Assessing the utility of ultrasound-guided vascular access placement with longer catheters in critically ill pediatric patients
Section Editor: Francis Veyckemans
Abstract
Background
Critically ill pediatric patients can have difficulty with establishing and maintaining stable vascular access. A long-dwelling peripheral intravenous catheter placement decreases the need for additional vascular interventions.
Aim
The study sought to compare longevity, catheter-associated complications, and the need for additional vascular interventions when using ultrasound-guided longer peripheral intravenous catheters comparing to a traditional approach using standard-sized peripheral intravenous catheters in pediatric critically ill patients with difficult vascular access.
Methods
This single-center retrospective cohort study included children 0–18 years of age with difficult vascular access admitted to the pediatric intensive care unit between 01/01/2018–06/01/2021.
Results
One hundred and eighty seven placements were included in the study, with 99 ultrasound-guided long intravenous catheters placed and 88 traditionally placed standard-sized intravenous catheters. In the univariate analysis, patients in the traditional approach were at a higher risk of intravenous failure compared to those in the ultrasound-guided approach (HR = 2.20, 95% CI [1.45–3.34], p = .001), with median intravenous survival times of 108 and 219 h, respectively. Adjusting for age, patients in the traditional approach remained at higher risk of intravenous failure (HR = 1.99, 95% CI: [1.28–3.08], p = .002). Adjusting for hospital length of stay, patients in the ultrasound-guided approach were less likely to have additional peripheral intravenous access placed during hospitalization (OR = 0.39, 95% CI [0.18–0.85] p = .017).
Conclusion
In critically ill pediatric patients with difficult vascular access, ultrasound-guided long peripheral intravenous catheters provide an alternative to traditional approach standard-sized intravenous catheters with improved longevity, lower failure rates, and reduced need for additional vascular interventions.
What is already known about the topic?
Establishing and maintaining stable vascular access can be difficult in critically ill pediatric patients. Very few existing studies have investigated potential advantages of ultrasound-guided long peripheral intravenous catheters in critically ill pediatric patients.
What new information this study adds
The study identifies the advantages of placing longer intravenous catheters with ultrasound guidance.
1 INTRODUCTION
The establishment and maintenance of stable vascular access in critically ill children with complex operations, multiple co-morbidities, and frequent hospitalizations can be challenging for several reasons, including small caliber veins, limited access sites, and high emotional stress from the child and family. Recent estimates suggest that catheter dwell time in pediatric patients with traditional, standard length catheter placement ranges between 2–3 days, with a rapid increase in malfunction following 48 h.1 With an estimated median pediatric intensive care unit length of stay of 2 days in North America, such access may not carry patients through ICU admission, potentially causing interruptions in therapy and requiring additional interventions to maintain access.2 The use of ultrasound guidance to enhance first-pass success with peripheral intravenous catheter placement is now well established in both adult and pediatric emergency medicine literature.3-6 The relationship however between an ultrasound-guided peripheral intravenous catheter approach and catheter longevity has been less studied and with inconsistent results. Adult literature suggests a high failure rate of ultrasound-guided peripheral intravenous catheter placement at 48 h, correlating failure rate to the depth of vessel cannulated.7 A recent pediatric randomized control trial comparing ultrasound-guided peripheral intravenous catheter to traditional approaches showed dwell time to extend by 5 days with the use of ultrasound; however, unlike the adult study, longer catheters were used in many of those cannulated with ultrasound guidance.3
This study hypothesizes that placing ultrasound-guided long peripheral intravenous catheters in the pediatric intensive care unit will lead to significantly longer dwell times, with improved longevity, lower failure rates, and reduced need for additional vascular interventions when compared to a traditional approach to standard-sized peripheral intravenous catheter placement.
Our approach is unique in its exclusive use of longer peripheral intravenous catheters in the ultrasound group and its focus on pediatric critically ill patients.
2 METHODS
2.1 Study design and setting
This was a retrospective cohort study in a tertiary 25-bed combined cardiac and pediatric intensive care unit comparing ultrasound-guided long peripheral intravenous catheters to traditional approach standard-sized peripheral intravenous catheters in children with difficult vascular access.
2.2 Selection of participants
Patients were eligible if admitted to the pediatric intensive care unit, needed peripheral venous access, and were deemed to have difficult access by the bedside nursing team between 01/01/2018 and 06/01/2021. IRB approval was obtained by Cleveland Clinic IRB (#21–901) following review.
