Pediatric donor heart acceptance practices in the United States: What is really being considered?
Abstract
Background
Recent studies demonstrate high offer decline and organ non-utilization rates are associated with increased pediatric heart transplant waitlist mortality. We sought to determine which donor, candidate, and offer specific variables most importantly influenced these decisions using only data available at the time of each offer.
Methods
Retrospective review of pediatric (<18 years) heart donor offers made to pediatric candidates in the United States between 2010 and 2020. In addition to standard donor, candidate, and offer data available in UNOS, we extracted objective and qualitative valvar and myocardial function data from all available donor echocardiogram reports.
Results
During the study period, 5625 pediatric donor hearts produced 30 156 offers to 4905 unique candidates, of which 88.7% of all offers were declined and 39.2% of organs were not utilized by pediatric waitlisted candidates. Of the 60.8% utilized hearts, 89.7% had a ‘cumulatively’ normal echocardiogram at the time of offer acceptance; 62.9% of hearts not utilized for a pediatric candidate also had a cumulatively normal final echocardiogram. Random forest and logistic regression modeling demonstrated good predictive performance (AUROC ≥0.83) of likelihood to accept when utilizing donor, candidate, and offer specific variables. SHAP variable importance scores demonstrated number of prior offer declines and candidate institution's prior year acceptance rates as the two most important variables influencing offer decisions.
Conclusions
Behavioral economics appear to play a significant role in pediatric heart transplant candidate institutions' acceptance practices, even when considering the arguably healthier pediatric donor population. Removal of prior institution's decisions from DonorNet may help increase donor utilization.
Abbreviations
-
- DDNC
-
- Declaration of Death by Neurologic Criteria
-
- LR
-
- Logistic Regression
-
- RF
-
- Random Forest
1 INTRODUCTION
Despite a 20% waitlist mortality,1 nearly half of all donor hearts offered to US infants and children waitlisted for heart transplantation are ultimately discarded.2, 3 To understand this incongruity, a recent international survey of pediatric heart transplant clinicians demonstrated marked variability in donor acceptance practices, a finding that was underscored by US centers reporting significantly more restrictive donor age, donor/candidate weight ratio, and left ventricular ejection fraction (LVEF) criteria.4 Such findings inspired an international writing group focused on optimizing pediatric donor heart utilization and reducing waitlist mortality without negatively impacting post-transplant outcomes.5 The resulting publications concluded that, aside possibly from cerebrovascular accident as a cause of death and donor ischemic time, in the setting of a normal donor LVEF, virtually all other donor heart characteristics become irrelevant for post-transplant outcomes.5, 6 These recommendations, however, were oftentimes derived from adult or small pediatric studies, always used final LVEF as the only indicator of myocardial assessment, and incorporated data from the entirety of a donor's ‘terminal hospitalization’ in variable assessment.
The intent of our study was to provide the most complete assessment of pediatric donor heart acceptance practices in the US by including the entirety of a donor heart's echocardiographic interpretation, vital sign, and medical management data available to centers, but only using the data available at the time a donor offer was made.
2 MATERIALS AND METHODS
2.1 Data source
This retrospective study utilized donor data from the Organ Procurement and Transplant Network (OPTN) which includes data on all donors, waitlisted candidates, and transplant recipients in the US, submitted by the members of OPTN. The Health Resources and Services Administration (HRSA), U.S. Department of Health and Human Services provides oversight of the activities of the OPTN contractor. The data reported here have been supplied by the United Network of Organ Sharing (UNOS) as the contractor for OPTN. The interpretation and reporting of these data are the authors' responsibility and in no way represent an official policy of or interpretation by the OPTN or the US Government. This study was approved by the University of Virginia's (UVA) Institutional Review Board (IRB). Both the OPTN and UVA consider research using decedent data as ‘non-human research’ and do not require full IRB approval.
