Comparable improvements achieved in chronic obstructive pulmonary disease through pulmonary rehabilitation with and without a structured educational intervention: A randomized controlled trial
Abstract
Background and objective
Pulmonary rehabilitation is beneficial for people with chronic obstructive pulmonary disease (COPD) and typically includes exercise and disease-specific education components. However, the benefits directly attributable to the education component remain unclear. This trial sought to determine whether the addition of education to exercise training resulted in greater improvements in health outcomes than pulmonary rehabilitation where education has been omitted.
Methods
A randomized trial with allocation concealment, assessor blinded to group allocation and intention-to-treat analysis was conducted. Two hundred and sixty-seven people with COPD (mean age 72(9) years, forced expiratory volume in 1 s, 59(23)% predicted) were allocated to receive either 8 weeks of twice weekly group exercise training plus education or exercise training alone. Education was disease specific with a self-management focus. Primary outcome measures included 6-min walk distance and Chronic Respiratory Questionnaire. Secondary outcomes included dyspnoea, health behaviours, generic health-related quality of life, self-efficacy and healthcare usage with measurements taken immediately following completion and at 6 and 12 months.
Results
There were no significant differences that indicated greater improvement in any health outcome with the addition of education. The two intervention groups had similar significant improvements immediately following intervention, and these were maintained comparably in the subsequent 12 months.
Conclusions
The results of this investigation suggest that disease-specific group education is not an essential component of pulmonary rehabilitation. Pulmonary rehabilitation based on exercise training is an effective option in the management of patients with COPD if multidisciplinary education cannot be offered.
Abbreviations
-
- COPD
-
- chronic obstructive pulmonary disease
-
- ET
-
- exercise training intervention
-
- ET + ED
-
- exercise training and education intervention group
-
- heiQ
-
- Health Education Impact Questionnaire
-
- HRQoL
-
- Health-related quality of life.
Introduction
Pulmonary rehabilitation improves health outcomes in chronic obstructive pulmonary disease (COPD).1, 2 Practice guidelines state comprehensive pulmonary rehabilitation involves patient assessment, exercise training, education, nutritional intervention and psychosocial support.1-5 However, clinical practice varies,6-8 and studies evaluating pulmonary rehabilitation have not consistently included all components.9
Randomized controlled trials have repeatedly shown significant improvements in exercise capacity, symptoms and health-related quality of life (HRQoL) with exercise training alone compared with usual care.9-11 Studies combining exercise training with an education component have demonstrated similar significant improvements.9 Education in the context of pulmonary rehabilitation has not been evaluated or clearly defined. Compared with usual care, self-management education has demonstrated decreased healthcare usage and improved HRQoL.12, 13 The typical provision of simultaneous exercise and education in trials examining pulmonary rehabilitation has not allowed discrimination of the benefits attributable to the education component.
This study describes the evaluation of benefit of disease-specific group education incorporating principles of self-management within a pulmonary rehabilitation programme for patients with COPD. The hypothesis was that pulmonary rehabilitation including exercise training and education would result in greater improvements in health outcomes than pulmonary rehabilitation where educational activities have been omitted.
Methods
Participants and study design
A randomized controlled trial was conducted at a large metropolitan tertiary hospital in Australia (Australian Clinical Trials Registration Number: ACTRNO 12605000703606). People with COPD referred for outpatient pulmonary rehabilitation between May 2004 and May 2005 (phase 1) and between November 2006 and June 2009 (phase 2) were invited to participate. Phase 2 included the addition of two further outcome measures: the Health Education Impact Questionnaire version 1.2 (heiQ)14 and outpatient healthcare usage for which specific ethical, legal and licensing approval were required.
Eligible participants had a primary diagnosis of COPD,2 reported dyspnoea with daily activities and were on stable medical therapy. People were excluded if they were not fluent in English, had a documented cognitive deficit limiting their ability to learn, had comorbidities limiting their ability to exercise, or if they had participated in a pulmonary rehabilitation programme in the preceding 2 years. All participants gave written informed consent, and the study was approved by the ethical review board of the administering institutions (La Trobe University FHEC05/23 and FHEC05/163, Austin Health H2004/01859 and H2006/02388).
Participants were assigned using computer-generated random numbers to one of two pulmonary rehabilitation intervention groups, with education being the independent variable. Allocation was performed independently using sequentially numbered sealed opaque envelopes.
