1 CPAP adherence is crucial for improvement of symptoms2 and to reduce cardio-metabolic consequences.3 Adherence depends on several mechanisms such as the self-perceived benefit/inconvenience ratio, social status,4 depressive status and technological aspects. Among this latter, the type of mask may impact on CPAP adherence.5 The choice of the mask is essential for CPAP treatment to be successful.
Nasal masks are most commonly used.6 Oronasal masks, covering the nose and mouth, are usually offered either as a second choice when patients report mouth leaks during CPAP treatment with a nasal mask or immediately when patients have severe nasal obstruction or report sleeping with their mouth open.7
There is a close link between obstructive sleep apnoea–hypopnoea syndrome and mouth breathing during sleep. During an obstructive respiratory event, respiratory effort increases and recruitment of supra-hyoid muscles, mylohyoid, geniohyoid and genioglossus cause mouth opening, which is not compensated by the jaw closing muscles, masseter, internal pterygoid and temporalis.8, 9 Mouth opening in turn induces mandibular retrusion, decreases pharyngeal diameter,10 reduces the mechanical efficiency of the pharyngeal dilator muscles11 and increases pharyngeal resistance and collapsibility.12
CPAP treatment with a nasal mask, by alleviating pharyngeal obstructions, reduces sleep time spent in mouth breathing13, 14 as well as the amplitude of mouth opening movements.15 However, some patients report mouth leaks under nasal CPAP suggesting the persistence of mouth opening during sleep and require an oronasal mask. In clinical practice, oronasal masks is offered about 25%5 of patients treated with CPAP and are often suggested after a few days or weeks of nasal CPAP treatment. The proportion of sleep time spent with the mouth open is usually not documented. The choice of an oronasal mask is based on patient's self-reported symptoms particularly dry mouth, the level of leaks observed with CPAP built-in software and the clinical impression. When an oronasal mask is prescribed, a switch back to a nasal mask is rarely envisaged, implying that mouth opening and mouth leaks may be a long-term condition. However, it has been recently shown that symptoms such as dry mouth and leaks can evolve during treatment with CPAP.16 Moreover, factors contributing to persistent mouth opening under CPAP remain relatively unknown.
In this context, the main objective of this cross-sectional study was to compare mean mouth opening during sleep in patients with obstructive sleep apnoea syndrome treated with CPAP for several months by nasal and oronasal masks. The secondary objective was to identify independent characteristics of patients with persistent mouth opening during CPAP therapy.
Methods
This was a cross-sectional prospective study. Our institutional review board (IRB-6705) approved this study, and all patients included signed written informed consent.
Study participants
Between February and May 2014, patients (aged ≥18 years) with moderate to severe obstructive sleep apnoea syndrome (OSAS) followed by our sleep clinic and fulfilling the following criteria were asked to participate: (i) patients treated at home exclusively with auto-adjusted CPAP for at least 4 months; (ii) using a nasal mask or oronasal mask; and (iii) objective CPAP adherence obtained from built-in time counters in the CPAP devices of greater than 3 h/night.
Study procedures
Recording during sleep
All included patients underwent a single-night sleep recording under CPAP at home using a type 4 monitoring device (Brizzy Nomics, Liege, Belgium).17 This device records blood oxygenation (pulse oxygen saturation (SpO2), body position, mandible position and mandible movements. Patients used their own mask. Data of the 95th percentile pressure and non-intentional leaks L/min were also downloaded from the CPAP device (S9 Autoset RESMED, Sydney, Australia).
Clinical assessment
OSAS severity, lung function and arterial blood gas values just before starting CPAP were collected from patient's medical charts.
Anthropometric data (weight, height, neck and waist circumferences), smoking status and the Mallampati score were recorded. Nasal obstruction was assessed by the validated French version of the Nasal Obstruction Symptom Evaluation (NOSE) questionnaire. NOSE is an auto-questionnaire consisting of five items each scored using a 5-point Likert scale from 0 to 20. The total score represents the sum of the responses to the five items and ranges from 0 to 100.18 Higher scores indicate greater obstruction.
Determination of mouth opening and mandible movements
A mid-sagittal mandibular movement magnetic sensor (Brizzy Nomics, Liege, Belgium) measured the distance between two parallel, coupled, resonant circuits placed on the forehead and on the chin (Fig. 1). The transmitter generated a pulsed magnetic wave of low energy at 10 Hz. The change in the magnetic field recorded at the receiver is inversely related to the distance between the chin and forehead probe. The resolution of the measurement was 0.1 mm. The signal was interpreted as follows: the greater the value of the signal, the lower the mandible position, reflecting wider opening of the mouth. Mandible behaviour has been shown as a reliable marker of respiratory effort during sleep.19 An automatic analysis of mandible movement has been previously developed for the scoring of apnoea-hypopnoea events,9, 20, 21 the scoring of sleep/wake phases22, 23 as well as micro-arousals.21 In the present study, the automatic analysis of this signal was used to assess (i) the mean value of mouth opening over the entire sleep period and (ii) the mean amplitude of the mandible oscillation. The mandibular movement signal was expressed as an absolute value (mm).