2.2 Study population and data collected
Data were evaluated on all pediatric donors (<18 years of age at the time of declaration of death by neurologic criteria (DDNC)) whose hearts were offered to pediatric patients (<18 years of age at the time of offer) on the waitlist for heart transplantation between January 1, 2010 and December 31, 2019. Donors following declaration of cardiac death, offers made to a candidate who had already accepted another organ, and candidates requiring heart-lung or retransplantation were excluded. In addition to the de-identified data available within the provided DonorNet database files, all attachments (PDF format) associated with the donor's terminal hospitalization were also provided for evaluation. These attachments included, but were not limited to: cardiology consultation forms, echocardiographic (echo) interpretations both within the native echo interpretation software and subsequent electronic medical record formats, and all formal donor documentation produced by the Organ Procurement Organization (OPO) personnel responsible for donor management. PDF data extraction focused entirely on echo-related documentation, specifically: study date and time; qualitative assessments of right ventricular systolic function; objective and qualitative assessments of left ventricular systolic function; objective assessments of tricuspid valve insufficiency gradients; qualitative assessments of atrioventricular and semilunar valve insufficiency; and any structural abnormalities, as outlined below. Data were extracted by MM, SW, and FH and a team of 24 undergraduate University of Virginia students personally instructed on the technique by MM prior to any data extraction. After initial instruction, MM reassessed extraction accuracy by reviewing the first 50 donor files of each student and provided repeat training as necessary. MM continued to over-read studies until satisfactory performance was achieved by every student. Data were entered into a REDCap database produced and maintained by UVA. REDCap (research electronic data capture) is a secure, web-based application designed to support data capture for research studies, providing: (1) an intuitive interface for validated data entry; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; (4) procedures for importing data from external sources. The REDCap echo database was subsequently merged with the DonorNet database using individual DONOR IDs.
Data were collected on the donors, candidates, offers, listing centers, donor hospitals, and OPOs. Static donor data included gender, race, weight, height, date and time of DDNC, cause of death, duration of cardiopulmonary resuscitation (CPR), center for disease control (CDC) high-risk status, and blood type. Dynamic donor variables include the time since DDNC, vital signs, inotrope administration, and echocardiogram reports. Candidate variables included status, diagnosis, calculated panel reactive antibody (cPRA), weight, height, gender, race, blood type and need for mechanical ventilation, extracorporeal membrane oxygenation (ECMO), or ventricular assist device (VAD). The donor/candidate weight ratio and age differences were also included. Offer variables included distance between donor hospital and transplant center, offer time of day, and the number of prior donor refusals. We also calculated listing centers' prior year number of pediatric heart transplants, prior year acceptance rate by candidate status, and prior 18-month adverse outcome rate (defined as the censoring adjusted proportion of transplants occurring in the last 18 months that required re-transplant or resulted in patient death within 1 year). The Organ Procurement Organization's (OPO) prior year number of pediatric donors managed and donor hospital's prior year number of pediatric donors produced were also included. Since we did not have offers from 2009, 2010 data were utilized as a proxy for the prior year's values.
2.3 Echocardiographic data
We collected date and time of donor echocardiogram reports as well as qualitative and quantitative assessments of right and left ventricular function and both semilunar and atrioventricular valve function. An echocardiogram received a composite categorization of ‘Normal’ if: qualitative assessments of right and left ventricular wall motion were considered normal AND if present, ejection fraction measurements were ≥55% and/or shortening fraction was ≥28%; AND no evidence of left ventricular segmental wall motion abnormalities (LVSWMA); AND no more than mild insufficiency of either semilunar or atrioventricular valve; all other studies were considered ‘Abnormal’. Any structural abnormalities aside from atrial septal defects were noted when relevant (e.g., bicuspid aortic valves, ventricular septal defects) but were not considered in the composite endpoint. For a more detailed description of the echocardiographic data assessment, see Appendix S1.
2.4 Primary outcome
The primary outcome for each offer was whether a pediatric heart transplant candidate's institution decided to ‘accept’ or ‘decline’. A heart accepted for the first candidate on a donor list was determined to have produced 1 offer and if accepted by the 10th candidate, that donor heart generated 10 different offers. In both cases, the final offer was considered ‘accepted’ and the donor heart ‘utilized’ by a candidate in our study population. If a donor heart was never accepted by a candidate in our study population during the study period, that organ was considered ‘non-utilized’. It is possible that non-utilized organs were eventually accepted for a candidate outside of our study population (e.g., adult or Canadian candidate) or after December 31, 2019. It is also possible that an accepted organ was never procured or transplanted.