2.3 Definitions
The standard-sized peripheral intravenous catheters were defined as 24 Ga. 1.9 cm, 22 Ga. 2.5 cm, 20 Ga. 3.2 cm. The long peripheral intravenous catheters were defined as 24 Ga. 3.2 cm, 22 Ga 4.4 cm, and 20 Ga 4.4 cm. Determination of difficult vascular access was made at the discretion of the ICU nursing team, often after being unable to place a peripheral intravenous catheter within two attempts. Traditional approaches for placement of intravenous catheters included the use of landmarks, palpation of the vein, and the use of a vein illuminator. Ultrasound-guided approach for placement of intravenous catheters involved a dynamic approach, with a combination of either short or long-axis techniques, depending on proceduralist preference.
2.4 Interventions
The vascular access team or intensivists were contacted for placement of peripheral intravenous access in the difficult vascular access patients. The vascular access team used a traditional approach through 2018, and later transitioned to an ultrasound-guided approach following a standardized ultrasound-guided vascular access course and regular practice sessions. Intensivists exclusively used an ultrasound-guided approach, receiving formal training through a workshop, frequent practice sessions, and twice-yearly assessments of skills in the simulation laboratory.
Machines used for placement included both the General Electric Venue 50 and Logiq e machines, with the use of either L 8-18i or L10-22 linear transducers (General Electric). Veins were scanned with ultrasound for the most appropriate access site before peripheral intravenous catheter placement, at the discretion of the proceduralist.
2.5 Outcome measures
The primary outcome measure was defined as dwell time in hours of the catheter during hospitalization and the secondary outcomes included complication rates (infiltration, catheter integrity, leak, occlusion, site tenderness, bleeding, or unplanned removal (defined as the inadvertent or deliberate displacement of the catheter by patient or other factors prior to completion of therapy)) and the need for additional intravenous access following placement in the intensive care unit.
2.6 Data analysis
Continuous variables were summarized as medians (25th, 75th percentile) and categorical variables as frequency (percent). Demographics, clinical characteristics, successful intravenous catheter placement, complications, need for additional vascular access interventions following placement, were compared between ultrasound-guided long peripheral intravenous catheters and traditional approach standard-sized peripheral intravenous catheters by utilizing the Wilcoxon rank-sum test for continuous/ordinal characteristics and the Pearson's chi-square test or Fisher's exact test for categorical characteristics, as appropriate. To estimate the 95% confidence interval (CI) for difference in median age between the long and traditional catheter groups, the quantile regression modeling on the median age was used with the rank method under the simplex algorithm. The Kaplan–Meier plot was constructed to depict time to all-cause intravenous catheter failure. The log-rank test was used to compare unadjusted intravenous catheter survival between the long and standard-sized catheter groups. The Cox proportional hazards model was performed to assess the associations between intravenous catheter failure and the corresponding placement technique and to estimate unadjusted and adjusted hazard ratios (HRs) with 95% CIs. The catheter group and baseline age were included in the multivariable Cox proportional hazards model. The multinomial logistic regression model was used to access the association between the additional IV access and the catheter groups after adjusting for the length of stay and to estimate adjusted odd ratios (ORs) with 95% CIs.
All analyses were performed on a complete-case basis; subjects with missing data on particular variables were only excluded for analyses in which those variables were used. All tests were 2-tailed and were performed at an overall significance level of 0.05. SAS 9.4 software (SAS Institute) was used for all analyses and plots.
3 RESULTS
Included in the ultrasound-guided long peripheral intravenous catheters group were 99 placements compared to 88 in the traditional approach standard-sized peripheral intravenous catheter, with a median age of 58 versus 10 months (95% CI for difference in medians [15–81], p = .001) between long and traditional groups, respectively. Traditional approach standard-sized peripheral intravenous catheter placement location was more often in the hand (35.2%) followed by the forearm (26.1%), whereas in the ultrasound-guided long peripheral intravenous catheters group was more often in the forearm (55.6%) followed by the upper arm (36.4%). See Table 1 for further baseline comparisons.
| Study variable | Overall (n = 187) | USGPIV (n = 99) | Traditional (n = 88) | p-Value |
|---|---|---|---|---|
| Age (months) | 33.0 [6.0, 121] | 58.0 [17.0, 154.0] | 10.0 [1.0, 80.0] | .001 |
| PICU LOS (days) | 6.0 [3.0,12.0] | 5.0 [2.0, 11.0] | 6.5 [3.0, 13.5] | .29 |
| Hospital LOS (days) | 12.0 [6.0, 30.0] | 12.0 [6.0, 30.0] | 14.0 [7.0, 31.0] | .77 |
| Reason for ICU admission | ||||
| Post-op cardiac surgery | 26 (13.9) | 8 (8.1) | 18 (20.5) | |
| Acute respiratory failure | 51 (27.3) | 28 (28.3) | 23 (26.1) | |
| Status Epilepticus | 7 (3.7) | 1 (1.0) | 6 (6.8) | |
| Diabetic Ketoacidosis | 9 (4.8) | 6 (6.1) | 3 (3.4) | |
| Sepsis | 19 (10.2) | 16 (16.2) | 3 (3.4) | |
| Acute Heart Failure | 11 (5.9) | 10 (10.1) | 1 (1.1) | |
| Other | 64 (34.2) | 30 (30.2) | 34 (38.7) | |
| PIV location (N,%) | ||||
| Upper Arm | 37 (19.8) | 36 (36.4) | 1 (1.1) | |
| Forearm | 78 (41.7) | 55 (55.6) | 23 (26.1) | |
| Scalp | 7 (3.7) | 0 (0) | 7 (8.0) | |
| Hand | 33 (17.6) | 2 (2.0) | 31 (35.2) | |
| Leg | 12 (6.4) | 6 (6.1) | 6 (6.8) | |
| Foot | 20 (10.7) | 0 (0) | 20 (22.7) | |
| Operator background (N,%) | ||||
| MD | 65 (34.8) | 65 (65.7) | 0 (0) | |
| VATa | 122 (65.2) | 34 (34.3) | 88 (100) | |
- a VAT refers to vascular access team.