All participants underwent baseline assessment including screening for nutritional and psychological abnormalities with subsequent individual intervention as indicated. Demographic data are presented in Table 1. Spirometry was measured with the EasyOne hand-held spirometer (Niche Medical Pty Ltd, Melbourne, Australia) following a standard protocol.15
| ET + ED n = 141 | ET n = 126 | |
|---|---|---|
| Age, years | 72.4 (10.0) | 72.0 (8.4) |
| Gender, male/female, n (%) | 89 (63)/52 (37) | 72 (57)/54 (43) |
| Current smokers, n (%) | 11 (8) | 14 (11) |
| Home oxygen, n (%) | 18 (13) | 16 (13) |
| Pulmonary function | ||
| FEV1, L | 1.3 (0.6) | 1.4 (0.6) |
| FEV1, % predicted | 56 (23) | 59 (22) |
| FVC, L | 2.6 (0.9) | 2.7 (0.9) |
| FEV1/FVC % | 52 (16) | 52 (16) |
| Respiratory-related hospital admissions | ||
| No hospital admissions, n (%) | 79 (56) | 68 (54) |
| One or more hospital admissions, n (%) | 62 (44) | 58 (46) |
| Body Composition | ||
| Weight, kg | 75.8 (17.2) | 74.7 (19.8) |
| Height, m | 1.65 (8.6) | 1.65 (8.9) |
| BMI, kg/m2 | 27.7 (5.8) | 27.4 (6.5) |
| Exercise Capacity | ||
| 6MWD | 370 (103) | 387 (103) |
| Quality of Life | ||
| CRQ Dyspnoea | 14.8 (5.6) | 13.7 (5.3) |
| Fatigue | 15.2 (5.4) | 14.7 (5.4) |
| Emotion | 32.8 (9.2) | 33.2 (8.4) |
| Mastery | 18.5 (5.7) | 19.3 (5.1) |
- Data are mean (standard deviation).
- 6MWD, 6-min walk distance; BMI, body mass index; CRQ, Chronic Respiratory Questionnaire; ET, exercise training intervention; ET + ED, exercise training and education intervention group; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity.
Intervention
All participants attended a twice-weekly supervised exercise training intervention (ET) for eight weeks. Exercise prescription was consistent with recommended exercise training principles for patients with COPD.3, 4 Thirty minutes of lower limb endurance exercise was prescribed at each session using treadmill walking (commenced at 70% of baseline 6-min walk test speed) and stationary cycling. Resistance training comprised moderate intensity upper and lower limb functional strength training. Exercise was monitored and progressed by an experienced physiotherapist according to a previously described standardized protocol.16 Supplemental oxygen was provided during training as necessary to achieve oxygen saturation ≥88%.17 All participants were provided with an illustrated exercise guide and diary, and encouraged to complete the same exercise programme at home to a total of five exercise sessions per week. Exercise sessions for both groups were conducted on the same day in separate locations, supervised by the same experienced physiotherapist and exercise physiologist.
Participants assigned to the exercise training and education intervention group (ET + ED) also completed an education programme consisting of sixteen 45-min sessions (topics detailed in Table 2). The content and format were consistent with international pulmonary rehabilitation position statements and recommendations.2-5 The face-to-face group education sessions minimized didactic delivery of material. Group discussions were facilitated by members of a multidisciplinary team (Table 2) who had a total of 34 years (range 1–15 years) of experience conducting pulmonary rehabilitation. Individual behaviour-specific action plans were formulated and reviewed at each session. The action plan involved a participant making a short-term plan to change specific aspects of their lifestyle over a 1- to 2-week period. An illustrated education booklet, compiled by members of the multidisciplinary team with patient feedback, was issued to participants. Content was reviewed by a senior respiratory physician, and language and structure were edited by a reading language specialist to achieve a reading level that a 12-year-old could comprehend. Carers or support people were welcome to accompany participants to all sessions. For both groups, completion of the trial protocol was considered to be attendance at ≥12 supervised sessions of exercise training with or without education.
| Topic | Healthcare professional |
|---|---|
| Lung disease and COPD management | Respiratory physician |
| Respiratory function tests | Respiratory scientist |
| Medications | Pharmacist |
| Home oxygen therapy | Respiratory physician |
| Self-management including exacerbations | Respiratory nurse |
| Managing breathlessness | Physiotherapist |
| Energy conservation | Occupational therapist |
| Exercise and physical activity | Exercise physiologist |
| Stress and anxiety | Occupational therapist |
| Nutrition and health eating | Dietician |
| Sexuality and intimacy | Respiratory nurse |
| Community resources | Social worker |
| Swallowing and COPD | Speech therapist |
| Swallow screening | Speech therapist |
| Continence and COPD | Physiotherapist |
| Airway clearance | Physiotherapist |
- COPD, chronic obstructive pulmonary disease.