2.5 Statistical analysis and mathematical modeling
Descriptive statistics utilized median and interquartile ranges for continuous and proportions for categorical variables, respectively. Comparisons between groups utilized Wilcoxon rank sum or chi-square as appropriate. Considering the large number of variables assessed, statistical significance was assessed with a p-value <.01.
Multivariable logistic regression (LR) and random forest (rf) models were fit to determine patterns associated with the decision to ‘Accept’ versus ‘Decline’ an offer. Both models used the same 44 predictor variables that were available to decision-makers at the time of offer. Median imputation was used for numeric predictors and an ‘Unknown’ category was added to categorical predictors with missing values.7 Predictive performance and variable importance scores were evaluated using stratified Monte Carlo cross-validation. Stratification of offers was based on the listing center transplant rates. Predictions on the hold-out offers were used to compute the out-of-sample area under the ROC curve (AUROC). SHAP (SHapley Additive exPlanations) values were used to measure variable importance.8, 9 Additional details are provided in Appendix S1.
3 RESULTS
3.1 Donor demographics
During the study period, hearts from 5625 pediatric donors resulted in 30 156 offers to 4905 pediatric heart transplant candidates in the US. Of these offers, 88.7% (26 738/30 156) were Declined and there was a final Non-Utilization rate of 39.2% (2207/5625). Table 1 demonstrates donor demographics both for individual offers and the final decision. Donor age demonstrated marked differences in acceptance practices; donors <2 years resulted in the highest utilization rates as compared to a significant, progressive decline in utilization with increasing age. Though individual offer decisions were affected by blood type, final Utilization rates were only slightly higher for O blood type donors (p = .02). Anoxia, head trauma, or stroke were the cause of death listed in 97% of donors. CNS tumor and infection of any type (CNS or ‘general’) were routinely declined and collectively utilized from only 38% of donors, which was less common than all other causes of death (p < .0001). History of CPR was present in 58% of donors and although it did decrease offer acceptance, it did not negatively impact Utilization. The median CPR duration was 24 (12, 40) minutes and there was no statistically detectable difference between whether or not a heart was utilized (utilized 25 (12, 40) minutes versus non-utilized 24 (12, 39), p = .6).
| N (%) (5625) | Total offers (30 156) | Accepted/utilized (3418) | % Offers accepted (11%) | % Donors utilized (61%) | |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 3466 (62%) | 17 881 (59%) | 2090 | 12 | 60 |
| Female | 2159 (38%) | 12 275 (41%) | 1328 | 11 | 62 |
| Race | |||||
| White | 3036 (54%) | 16 086 (53%) | 1793 | 11 | 59 |
| Black | 1324 (24%) | 7315 (24%) | 835 | 11 | 63 |
| Hispanic | 1073 (19%) | 5797 (19%) | 669 | 12 | 62 |
| Other | 192 (3%) | 958 (3%) | 121 | 13 | 63 |
| Age | *** | *** | |||
| <2 | 1575 (28%) | 8379 (28%) | 1282 | 15 | 81 |
| 2–11 | 1980 (35%) | 15 050 (50%) | 1261 | 8 | 64 |
| 11–17 | 2070 (37%) | 6727 (22%) | 875 | 13 | 42 |
| Blood type | ** | ||||
| O | 2913 (52%) | 18 835 (62%) | 1890 | 10 | 65 |
| A | 1914 (34%) | 8661 (29%) | 1102 | 13 | 58 |
| B | 638 (11%) | 2229 (7%) | 352 | 16 | 55 |
| AB | 160 (3%) | 431 (1%) | 74 | 17 | 46 |
| Cause of death | *** | *** | |||
| Anoxia | 2592 (46%) | 16 507 (55%) | 1595 | 10 | 62 |
| Head trauma | 2553 (45%) | 10 412 (35%) | 1570 | 15 | 61 |
| Stroke | 307 (5%) | 1791 (6%) | 174 | 10 | 57 |
| Infection | 66 (1%) | 669 (2%) | 23 | 3 | 35 |
| CNS tumor | 42 (1%) | 315 (1%) | 18 | 6 | 43 |
| Other | 65 (1%) | 462 (2%) | 38 | 8 | 58 |
| CPR | *** | *** | |||
| Yes | 3271 (58%) | 19 395 (64%) | 2033 | 10 | 62 |
| No | 2229 (40%) | 10 128 (34%) | 1312 | 13 | 59 |
| Unknown | 125 (2%) | 633 (2%) | 73 | 12 | 58 |
| Number of inotropes at time of offer | *** | ** | |||
| 0 | 2257 (40%) | 11 628 (39%) | 1409 | 12 | 62 |
| 1 | 1878 (33%) | 10 668 (35%) | 1102 | 10 | 59 |
| 2 | 516 (9%) | 3712 (12%) | 274 | 7 | 53 |
| ≥3 | 192 (3%) | 818 (3%) | 114 | 14 | 59 |
| Missing | 782 (14%) | 3330 (11%) | 519 | 16 | 66 |
- Note: N (%) represents the absolute number and proportion of donors in each category. % offers accepted and % donors utilized refer to the proportion of the variable's subset (i.e., male gender) that was accepted or utilized, respectively. For example, 2090 of the 3466 male donors were utilized (60.3%) and 2090 of the 17 881 male donor offers were accepted (11.6%). Chi-square test was performed to assess intragroup differences, excluding missing values.