The median intravenous survival times in the long and traditional catheter groups were 219 (95% CI [142, 312]) and 108 (95% CI [72, 149]) hours, respectively; patients in the traditional group were at a higher risk of intravenous catheter failure than those in the long catheter group (unadjusted HR = 2.20, 95% CI [1.45–3.34], log rank p = .001), with 3- day intravenous catheter survival at 59.5% and 83.0%, respectively (Figure 1). Adjusting for age, patients in the traditional catheter group remained at higher risk of intravenous catheter failure (HR = 1.99, 95% CI: [1.28–3.08] p = .002). Adjusting for hospital length of stay, patients in the ultrasound-guided catheter group were less likely to have additional peripheral intravenous access placed during hospitalization (OR = 0.39, 95% CI [0.18–0.85]. p = .017); however, no significant difference was found between the need for additional central venous line placement between groups (OR = 0.76, 95% CI [0.28–2.1] p = .60).
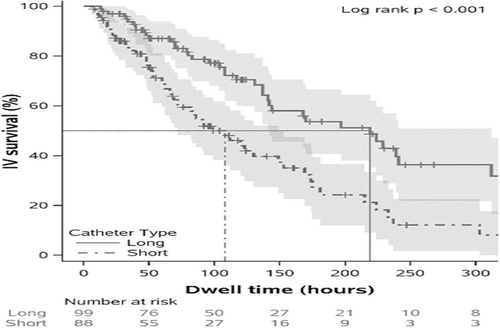
Among reasons for premature intravenous catheter removal, 19.3% of short intravenous catheter placements were related to unplanned removal compared to 7.1% in the ultrasound-guided group (see Table 2). Complication rates otherwise were similar between the ultrasound-guided and standard groups, but not analyzed for statistical significance due to limited numbers of observations.
| Reasons for IV removal | Overall (N,%) | USGPIV (n = 99) | Traditional (n = 88) |
|---|---|---|---|
| Completion of therapy | 93 (51.1) | 58 (59.2) | 35 (41.7) |
| Infiltration | 29 (15.9) | 14 (14.3) | 15 (17.9) |
| Impaired catheter integrity | 9 (4.9) | 5 (5.1) | 4 (4.8) |
| Site tenderness | 7 (3.8) | 5 (5.1) | 2 (2.4) |
| Catheter leak | 6 (3.3) | 3 (3.1) | 3 (3.6) |
| Unplanned removal | 24 (13.2) | 7 (7.1) | 17 (20.2) |
| Catheter occlusion | 10 (5.5) | 5 (5.1) | 5 (6.0) |
| Bleeding at the insertion site | 2 (1.1) | 0 (0) | 2 (2.4) |
| Unknown | 2 (1.1) | 1 (1.0) | 1 (1.2) |
4 DISCUSSION
This study found that placement of peripheral intravenous catheters by pairing ultrasound guidance with long catheters in critically ill children increased intravenous catheter longevity, success through the completion of therapy and decreased need for additional vascular interventions during the remainder of hospitalization with less complication rates when compared to a traditional approach. These results are consistent with the results of recent pediatric emergency medicine studies. Vinograd et al. retrospectively studied 300 patients receiving the ultrasound-guided peripheral intravenous catheters and found a median dwell time of 143 h and a failure rate at 48 h of only 25%, although not directly comparing this to a traditional intravenous catheter placement control group.3 A subsequent age-stratified randomized control trial of 167 patients by the same author found a median dwell time of 7.3 days in the ultrasound-guided placement versus 2.3 days in traditional placements. Both studies, while favoring the use of longer peripheral intravenous catheters in the ultrasound groups, did not fully control for this variable.6 Contrary to these data, existing adult and pediatric literature suggests that ultrasound-guided peripheral intravenous catheters may be associated with a higher failure rate.7-9
Investigating reasons for this, Fields et al. found that vessel depth and location accounted for this higher rate, with deeper and more proximal vessel cannulation constituting the majority of early failure rate when using standard peripheral intravenous catheters.10 Associating ultrasound guidance to select the optimal and often deeper vein with the use of a longer catheter to ensure its adequate seating within the vein could avoid this cause of failure, and may explain the differences in the ultrasound-guided success between existing pediatric and adult literature. Our data support this idea, as more ultrasound-guided peripheral intravenous catheters were placed in the oftentimes deeper forearm and upper arm locations while still maintaining greater longevity.11-13
Intravenous catheter placement in pediatric patients is a known stressor to both patients and families and adds to the cumulative trauma of patients admitted to the pediatric intensive care unit.14 Improved first pass success has clearly been linked with the use of ultrasound guidance in the pediatric literature, highlighting the superiority of this approach. Likewise, multiple pediatric studies have indicated ultrasound guidance can be successfully taught to a wide variety of care providers.15-19 A recent study of >4000 hospitalized infants and children indicated that roughly 50% need 2–4 peripheral intravenous access placed during hospitalization with 1–2 catheters placed per week, suggesting that focusing on intravenous catheter longevity likewise could minimize additional catheter-related hospital trauma.20 While we found a significant decrease in the need for additional peripheral intravenous access, the need for central venous lines remained the same between groups. Shokoohi et al. found a 5%–8% reduction in the need for central venous lines following the implementation of an emergency medicine ultrasound-guided vascular access program, although the reduction was only 0.9% in the subpopulation of critically ill patients.21