Outcome measures
Primary outcomes were disease-specific HRQoL evaluated with the self-reported Chronic Respiratory Disease Questionnaire,18 and functional exercise capacity was measured using the 6-min walk distance using a practice test, standardized environment, instructions and encouragement.19 These were chosen because they are the primary outcomes of pulmonary rehabilitation, and the aim of this trial was to determine the benefit of education within pulmonary rehabilitation.
Secondary outcomes included dyspnoea, assessed with the Medical Research Council dyspnoea scale,20 functional activity with the grocery shelving task,21 general HRQoL using the Assessment of Quality of Life tool22 and self-efficacy with the General Self-Efficacy Scale-12.23
For all participants, healthcare usage was measured as respiratory-related hospital admissions, tracked via electronic database at the participating tertiary hospital. An admission was considered respiratory-related when the admission diagnosis was documented as COPD, exacerbation of COPD, chest infection or pneumonia. Medical consultation and prescription medication supply data from Australian government bodies including Medicare Australia, Department of Veterans Affairs, the Pharmaceutical Benefits Scheme and the Repatriation Pharmaceutical Benefits Scheme were accessed for phase 2 participants.
The impact of the education was measured in phase 2 participants using the 42-item heiQ.14 This tool aims to establish how education has impacted on a participant's perceived positive engagement in life, healthy behaviours, skill acquisition, constructive attitudes, self-monitoring behaviours, confidence for health service navigation, social integration and support, and emotional well-being.
Primary outcome measures were recorded at baseline, immediately following the intervention, and at 6 and 12 months. Secondary outcomes were recorded at baseline, immediately post and 12 months post-intervention. Healthcare usage was recorded for the 12 months prior to and following intervention. All measurements were completed by an independent data collector blinded to intervention allocation.
Analysis
Based on pilot data, a sample of 100 participants per group was required to detect minimally important differences between groups of 0.5 per item for the Chronic Respiratory Disease Questionnaire24 and 54 m in 6-min walk distance25 (effect size of 0.2) immediately following intervention, with a 5% significance level and power of 80%. Intention-to-treat analysis was undertaken whereby all participants were scheduled to attend follow-up assessment, regardless of completion and all available data have been included in the analysis.
Statistical analyses for outcomes with repeated measures over 12 months were performed using a generalized estimated equation with Gaussian distribution (generalized estimated equation).26 Generalized estimated equation were chosen to allow for analysis of incomplete longitudinal data maximizing analysis sample size by including all data points available.26 Where data were not normally distributed, generalized estimated equations were used with a Gamma distribution. Data are reported as a group allocation coefficient outlining the mean difference between the groups considering all time points. Time coefficients are also reported, outlining the mean difference between baseline and each post-intervention assessment time for all participants as a cohort. Nominal data were compared using a Pearson's chi-square. Non-parametric healthcare usage data were compared using a Mann–Whitney U for between-group differences and Wilcoxon Signed Rank for within-group differences. Significance was set at P < 0.05. Analyses were completed using stata (Release12, StataCorp LP, College Station, TX, USA) with guidance from a health statistician.
Results
One hundred and forty-one participants were randomized to the ET + ED group and 126 to the ET group, with all participants receiving allocated intervention (Fig. 1). No adverse events related to intervention were recorded. Overall participants attended a mean of 11 of possible 16 sessions of exercise training (ET + ED group mean 11.5 (4.6), ET group mean 10.6 (5.1), P = 0.616). The mean number of education sessions attended by the ET + ED participants was 10.4 (4.7). The number of participants completing 12 or more exercise training sessions was not significantly different between the groups (X2(1) = 3.288, P = 0.07) (Fig. 1).