- *p < .01, **p < .001, ***p < .0001.
The maximum vasoactive inotropic score prior to the current offer was higher for offers that were declined (declined 15 (5, 40) versus accepted 10 (3, 29.8); p < .001), but this calculated variable was not considered for the predictive models as it is not presently available in DonorNet. Maximum troponin-I values were lower in accepted/utilized (0.1 (0, 0.6)) versus both declined offers (0.3 (0.1, 1.4); p < .001) and non-utilized donors (0.4 (0.1,1.9); p < .001).
3.2 Echocardiographic data
A total of 7810 echocardiograms were evaluated from the 5394 donors with echocardiographic data. Each donor underwent a median of 1 (1, 2) echocardiograms during their terminal hospitalization, with the first occurring 10.8 h (2.1, 20.2) and the final 18.1 h (8.5, 25.3) after DDNC. Composite assessments of ‘normal’ were given to 79% of all final studies in donors with echocardiograms, comprising 89.7% (2943/3280) of all utilized donors and 62.9% (1330/2114) of non-utilized donors (Table 2). Of the 14 287 offers Declined using refusal code 830 (donor age or quality) and 2376 offers Declined using refusal code 837 (organ-specific donor issues), 48% and 34% had normal echocardiograms, respectively.
| N (%) (5394) | Accepted (3280) | % Donors utilized | |
|---|---|---|---|
| Composite assessment | |||
| Normal | 4273 (79%) | 2943 | 69 |
| Abnormal | 1121 (21%) | 337 | 30 |
| Left ventricular dysfunction (Ejection Fraction) | |||
| Mild (45%–55%) | 498 (66%) | 191 | 38 |
| Moderate (35–45) | 163 (22%) | 20 | 12 |
| Severe (<35%) | 97 (13%) | 8 | 8 |
| Left ventricular segmental wall motion abnormality | |||
| Absent | 5148 (95%) | 3207 | 62 |
| Present | 246 (5%) | 73 | 29 |
| ≥Moderate valvar insufficiency | |||
| Absent | 5215 (97%) | 3243 | 62 |
| Present | 179 (3%) | 37 | 21 |
- Note: N (%) represents the absolute number and proportion of candidates in each category for the 5394 donors with echocardiographic information. Data presented here only represent the last study performed for each donor. % donors utilized refers to the proportion of the variable's subset (i.e., normal) that was utilized.
A total of 63 donors demonstrated echocardiographic abnormalities aside from ventricular function or valvar insufficiency, of which 33 were utilized for transplant. Findings of subaortic stenosis, a left ventricular mass, possible rhabdomyosarcoma, prosthetic aortic valve, situs inversus totalis, a history of an ASD repair, history of a VSD repair, possible left ventricular non-compaction cardiomyopathy (4), pulmonary valve stenosis (2) and a right ventricular mass (2) were found in a total of 15 donors, which all were in the non-utilized group. Conversely, 4 different donors in the utilized group demonstrated evidence of a single right coronary artery, prominent left coronary artery, pulmonary artery sling, and circumflex artery arising from the right coronary artery. Of 5 donors on ECMO, 2 were utilized, as were 8/10 donors with small muscular ventricular septal defects, 4/5 with ‘echobright regions’ demonstrated within the left ventricle, 5/7 described as having left ventricular hypertrophy, 2/3 with a ‘right atrial mass’, 2/4 with a ‘mitral valve abnormality’, and 6/10 with a bicommissural aortic valve.