4.1 Limitations
There are several limitations to our study. While involving only pediatric patients deemed to have difficult access, the recognition of this was based upon subjective bedside nursing assessment rather than an algorithmic approach to recognition. Consistently using pediatric-specific scoring systems in the available literature such as the difficult vascular access score (DIVA) may allow for a standardized approach to isolating children with difficult access.22 Secondly, the focus of our research was on intravenous catheter longevity, and data regarding attempts at placement was not consistently recorded in available documentation for review/analysis. Thirdly, patients in the ultrasound-guided group were significantly older than the traditional group, although subsequent multivariate analysis was used to control for this factor. The reasons for this are unclear but may relate to less comfort among proceduralists using the newer skill set of an ultrasound-guided approach in neonates and young infants. Also, while documentation of medication and infusion types were not captured as contributors to IV longevity, strict hospital policy was followed regarding appropriate type and administration of medications through the long IVs, which were uniformly treated as standard peripheral IVs. In addition, the use of the vascular access team exclusively for the traditional intravenous catheter placements and a majority of intensivists for the ultrasound-guided peripheral intravenous catheter group may have introduced bias, although a similar approach to ultrasound placement was used in both groups. An increased proportion of ultrasound-guided peripheral intravenous catheter patients was also cannulated in deeper and more proximal vessels. While this approach, along with the use of a longer intravenous catheter likely accounts for our results, routine use of upper arm vessels for peripheral access should be thoughtfully approached given the potential value of preservation for peripherally inserted central venous cannulation. In this context, risk/benefit analysis must be carefully weighed, taking into account underlying patient conditions and course of illness. Lastly, while the low reported complication rates were not amenable to statistical analysis, it should be recognized in the adult literature that midline catheters may be more prone to thrombosis than standard intravenous catheters. The use of single lumen longer catheters with the same diameter as the standard catheters may have minimized this risk in the study, as adult literature suggest both dual lumen catheters and increased catheter diameters to be two independent risk factors for midline catheter-associated thrombosis.23
5 CONCLUSIONS
The use of ultrasound-guided long peripheral intravenous catheters in a pediatric intensive care unit was associated with a markedly longer intravenous catheter longevity, less need for additional peripheral intravenous access, and a comparable complication rate when compared to a traditional approach. Further prospective studies strictly controlling for operator experience/training and focusing additionally upon details of insertion technique may aid in further supporting our approach to maintaining stable access and minimizing harm in critically ill children.
AUTHOR CONTRIBUTIONS
RS participated in literature search, data collection, manuscript preparation, and review of the manuscript. AG and CF both participated in manuscript preparation and review. WL participated in statistical method development and analysis of data. WH participated in literature search, study design, data collection, and analysis of data, manuscript preparation, and review of manuscript.
FUNDING INFORMATION
No additional funding required.
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interest relevant to this article to disclosure.
ETHICS APPROVAL STATEMENT
IRB approval was obtained by Cleveland Clinic IRB (#21–901) following review.
CONSENT FOR PUBLICATION
None indicated.
Open Research
DATA AVAILABILITY STATEMENT
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.