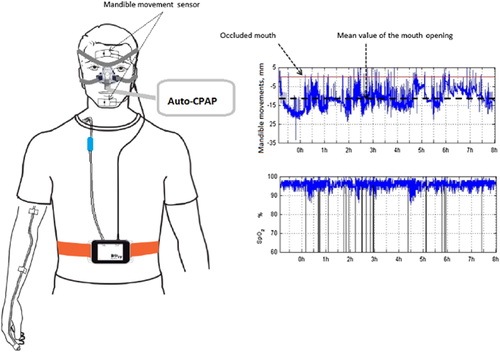
Schematization of the type 4 monitoring device (Brizzy Nomics, Liege, Belgium) used for sleep recording under continuous positive airway pressure (CPA ) at home. The device includes (i) two sensors placed on the median line of the face on the forehead and on the chin; the mandible movement signal corresponds to the distance between the two sensors; (ii) oximeter; (iii) body position.
Sample size
Since no published data were available, we hypothesized that patients treated with CPAP+ oronasal mask had the same mean mouth opening during sleep as OSAS patients without CPAP. Senny et al.15 showed that the mean mouth opening in OSAS patients decreased from −9.1 ± 3.5 mm (mean ± standard deviation) in spontaneous breathing to −5.8 ± 3.5 mm under nasal CPAP. Considering such differences in mouth opening between patients who had a nasal mask versus patients who had an oronasal mask, a total number of 36 patients had to be included to show a significant difference (alpha = 0.05, power = 80%).
Statistical analysis
Data were analysed using Statistical Analysis System (SAS) software version 9.1.3 (SAS Institute, Cary, NC, USA). Continuous data were expressed as median (25th; 75th percentiles) and categorical data as percentage.
Differences in characteristics between patients who had a nasal mask and those who had an oronasal mask were tested using chi-square or Fisher Exact tests for categorical data and Mann–Whitney non-parametric tests for continuous data. To take into account the risk of multiple comparisons, results are also presented with and without Holm–Bonferroni correction.24
To achieve the secondary objective of identifying the independent characteristics linked with mouth opening, two steps were used: (i) univariate linear regression models were used to determine variables associated with mean mouth opening; (ii) variables associated with mouth opening (with a P-value < 0.1) were introduced into a stepwise selection procedure in multivariate linear regression models. Before the stepwise selection, co-linearity between variables (defined r > 0.4) was verified by Pearson's or Spearman's coefficient or Cramer's V.
Results
Patients' characteristics
Fifty-five patients were asked to participate; 17 patients declined, 38 were included. Three patients were excluded because they were treated with fixed CPAP; two patients had an oronasal, one a nasal mask. The nocturnal recording was lost for one patient (nasal mask). The analysis was performed on 34 patients, 27 treated with a nasal mask, seven with an oronasal mask. At inclusion, the duration of CPAP treatment for the whole group was 7.5 (6; 9.7) months (median (25th; 75th)) (Table 1).