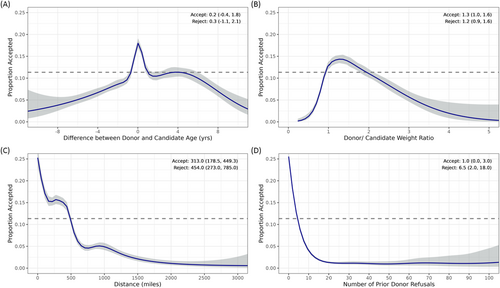
3.3 Offer data
Figure 1 demonstrates the univariate relationships between select donor/candidate data and likelihood to accept. When comparing accepted versus declined offers, age difference and weight ratios were statistically but not clinically different, though there were clear inflection points when donors and candidates had similar ages and weights (Figure 1A,B). Figure 1C demonstrates acceptance inflection points at approximately 250 and 1000 nautical miles, coinciding with two of the four geographical location zones impacting pediatric donor allocation (https://optn.transplant.hrsa.gov/media/eavh5bf3/optn_policies.pdf). The median distance between donor and candidate centers was significantly shorter for accepted offers. Figure 1D demonstrates the marked decline in the likelihood of offer Acceptance with increasing numbers of prior offer refusals.
3.4 Candidate data
Table 3 demonstrates baseline demographics for the 4905 candidates. Candidate race demonstrated a significant intragroup difference for offer Acceptance rates and post hoc analyses demonstrated a trend toward less Black candidates being transplanted as compared to all other races (p = .02). Age <2 years was associated with a higher rate of offer Acceptance but not final transplantation rates as compared to all other age ranges (p = .07), whereas candidates aged >11 were associated with lower offer Acceptance and transplantation rates. Transplantation rates trended lower for candidates with O blood type (p = .011) but higher for those with AB blood type (p = .038). Candidates with cardiomyopathy as their listing diagnosis experienced higher offer Acceptance and transplantation rates than those with congenital heart disease. Of the 1775 candidates with a documented cPRA, 38% (682/1775) were ≥10%; of these, 57% listed CHD as their listing diagnosis.
| N (%) (4905) | Total offers (30 156) | Accepted (3418) | % Offers accepted (11%) | % Candidates transplanted (70%) | |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 2717 (55%) | 16 891 (56%) | 1875 | 11 | 69 |
| Female | 2188 (45%) | 13 265 (44%) | 1543 | 12 | 71 |
| Race | * | ||||
| White | 2632 (54%) | 16 862 (56%) | 1823 | 11 | 69 |
| Black | 959 (20%) | 5401 (18%) | 639 | 12 | 67 |
| Hispanic | 980 (20%) | 5950 (20%) | 711 | 12 | 73 |
| Other | 334 (7%) | 1943 (6%) | 245 | 13 | 73 |
| Age | *** | *** | |||
| <2 | 2096 (43%) | 10 184 (34%) | 1489 | 15** | 71 |
| 2–11 | 1598 (33%) | 14 195 (47%) | 1172 | 8 | 73 |
| 11–17 | 1211 (25%) | 5777 (19%) | 757 | 13*** | 62*** |
| Blood type | ** | ||||
| O | 2303 (47%) | 13 622 (45%) | 1564 | 11 | 68 |
| A | 1754 (36%) | 11 662 (39%) | 1232 | 11 | 70 |
| B | 657 (13%) | 3622 (12%) | 476 | 13 | 72 |
| AB | 191 (4%) | 1250 (4%) | 146 | 12 | 76 |
| Status | *** | *** | |||
| 1A | 3681 (75%) | 19 299 (64%) | 2922 | 15 | 79 |
| 1B | 721 (15%) | 6590 (22%) | 386 | 6 | 54 |
| 2 | 503 (10%) | 4267 (14%) | 110 | 3 | 22 |
| Diagnosis | *** | *** | |||
| CHD | 2604 (53%) | 18 691 (62%) | 1737 | 9 | 67 |
| CM | 2196 (45%) | 10 993 (36%) | 1614 | 15*** | 73*** |
| Other | 105 (2%) | 472 (2%) | 67 | 14 | 64 |
| cPRA | |||||
| <10% | 1093 (22%) | 6478 (21%) | 934 | 14 | 85 |
| ≥10% | 682 (14%) | 5164 (17%) | 567 | 11 | 83 |
| Absent | 3130 (64%) | 18 514 (61%) | 1917 | 10 | 61 |
| Candidate support | |||||
| ECMO | 274 (6%) | 1189 (4%) | 162 | 15 | 73 |
| VAD | 559 (11%) | 2510 (8%) | 409 | 16 | 73 |
| Ventilator | 902 (18%) | 3958 (13%) | 638 | 16 | 71 |
- Note: N (%) represents the absolute number and proportion of candidates in each category. Number offers to accept is the median number (IQR) of offers before acceptance, when it occurred. % offers accepted and % candidates transplanted refers to the proportion of the variable's subset (i.e., male gender) for which offers were accepted or the candidate was transplanted, respectively. For example, 1875 of the 2717 male candidates were transplanted (69%) and 1875 of the 16 891 offers made to male candidates were accepted (11.1%). ECMO, VAD, and ventilator all refer to the percentage of candidates receiving these types of support at the time of listing. Chi-square test was performed to assess intragroup differences.