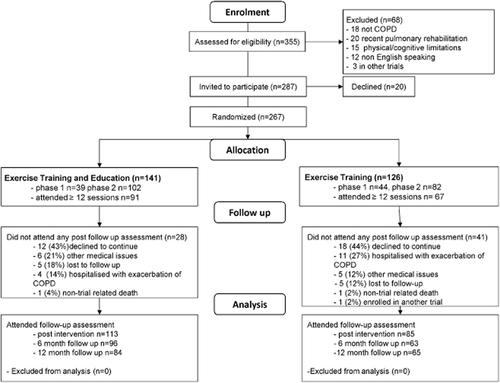
Summary of recruitment and allocation process.
Attendance at follow-up assessments was significantly greater for the ET + ED group (80%) than the ET group (67%) immediately following intervention (X2(1) = 5.584, P = 0.018) and also at 6-month follow-up (68% and 49%, X2(1) = 9.035, P = 0.003), it but was not significantly different at 12 months (60% and 52%, X2(1) = 1.721, P = 0.19). The number of participants who did not attend any follow-up was greater in the ET group (33%) than the ET + ED group (20%) (X2(1) = 5.584, P = 0.018). Reasons for non-attendance are detailed in Figure 1. No participants withdrew consent for access to their healthcare usage data resulting in no loss to follow-up for these outcomes for either group.
Primary outcomes
There were no significant differences between the groups for any Chronic Respiratory Disease Questionnaire domain scores or 6-min walk distance (Table 3). Participants in both groups demonstrated statistically significant improvements in exercise capacity and all domains of HRQoL, which were maintained over the 12 months following intervention for all measures. These improvements exceeded the minimally important differences for the Chronic Respiratory Disease Questionnaire domains of dyspnoea, fatigue and mastery,24 and the recently updated minimally important differences of 25–35 m for 6-min walk distance19, 27 (Figs 2, 3).
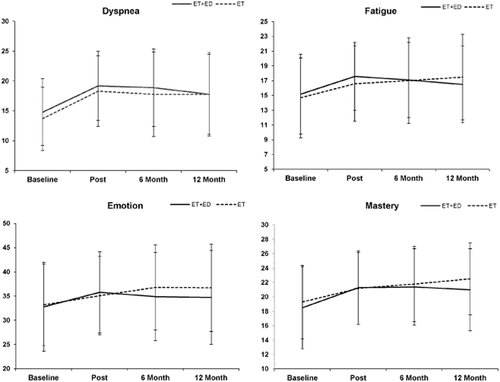
Comparison between groups for the four domains of Chronic Respiratory Questionnaire.
Mean Chronic Respiratory Questionnaire domain score and error bars ± 1 SD; ET, exercise training intervention; ET + ED, exercise training and education intervention group.  , ET + ED;
, ET + ED;  , ET.
, ET.
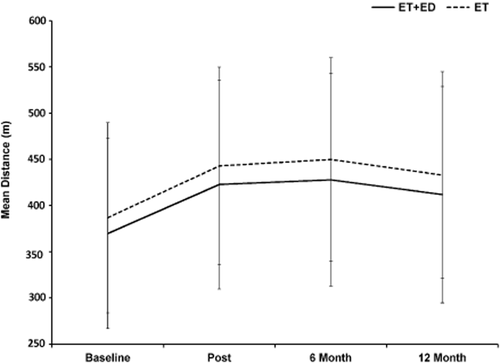
Comparison between groups for 6-min walk distance. Mean and error bars ± 1 SD; ET, exercise training intervention; ET + ED, exercise training and education intervention group.  , ET + ED;
, ET + ED;  , ET.
, ET.