| Whole group (n = 34) | Nasal mask (n = 27) | Oronasal mask (n = 7) | P-value* | P-value** | |
|---|---|---|---|---|---|
| Anthropometry | |||||
| Age (years) | 57.5 (53.0; 62.0) | 58.0 (51.0; 62.6) | 57.00 (54.9; 61.1) | 0.798 | 1.0 |
| Gender (% males) | 64.7 | 59.3 | 85.7 | 0.378 | 1.0 |
| BMI (kg/m2) | 32.6 (29.1; 35.2) | 32.1 (28.3; 34.6) | 33.90 (29.1; 38.1) | 0.580 | 1.0 |
| Neck circumference (cm) | 43.0 (39; 44) | 42.5 (38; 44) | 43.0 (40; 50) | 0.479 | 1.0 |
| Waist circumference (cm) | 114 (107; 123) | 113 (107; 121) | 123.00 (104; 127) | 0.332 | 1.0 |
| Mallampati score | 0.644 | 1.0 | |||
| ≤2 (%) | 73.5 | 73.4 | 85.7 | ||
| ≥3 (%) | 26.5 | 26.6 | 14.3 | ||
| Active smoking (%) | 5.9 | 0 | 28.6 | 0.037 | 0.296 |
| NOSE score (0–100) | 13 (5; 50) | 10 (5; 40) | 55 (15; 55) | 0.078 | 0.546 |
| Respiratory function | |||||
| FEV1 (% predicted value) | 106 (94; 116) | 107 (103; 119) | 100 (76; 108) | 0.074 | 0.296 |
| FEV1/FVC | 83 (76; 88) | 84 (76; 89) | 80 (73; 84) | 0.180 | 0.540 |
| PaO2 (mm Hg) | 83 (77; 90) | 83 (78; 90) | 86 (78; 87) | 0.880 | 1.0 |
| PaCO2 (mm Hg) | 36 (33; 39) | 36 (33; 39) | 36 (34; 41) | 0.530 | 1.0 |
| Sleep apnoea severity (at diagnosis) | |||||
| AHI (events/hour) | 45 (35; 74) | 44 (35; 80) | 58 (33; 70) | 0.898 | 1.0 |
| Mean nocturnal SpO2 (%) | 92.0 (91.0; 94.0) | 92.2 (91.0; 94.0) | 90.8 (89.2; 92.0) | 0.032 | 0.096 |
| Epworth Sleepiness Scale (0–24) | 9 (7; 12) | 9 (7; 12) | 9 (6; 16) | 0.847 | 1.0 |
| Characteristics of CPAP treatment | |||||
| CPAP adherence (h/night) | 6.4 (4.5; 7.4) | 6.4 (4.5; 7.4) | 6.2 (4.0; 8.2) | 0.814 | 0.815 |
| Additional heated Humidification (%) | 38 | 22 | 100 | <0.001 | 0.001 |
- *P-value = Comparison between nasal mask versus oronasal mask; **P-values represent P-values with Holm–Bonferroni correction for multiple comparisons.
- Continuous data were expressed as median (25th; 75th) and categorical data as percentage.
- AHI, Apnoea–Hypopnea Index; BMI, body mass index; FEV1 (% predicted value), forced expiratory volume in 1 s expressed in percentage of predicted value; FVC, forced vital capacity; NOSE Score, Nasal Obstruction Symptom Evaluation score.
Anthropometric variables were comparable among patients treated with oronasal and nasal masks. Although sleep apnoea severity, estimated by the apnoea–hypopnoea index (AHI), was comparable in both groups, mean nocturnal SpO2 during spontaneous breathing at the time of diagnosis was lower in patients treated with an oronasal mask. Patients treated with an oronasal mask tended to have greater nasal obstruction and a lower FEV1.
All patients but one treated with oronasal mask had been initiated to CPAP with a nasal mask and have been changed to an oronasal mask between 7 and 232 days of treatment. The patient who was immediately treated with oronasal mask, reported chronic nasal obstruction and oral breathing during sleep; his NOSE score at inclusion was high (60/100). In the six remaining patients, four patients reported two symptoms or more which provide a rationale for switching from nasal to oronasal mask (Table 2).
| Patient no. | Persistent upper airway dryness | Leaks | Nasal obstruction | Mouth opening |
|---|---|---|---|---|
| 1 | — | Yes | Yes | — |
| 2 | Yes | Yes | Yes | Yes |
| 3 | Yes | Yes | — | Yes |
| 4 | — | Yes | — | — |
| 5 | — | — | Yes | Yes |
| 6 | — | — | — | Yes |
| 7 | — | — | Yes | Yes |
- Patient 7 received an oronasal mask from the beginning of treatment with auto-CPAP. CPAP, continuous positive airway pressure.
All patients with oronasal masks needed additional heated air humidification compared to 22% of patients with nasal masks, CPAP adherence was equivalent in both groups.
Features of sleep recording under CPAP according to the type of mask
Figure 2 shows features of the sleep recording according to the type of mask. Patients treated with oronasal mask had greater mean mouth opening during the night (a). Additionally, the oxygen desaturation index (at 3%) was higher in patients with oronasal masks than in patients with nasal masks (c) although the 95th percentile pressure was not different in the two groups (e). Non-intentional leaks tended to be more important in patients with oronasal masks (f).
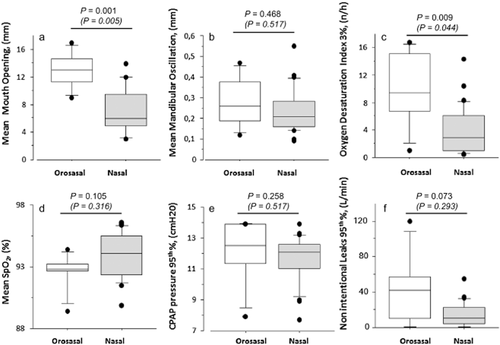
Features of sleep recording according to the type of mask. Differences between patients who had a nasal mask and those who had an oronasal mask were tested using Mann–Whitney non-parametric tests. P-values represent P-values with Holm–Bonferroni correction for multiple comparisons.