- Abbreviations: CHD, congenital heart disease; CM, cardiomyopathy; cPRA, calculated panel reactive antibody.
- *p < .01, **p < .001, ***p < .0001.
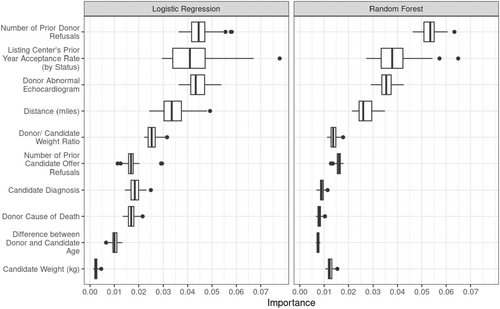
3.5 Modeling results
Table 4 demonstrates the predictive performance of the LR and RF models using different dataset variables. Using donor, candidate, and offer variables, both models demonstrate good predictive performance of likelihood to Accept (AUROC ≥0.83). The performance difference between models is not statistically significant (p = .09), suggesting the added flexibility of RF to incorporate non-linear and interaction effects did not substantially improve prediction. Limiting the dataset to include only candidate or donor variables markedly decreased predictive performance.
| Data | Model type | Mean and 95% CI |
|---|---|---|
| All variables | Logistic regression | 0.839 (0.835, 0.842) |
| All variables | Random forest | 0.836 (0.832, 0.840) |
| Candidate-only variables | Logistic regression | 0.683 (0.675, 0.691) |
| Candidate-only variables | Random forest | 0.672 (0.663, 0.681) |
| Donor-only variables | Logistic regression | 0.720 (0.716, 0.724) |
| Donor-only variables | Random forest | 0.813 (0.809, 0.817) |
| First offer | Logistic regression | 0.723 (0.713, 0.733) |
| First offer | Random forest | 0.724 (0.713, 0.734) |
| Random subset | Logistic regression | 0.820 (0.813, 0.827) |
| Random subset | Random forest | 0.811 (0.802, 0.819) |
- Note: Model performance is demonstrated for both LR and RF models, using different combinations of available datasets. Candidate-only variables included the derived variable of the candidate institution's prior year acceptance practices.
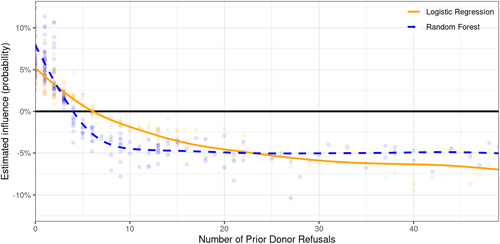
To assess the importance of each predictor variable on the estimated probability of offer acceptance, we produced SHAP variable importance scores. Figure 2 demonstrates the 10 variables with median importance scores >0.01 for either the RF or LR models. The number of prior donor refusals and our derived variable assessing a listing center's prior year acceptance rates were the two most important variables predicting offer acceptance practices, followed closely by whether an echocardiogram was interpreted as normal and distance between donor and candidate centers. As a prior number of refusals was a stronger predictor using the more flexible RF modeling, we evaluated its independent influence on acceptance probability. Figure 3 demonstrates that on initial offers, where the number of prior refusals is 0, acceptance probability increases between 5 (LR) and 8% (RF) as compared to a donor on its 10th offer, in which the likelihood of acceptance has decreased between 7% and 12%. This is further supported by the finding that both RF and LR models lost acceptance practice predictive performance when using only first offers, as seen in Table 4, but largely regain it when using a random subset of subsequent offers, allowing the reintroduction of prior decision bias back into the model.
