Infant With Beckwith–Wiedemann Requiring Transplant for Hepatic Mesenchymal Hamartoma
Funding: The authors received no specific funding for this work.
ABSTRACT
Background
Liver transplantation for unresectable, benign hepatic lesions is rare. Hepatic mesenchymal hamartomas (HMH) are benign, cystic tumors that arise mostly in pediatric populations and can cause compressive symptoms. HMH is rarely associated with placental mesenchymal dysplasia (PMD) and Beckwith–Wiedemann syndrome (BWS). Treatment is complete excision due to the risk of rapid growth, recurrence, and malignant transformation. Very rarely is HMH so diffuse that transplantation is required.
Methods
We present the first case of a patient with BWS, HMH, and a history of PMD who underwent a transplant. This is also incidentally the third case of a pediatric patient with a myxoid adrenocortical adenoma (MACA).
Results
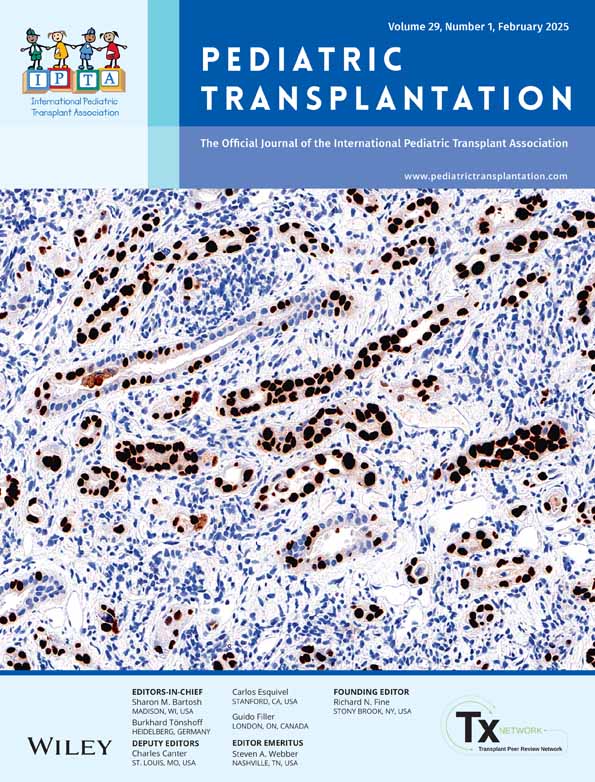
Our patient with HMH, MACA, chronic respiratory distress secondary to tracheobronchomalacia and abdominal competition from hepatomegaly, and nasojejunal (NJ) tube dependence successfully underwent orthotopic whole liver transplantation at 7 months of age. She had one episode of acute cellular rejection, but otherwise recovered well. Despite negative molecular testing for BWS in peripheral blood, additional analysis on the explanted liver was consistent with a diagnosis of mosaic BWS. At a 14-month follow-up, she continues to do well with improvement in growth.
Conclusions
Transplantation is an effective treatment option for patients with unresectable HMH. Our case highlights this and introduces a possible underlying association between HMH, PMD, and BWS.
Disclosure
The authors have nothing to report.
Open Research
Data Availability Statement
The authors have nothing to report.