Patients' characteristics linked with mouth opening
Table 3 and Figure 3 show the characteristics that were associated with mean mouth opening. Male gender, active smoking, nasal obstruction, neck circumference and lower FEV1 were significantly associated with mouth opening during sleep.
| Regression coefficient | 95% CI | P-value | |
|---|---|---|---|
| Age | 0.00 | (−0.13; 0.14) | 0.997 |
| Gender (male vs female) | 4.53 | (2.14; 6.92) | <0.001 |
| BMI | 0.02 | (−0.26; 0.31) | 0.800 |
| Active smoking (yes vs no) | 5.56 | (0.03; 11.1) | 0.049 |
| Neck circumference | 0.41 | (0.13; 0.13) | 0.006 |
| Waist circumference | 0.07 | (−0.03; 0.18) | 0.146 |
| Mallampati score (3;4 vs 1;2) | −2.63 | (−5.62; 0.37) | 0.083 |
| FEV1 | −0.09 | (−0.16; −0.01) | 0.022 |
| FEV1/FVC | −0.11 | (−0.23; 0.002) | 0.055 |
| PaO2 | −0.05 | (−0.18; 0.07) | 0.394 |
| PaCO2 | −0.03 | (−0.32; 0.26) | 0.831 |
| NOSE Score (≥50 vs < 50) | 4.02 | (1.24; 6.81) | 0.006 |
| AHI | −0.02 | (−0.07; 0.04) | 0.576 |
| Epworth Sleepiness Scale | −0.002 | (−0.34; 0.33) | 0.989 |
- AHI, Apnoea–Hypopnea Index; BMI, body mass index; CI, confidence interval; FEV1 (% predicted value), forced expiratory volume in 1 s expressed in percentage of predicted value; FVC, forced vital capacity; NOSE Score, Nasal Obstruction Symptom Evaluation score.
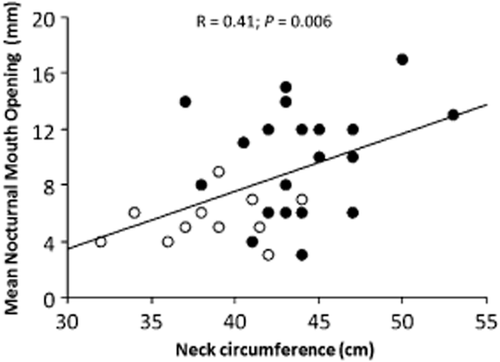
Linear regression between mean mouth opening (expressed in mm) and Neck Circumference (expressed in cm). Open circles = women (one missing data); Black circles = men
In multivariate analysis (Table 4), male gender and nasal obstruction remained independently associated with mouth opening during sleep.
| Variables | Regression coefficient | 95% CI | P-value |
|---|---|---|---|
| Gender (male vs female) | 4.442 | (2.394; 6.489) | 0.0001 |
| NOSE Score ≥50 versus < 50 | 3.904 | (1.686; 6.122) | 0.0011 |
| Adjusted R2 | 0.4865 |
- NOSE score, Nasal Obstruction Symptom Evaluation score.
Discussion
The main findings of this study are: (i) patients treated with an oronasal mask had more mean mouth opening during the night than patients treated with nasal masks; (ii) patients using oronasal mask had a greater oxygen desaturation index than patients on nasal masks; (iii) active smoking, nasal obstruction, male gender, larger neck circumference and lower FEV1were linked with mouth opening in univariate analysis; and (iv) in a multivariate analysis, male gender and nasal obstruction remained independently associated with mouth opening.