4 DISCUSSION
Our review of the last decade's acceptance practices demonstrated nearly 90% of all pediatric heart offers to pediatric waitlisted patients are still declined,10 40% of organs are not utilized,3 and for the first time, we have objective evidence that prior refusals are significantly impacting the downstream decisions of other institutions. Further, despite a recent ISHLT consensus statement suggesting echocardiographic assessment of ventricular function is the strongest predictor of post-transplant outcomes,5 60% of discarded pediatric donor hearts were documented to have completely normal findings in their final study. Despite a growing body of evidence demonstrating higher waitlist mortality for children whose listing institutions have either habitually high refusal rates11 or decline hearts accepted on subsequent offers,10 our findings suggest most institutions' default decision is to decline.
Behavioral economics undoubtedly play an important role in these high refusal/ discard rates.12 Although OPTN oversight metrics recently added waitlist mortality, they have historically focused almost exclusively on post-transplant outcomes, producing misguided incentives and risk aversion. This favors lower risk transplant candidates, decreased listing volumes in centers recently flagged for low center performance evaluations,13 and potentially a tolerance for higher waitlist mortality. Our finding that the prior number of refusals was the most important variable impacting subsequent decisions is a classic example of an ‘information cascade’,12 suggesting listing institutions are unduly influenced by the decisions of others, despite studies refuting the impact of prior number of refusals on pediatric heart transplant outcomes.14 Both the RF and LR models performed markedly worse when using only first offers. Though partly due to a significant reduction in offer sample size and potentially from donor instability, it is more likely due to the loss of bias associated with prior offer decisions. This assertion is supported by a significant improvement in predictive accuracy when utilizing a random subset of 4733 offers, allowing the bias of prior decisions to re-enter the model. While research suggests candidate variables are the most important factors in post-transplant outcomes, our models of acceptance practices demonstrate a reduction in predictive power when only using candidate and listing center variables, suggesting donor and offer-specific variables continue to play a large role in institutional practice.
We focused our analyses on pediatric donors to assume a ‘healthier’ and more resilient myocardium than that of the adult donor, with the latter challenged by decades of hypertension, diabetes mellitus, atherosclerosis, and numerous environmental risk factors, reasons commonly resulting in refusal of adult donor hearts.15 Accordingly, though both inotrope exposure and troponin values were higher at the time of declined offers and non-utilized donors, neither variable was found to have significant importance within the predictive models, in keeping with studies refuting their relevance on post-transplant outcomes.16, 17 Further, neither CPR history, present in nearly 60% of donors in our study, nor its duration, negatively impacted donor utilization, a decision supported by several prior studies.17-19 Distance between donor and candidate, a surrogate for donor ischemic time, was predictably an important variable in acceptance/utilization decisions, but this will hopefully decline with the advent of pediatric-specific organ transport technology. Donor age, a relative surrogate for organ size and possibly anticipated functional resilience remains important with a >80% utilization rate for hearts from donors less than 2 as compared to only 42% in the adolescent population, suggesting adolescent donor utilization should be a focus of future research. This assertion is supported by the fact that 61% of the adolescent donors declined by pediatric centers were ultimately utilized for adult candidates, suggesting more rigid donor criteria utilization by pediatric centers. Finally, though not meeting our p-value cut-off of <.01, post-hoc analyses suggested Black candidates were transplanted at a lower rate than all other races. Although equity in transplant is slowly getting the attention it requires, there definitely remains room for improvement.20, 21
By reviewing the entirety of available echocardiographic reports, we also present the most complete representation of cardiac function ever assessed in pediatric heart donors. Recent publications5, 6 concluded that in the setting of a ‘normal echocardiogram’, aside possibly from a cerebrovascular accident as the cause of death or donor ischemic time greater than 4 h, no other donor characteristics were associated with recipient outcomes. It is important to recognize, however, that many of these assertions were derived from adult or small pediatric studies, none specifically assessing the impact of echocardiographic measurements of function on recipient outcomes, and that the sole measurement of function was a final available LVEF. Our composite echocardiogram assessment incorporating quantitative/qualitative measurements of ventricular function, LVSWMA, and valvar insufficiency, was able to account for differences between a completely normal study and one documenting a left ventricular ejection fraction >55% but with LVSWMA or moderate mitral valve insufficiency, a distinction lost in prior studies.