| Outcome | Baseline | Post-intervention | 6 months | 12 months | Group allocation coefficient (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|---|
| ET + ED | ET | ET + ED | ET | ET + ED | ET | ET + ED | ET | ||
| CRQ Dyspnoea | 14.8 (5.6) | 13.7 (5.3) | 19.2 (5.8) | 18.3 (5.9) | 18.9 (6.5) | 17.8 (7.1) | 17.8 (6.7) | 17.8 (7.0) |
−0.7 (−2.0 to 0.7) P = 0.338 |
| Time coefficient (95% CI) | 4.6 (3.6–5.0)* | 4.3 (3.6–5.0)* | 3.5 (2.8–4.2)* | ||||||
| CRQ Fatigue | 15.2 (5.4) | 14.7 (5.4) | 17.6 (4.6) | 16.6 (5.1) | 17.1 (5.1) | 17.0 (5.8) | 16.5 (5.2) | 17.5 (5.8) |
−0.1 (−1.3 to 1.0) P = 0.800 |
| Time coefficient (95% CI) | 2.2 (1.6–2.8)* | 2.0 (1.4–2.7)* | 2.0 (1.4–2.7)* | ||||||
| CRQ Emotion | 32.8 (9.2) | 33.2 (8.4) | 35.8 (8.4) | 35.1 (8.1) | 34.9 (9.1) | 36.8 (8.8) | 34.7 (9.7) | 36.7 (9.0) |
1.0 (−0.9 to 2.9) P = 0.301 |
| Time coefficient (95% CI) | 2.6 (1.7–3.6)* | 2.8 (1.8–3.9)* | 2.6 (1.5–3.6)* | ||||||
| CRQ Mastery | 18.5 (5.7) | 19.3 (5.1) | 21.3 (5.1) | 21.2 (5.0) | 21.4 (5.3) | 21.9 (5.2) | 21.0 (5.7) | 22.5 (5.0) |
0.8 (−0.4 to 1.9) P = 0.199 |
| Time coefficient (95% CI) | 2.2 (1.6–2.8)* | 2.5 (1.8–3.1)* | 2.4 (1.7–3.0)* | ||||||
| 6MWD (m) | 370 (103) | 387 (103) | 423 (113) | 443 (107) | 428 (115) | 450 (110) | 412 (117) | 433 (112) |
16.5 (−9.0 to 41.9) P = 0.205 |
| Time coefficient (95% CI) | 42.4 (34.4–50.3)* | 36.6 (28.0–45.2)* | 23.7 (15.0–32.5)* | ||||||
- * P < 0.05 compared with baseline, bold indicates a significant result.
- Data are mean (standard deviation).
- 6MWD, 6-min walk distance; CI, confidence interval; CRQ, Chronic Respiratory Questionnaire (Self-administered); ET, exercise training intervention; ET + ED, exercise training and education intervention group.
Secondary outcomes
There were no significant between-group differences for the secondary outcomes except for the Assessment of Quality of Life total score (Table 4). The ET group continued to improve in Assessment of Quality of Life total score over the 12 months following intervention, whereas the ET + ED group regressed towards the baseline score, giving a significant group allocation coefficient in favour of the ET group (P = 0.046).
| Outcome | Baseline | Post-intervention | 12 months | Group allocation coefficient (95% CI) | |||
|---|---|---|---|---|---|---|---|
| ET + ED | ET | ET + ED | ET | ET + ED | ET | ||
| GST (seconds) | 40 (11) | 39 (14) | 35 (10) | 34 (8) | 35 (9) | 36 (11) |
0.2 (−1.9 to 2.3) P = 0.854 |
| Time coefficient (95% CI) | –4.4 (−5.9 to −3.0)a | –3.4 (−5.0 to −1.8)a | |||||
| AQoL Total | 14.9 (6.0) | 13.6 (5.2) | 13.8 (5.7) | 13.0 (5.7) | 14.1 (5.6) | 12.8 (4.9) |
–1.3 (–2.6 to −0.02)a P = 0.046 |
| Time coefficient (95% CI) | –0.7 (−1.2 to −0.2)a | –0.4 (−1.0 to 0.2) | |||||
| AQoL Utility | 0.53 (0.25) | 0.58 (0.22) | 0.57 (0.22) | 0.60 (0.22) | 0.55 (0.23) | 0.61 (0.22) |
0.05 (−0.0002 to 0.1) P = 0.051 |
| Time coefficient (95% CI) | 0.02 (0.001–0.05)a | 0.002 (−0.02 to 0.03) | |||||
| GSES-12 | 46.1 (8.3) | 45.4 (8.8) | 47.0 (7.0) | 45.8 (7.9) | 46.7 (7.4) | 46.9 (8.2) |