Previous randomized cross-over control studies comparing oronasal versus nasal masks25-28 have included patients who were either CPAP naïve27, 28 or already on effective long-term treatment with nasal CPAP without a chinstrap,25 therefore they did not necessarily need an oronasal mask. In the present study was different since an oronasal mask was mainly provided in second intention to counteract mouth leaks with a nasal mask. Our results show that even after several months of CPAP, patients using ONM persist in keeping their mouths open at night. Moreover, the oxygen desaturation index was also greater in patients with oronasal masks suggesting a lower degree of control of sleep-related respiratory events. This is in accordance with previous published studies25-28 that showed a higher residual AHI under oronasal compared to nasal masks. The greater residual AHI could in part be related to the weight of the mask on the chin and the headgear straps of the oronasal mask that put pressure on the mandible, displacing it backwards and therefore inducing an increase in pharyngeal resistance.7, 29 Interestingly, while the oxygen desaturation index was greater with oronasal masks, the 95th percentile pressure delivered by the auto-PAP was not different between nasal and oronasal masks. This finding is in agreement with Teo et al.28 who also used auto-titrating PAP. In contrast, using polysomnography (PSG)-guided PAP titration, Ebben et al. have shown that oronasal masks required higher pressure levels than nasal masks.27 Thus, the ability of auto-titrating PAP to set appropriate pressures in patients who keep their mouths open while using an oronasal mask could be questioned. It might be hypothesized that the pressure has not been adequately titrated by using auto-titrating CPAP and that persistent mouth opening is the consequence of an elevated upper airway resistance and obstructive events. However, the design of the present study did not allow to delineate the respective importance of mechanisms contributing to mouth opening and oxygen desaturation index between patients treated with nasal mask versus oronasal masks. Moreover, it is possible that the oronasal mask by itself promotes mouth opening by pressing on the jaw. In further studies, it would be interesting to explore if mouth opening persists in patients with a nasal mask and an oronasal mask, respectively, after PSG titration.
Beyond these technical considerations, patients treated with oronasal masks were more often active smokers, tended to have a lower respiratory function (FEV1) and greater nasal obstruction. Nasal obstruction that can be aggravated by active smoking is a well-known key factor in the persistence of mouth breathing and mouth opening under CPAP.30 Treating nasal obstruction reduced mouth breathing during sleep.31-33
Anthropometric variables such as male gender, neck circumference and respiratory function (FEV1) were also linked with mouth opening in univariate analysis. Fernandez et al.34 have assessed patients' preference when prescribing the mask for non-invasive home ventilation; they observed that patients who preferred an oronasal mask were more often male, and non-invasive ventilation settings with the oronasal mask required around 2 cm H2O higher pressure support than settings with nasal masks.34 This study was mainly performed with patients with obesity hypoventilation syndrome who demonstrate an increased work of breathing. This suggests that effort breathing may favour mouth opening and mouth breathing. In our study, male gender was strongly correlated with neck circumference (V′ Cramer > 0.5), thus this latter variable could not be proposed to the multivariate analysis. However, neck circumference also reflects central fat distribution. Centrally distributed fat has detrimental effects on thoraco-pulmonary mechanics35 and upper airway collapsibility,36 particularly in recumbent positions, increasing the effort breathing,35 and may favor mouth opening during sleep.
This study has some limitations. First, the small number of patients treated with an oronasal mask. The objective was to recruit at least 36 patients from consecutive patients attending our sleep clinic. The ratio of patients treated with oronasal mask versus nasal mask was equivalent to that observed in a large cohort study.5 Multiple comparisons should have led to decrease in study power and inflation of the type I error. In order to counteract this problem, we have reported P-values (Holm–Bonferroni correction); as shown with these corrected P-values, comparisons between patients with nasal mask versus oronasal mask have to be taken with caution. These results refer to a first exploratory study that needs to be confirmed by further trials. However, regarding our main objective, even with Bonferroni correction, patients with oronasal mask exhibited a significantly greater mouth opening during sleep than patients with nasal mask.
The second main limitation is that we did not use polysomnography to document sleep duration and residual respiratory events. However, the oxygen desaturation index remains a robust marker of sleep-related respiratory disturbance. Finally, non-intentional leaks tended to be more important in patients with oronasal masks. It was difficult in such a sample to compare several oronasal masks from several brands. Moreover, we cannot formally exclude that the wire of the chin sensor has not interfered with the oronasal mask seal and thus minimally contributed to the leaks; however this wire is lightweight (<1 mm of diameter), and we did not identify leaks related to this wire during the sensor placement.
In conclusion, the present study shows that apnoeic patients using oronasal masks with CPAP keep their mouths open during the night even after several months of treatment. Nasal obstruction is determinant; anatomical and functional abnormalities that increase nasal resistance should be evaluated and if possible treated prior to the initiation of oronasal mask use. The NOSE questionnaire may be a simple tool in this decision process. Others factors such as antropometric features which contribute to mouth opening need to be better understood.
Acknowledgements
We thank Professor Frédéric Sériès (CRIUCPQ, Laval University, Quebec, Canada) for the fruitful discussion and Dr Alison Foote (Grenoble Clinical Research Centre) for the English editing. The study was funded by the ‘AGIR à dom. Association’ and ‘Fonds AGIR pour les Maladies Chroniques’.