A ‘normal’ final echocardiogram was observed for nearly 90% of all utilized hearts, but more notably in 60% of non-utilized organs. While even high donor organ acceptance rate centers must sometimes decline an otherwise acceptable organ for logistical challenges, excessive distance, donor/candidate size mismatch, or candidate instability, it is difficult to conceive that these issues compromised the utilization of 23.6% of the pediatric heart donor population. This becomes further troubling when considering the impact on subsequent institutions' acceptance patterns, as refusal codes 830 or 837 were utilized in the setting of normal echocardiograms for over 7600 offers.
Our analyses demonstrate that prior institutions' organ acceptance practices are unduly influencing decisions for subsequent institutions and as such, we would propose waitlisted patients may benefit from this data being thoughtfully phased out from DonorNet. Though this would remove an approximation of competing candidates for listing institutions, it could be offset by providing such data after making a decision or routinely providing the number of other donors with corresponding weight ranges and blood types within the candidate's institutional travel radius. OPOs would not need to be blinded to this information, which is necessary to produce ‘back up’ or ‘standby’ offer calls to institutions whose candidates are next on the list. Though such a proposition would require acceptance from all 11 UNOS regions and likely meet significant resistance, our data suggest this information cascade may be responsible for nearly 25% of the pediatric heart donor pool being discarded despite a completely normal echocardiogram.
4.1 Limitations
Our study has two important sets of limitations. The first relates to echocardiographic data. No studies were found for 4.5% of donors. As it is highly unlikely institutions would utilize a heart without an echocardiogram and over 60% of these donors, or 4.7% of all donors whose hearts were ultimately accepted did not have a documented echocardiogram, it is almost certain these studies were simply missed or not available, which also suggests studies may be missing for other donors. Additionally, all echocardiogram interpretations are taken directly from the local cardiologist's interpretations. Several studies have demonstrated marked discordance in functional assessments when local studies are reviewed by an experienced core lab,22, 23 but this was not possible for our study.
The second set of limitations relates to the challenges of analyzing and modeling observational databases, aside from the inherent issues of data reliability and missing values. We limited our population to pediatric donors offered to pediatric candidates, necessarily removing any information regarding donors accepted for US adult or Canadian pediatric candidates, which occurred in almost 40% of the 2207 pediatric donors not utilized for a US pediatric candidate. Secondly, it is important to note that the SHAP importance scores reflect an aggregate acceptance practice. Variables with high importance do not necessarily imply that all centers consider them strongly and conversely, variables with lower importance scores may be strongly utilized by other centers. Finally, after careful consideration of variable correlation and collinearity, we chose to model 44 of the more than 150 different donor, candidate and offer specific variables and as a result, may not have included variables some institutions are using for decision-making; conversely, this should have helped minimize the risk of model overfitting.
In conclusion, our data confirm prior findings that pediatric heart donor pool utilization remains low in the United States. For the first time, however, we have demonstrated both the potential viability of those organs being discarded and the negative downstream influence institutions' decisions have on subsequent offers. We believe more research is needed to assess the utility of removing this information on both donor acceptance practices and post-transplant outcomes.
AUTHOR CONTRIBUTIONS
All authors (M.M., L.A., S.W., F.H., M.P.) have contributed to the design, analysis, and interpretation of data; drafting of the manuscript; and participated in the final approval of the manuscript submitted.
ACKNOWLEDGMENTS
Research reported in this publication was supported in part by the University of Virginia Center for Engineering in Medicine, Jefferson Trust, and the National Center for Advancing Translational Sciences of the National Institutes of Health (Award Number UL1TR003015). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
CONFLICT OF INTEREST STATEMENT
None of the authors have any disclosures or conflicts of interest to report.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.