–0.5 (−2.2 to 1.2) P = 0.554 |
| Time coefficient (95% CI) | 0.7 (−0.3 to 1.6) | 0.7 (−0.4 to 1.7) | |||||
| HEI-Q Positive engagement in lifeb | 4.6 (0.9) | 4.6 (0.9) | 4.6 (0.9) | 4.6 (0.9) | 4.6 (1.0) | 4.8 (0.9) |
0.03 (−0.2 to 0.3) P = 0.820 |
| Time coefficient (95% CI) | 0.1 (−0.1 to 0.2) | 0.1 (−0.1 to 0.2) | |||||
| HEI-Q Health behaviourb | 4.0 (1.4) | 4.1 (1.3) | 4.8 (1.0) | 5.0 (0.9) | 4.5 (0.9) | 4.5 (1.2) |
0.2 (−0.1 to 0.5) P = 0.201 |
| Time coefficient (95% CI) | 0.8 (0.6–1.0)a | 0.4 (0.2–0.6)a | |||||
| HEI-Q Skill acquisitionb | 4.5 (0.8) | 4.6 (0.7) | 4.6 (0.8) | 4.6 (0.6) | 4.7 (0.6) | 4.9 (0.6) |
0.1 (−0.1 to 0.3) P = 0.295 |
| Time coefficient (95% CI) | 0.1 (−0.04 to 0.2) | 0.3 (0.1–0.4)a | |||||
| HEI-Q Constructive attitudesb | 4.8 (0.8) | 4.9 (0.7) | 4.7 (0.8) | 4.9 (0.6) | 4.8 (0.7) | 4.9 (0.8) |
0.2 (−0.004 to 0.4) P = 0.055 |
| Time coefficient (95% CI) | –0.003 (−0.1 to 0.1) | 0.02 (−0.1 to 0.2) | |||||
| HEI-Q Self monitoringb | 4.8 (0.6) | 4.9 (0.6) | 4.9 (0.6) | 4.9 (0.5) | 4.9 (0.5) | 5.0 (0.7) |
0.1 (−0.05 to 0.2) P = 0.246 |
| Time coefficient (95% CI) | 0.1 (−0.01 to 0.2) | 0.1 (0.01–0.2)a | |||||
| HEI-Q Health service navigationb | 5.1 (0.6) | 5.2 (0.6) | 5.2 (0.6) | 5.3 (0.5) | 5.3 (0.5) | 5.4 (0.6) |
0.1 (−0.1 to 0.3) P = 0.215 |
| Time coefficient (95% CI) | 0.1 (−0.02 to 0.2) | 0.2 (0.1–0.3)a | |||||
| HEI-Q Social integrationb | 4.9 (0.9) | 5.0 (0.7) | 4.8 (1.0) | 4.9 (0.9) | 4.8 (1.0) | 5.1 (0.8) |
0.1 (−0.1 to 0.4) P = 0.313 |
| Time coefficient (95% CI) | –0.04 (−0.2 to 0.1) | 0.02 (−0.1 to 0.2) | |||||
| HEI-Q Emotional well-beingb | 3.6 (1.2) | 3.7 (1.2) | 3.7 (1.2) | 3.9 (1.1) | 3.6 (1.1) | 4.1 (1.2) |
0.2 (−0.1 to 0.5) P = 0.192 |
| Time coefficient (95% CI) | 0.1 (−0.03 to 0.3) | 0.1 (−0.1 to 0.3) | |||||
- a P < 0.05 compared with baseline, bold indicates a significant result.
- Data are mean (standard deviation).
- b Sample size ET + ED, n = 102; ET, n = 82.
- AQoL, Assessment of Quality of Life questionnaire; CI, confidence interval; ET, exercise training intervention; ET + ED, exercise training and education intervention group; GSES-12, General Self-Efficacy Scale-12; GST, Grocery Shelving Task; HEI-Q, Health Education Impact Questionnaire.
Participants demonstrated significant improvements immediately following rehabilitation compared with baseline in functional activity (grocery shelving task, P < 0.001), Assessment of Quality of Life total (P = 0.008) and utility (P = 0.039) (Table 4). Thirty-five percent of participants in the ET + ED group and 28% of participants in the ET group had an improvement of one or greater Medical Research Council dyspnoea grade (X2(1) = 0.881,P = 0.348). Both groups (ET + ED n = 102, ET n = 82) had significant improvements immediately following rehabilitation in health-directed behaviour as measured by the heiQ, which were maintained for 12 months. There were also significantly higher scores for both groups in self-monitoring, skill acquisition and health service navigation at 12 months.
There was no difference between groups in the number of participants who had a respiratory-related hospital admission (25% of ET + ED vs 27% of ET, X2(7) = 7.125, P = 0.416 Table 5) which decreased significantly for both groups (P < 0.001). The median length of stay was 6 days for both groups (ET + ED range 1–23, ET range 1–47, P = 0.544).
| Healthcare usage | 12 months pre-intervention | 12 months post-intervention | Between groups Post | Within sample pre/post | ||
|---|---|---|---|---|---|---|
| ET + ED n = 101 | ET n = 80 | ET + ED n = 101 | ET n = 80 | |||
| Hospital admissions* | ||||||
| Total no. | 90 | 87 | 55 | 54 | ||
| Median (range) | 0 (0–3) | 0 (0–5) | 0 (0–7) | 0 (0–4) | P = 0.342 | P < 0.001 |
| General practitioner | ||||||
| n (total) | 1507 | 1208 | 1477 | 1147 | ||
| Median (range) | 13 (0–64) | 15 (0–43) | 14 (0–57) | 12 (0–73) | P = 0.088 | P = 0.191 |
| Respiratory physician | ||||||
| n (total) | 262 | 207 | 203 | 181 | ||
| Median (range) | 2 (0–11) | 2 (0–11) | 2 (0–13) | 2 (0–11) | P = 0.570 | P = 0.009 |
| Inhaled reliever medications | 2 (0–42) | 3 (0–43) | 3 (0–60) | 3 (0–29) | P = 0.693 | P = 0.455 |
| Tiotropium bromide | 4 (0–24) | 5 (0–14) | 9 (0–14) | 10 (0–14) | P = 0.066 | P < 0.001 |
| Inhaled corticosteroid | 0 (0–3) | 0 (0–8) | 0 (0–6) | 0 (0–13) | P = 0.381 | P = 0.114 |
| Inhaled combination therapy (steroid and LABA) | 5 (0–25) | 4 (0–21) | 6 (0–20) | 7 (0–16) | P = 0.139 | P < 0.001 |
| Oral prednisolone | 0 (0–19) | 1 (0–11) | 0 (0–17) | 0 (0–17) | P = 0.750 | P = 0.693 |
| Oral antibiotic | 4 (0–26) | 4 (0–34) | 3 (0–32) | 3 (0–30) | P = 0.541 | P = 0.811 |
- Bold indicates a significant result. Data are median (range) unless stated otherwise. Medications are number of prescriptions dispensed per participant over 12 months.
- * Sample size ET + ED = 141, ET = 126.
- ET, exercise training intervention; ET + ED, exercise training and education intervention group; LABA, long-acting β2 agonist.
Data were obtained for physician consultations and supply of prescription pharmaceuticals for 181 phase 2 participants. There were no significant differences between the groups in the median number of physician visits or supply of prescription medications in the 12 months following intervention (Table 5). There was a significant reduction in respiratory physician consultations, whereas there were significant increases in preventative or symptom controller medication supply (inhaled combination therapy P < 0.001 and tiotropium bromide P < 0.001) in the 12 months following intervention for both groups.
Discussion
This is the first large randomized controlled trial to investigate additional benefits directly attributable to disease-specific education incorporating self-management within a pulmonary rehabilitation programme for people with COPD. Both models of pulmonary rehabilitation with and without an education component were effective, with significant improvements in health outcomes immediately following the intervention that was maintained up to 12 months for the majority of parameters. There were no clinically important differences between the groups in any outcomes, reinforcing the belief that exercise is the key component for improving functional capacity and HRQoL in a pulmonary rehabilitation programme.
These results are consistent with the only other study which has attempted to isolate the education component of pulmonary rehabilitation.28 In an observational study, Crisafulli et al. found that participants with COPD who completed both education and exercise components of pulmonary rehabilitation had significantly higher levels of knowledge than participants who chose to complete only exercise training, but these reported increases in knowledge failed to carry over into greater improvements in HRQoL or exercise capacity.28 As participants in that study chose whether or not to complete the education component, results should be interpreted with caution; nonetheless, these are consistent with results from the current randomized controlled trial which demonstrated comparable improvements in health outcomes following pulmonary rehabilitation with or without formal education.
Attainment of knowledge was not specifically measured in the current study; however, the heiQ was used for phase 2 participants in an attempt to detect differences between the groups related to the education intervention. Although not a well-established measure in COPD, the heiQ has been validated to measure effectiveness of self-management education in chronic disease populations.14 The heiQ did not demonstrate any significant improvements in the education group that were not evident in the exercise training group, suggesting pulmonary rehabilitation where education has been omitted leads to comparable changes in health behaviours.
The lack of benefit observed with the addition of educational activities to exercise training in pulmonary rehabilitation in this study requires further exploration. Conclusions have been made relating to the education model described. This model was disease specific and included educational topics derived from international pulmonary rehabilitation position statements as well as from national resources guiding clinical practice.3, 4 The use of written behavioural action plans found to be beneficial in self-management education was included.29 Other models of facilitating behaviour change may yield different results. The present study did not directly compare two or more models of education nor examine behavioural therapy interventions within pulmonary rehabilitation. Interestingly though, the magnitude of benefit in HRQoL and healthcare usage outcomes was comparable with, or greater than, that identified in a systematic review examining education versus usual care for people with COPD conducted by our group.12 Further research to identify the best method of facilitating behaviour change in pulmonary rehabilitation would be justified.
Improvements in health behaviour and pattern of pharmaceutical usage were noted in both groups despite the exercise group only receiving specific information regarding exercise training. Informal education and advice that occur within a supervised exercise training programme were not controlled for but was expected to be similar between the groups as the same staff was involved. It was not possible to have intervention staff blinded to group allocation. Informal education and advice from health professionals external to pulmonary rehabilitation were also not controlled. Patients are likely to be referred to pulmonary rehabilitation following a specialist consultation or an exacerbation, at which time all aspects of the management of their COPD are likely to be addressed concurrently.
A limitation of this study is the completion rate with only 60% of those randomized completing the intervention protocol and 26% of participants not attending any follow-up assessment. However, the mean attendance rate by participants was 70% of sessions, one session short of the relatively high (75%) intervention protocol completion criterion. The broad inclusion criteria considered all people with a diagnosis of COPD with no restrictions for age, disease severity or smoking status, resulting in 75% of those referred to pulmonary rehabilitation with COPD being recruited. The sample is a representative of clinical practice where adherence rates are known to be poor.30 A per-protocol analysis was conducted with participants who completed more than 12 sessions, but still, no between-group differences were found in any outcomes. The significant difference between the groups in attendance at follow-up assessment and dropout may potentially lead to bias in results for outcome measures, including the primary outcome measures, collected at these assessments. Reasons for non-attendance were similar between groups (Fig. 1) other than for hospitalization for COPD which was higher in the group without education. Healthcare usage outcomes including hospitalization were not influenced by non-attendance as data were obtained for all participants from an independent database and no participant in either group withdrew consent for these data to be collected. We can therefore be more confident in the finding that the inclusion of education within a pulmonary rehabilitation programme does not lead to additional benefits in healthcare usage over pulmonary rehabilitation without education.
The extended period over which recruitment occurred and the two trial phases may also be considered a limitation of the trial. However, no changes were made to the intervention protocols between the two phases which remain consistent with the current clinical practice guidelines of the American Thoracic Society and European Respiratory Society and reflect local resources guiding practice3, 4 Content of the education material was updated as necessary with medical knowledge advances such as new medications. Additional outcome measures were introduced for phase 2: the heiQ and detailed healthcare usage from government databases. As such, these outcomes were only available for phase 2 participants (68% of the total sample).
Clinical implications of our trial are significant when considering access of people with COPD to pulmonary rehabilitation programmes. Health professionals from 10 different disciplines delivered the education programme. This compares with two health professionals for the exercise training component. Internationally, a health workforce shortage is occurring, with notable lack of access to specialist medical, nursing and allied health professionals, especially in regional and rural areas.31, 32 Some locations may not have the resources to offer a comprehensive multidisciplinary pulmonary rehabilitation programme. To maximize access for people with COPD, other models of pulmonary rehabilitation warrant consideration.
In conclusion, this study demonstrated that the addition of education to exercise training within a pulmonary rehabilitation programme did not result in greater improvements in health outcomes. Pulmonary rehabilitation where education has been omitted may be an effective option in the management of people with COPD where multidisciplinary staffing resources are limited and educational activities cannot be offered.
Acknowledgements
The authors would like to acknowledge Dr Siew Chan, health statistician, La Trobe University, for his guidance in selection of statistical analyses and interpretation of results.