Total Hip Arthroplasty Stems and Femur Strain During Implant Insertion: A Biomechanical Study of Single Taper, Double Taper, and Collared Monolithic Stems
Funding: This work was supported by the University of Connecticut. Smith and Nephew (London, UK) provided the instrumentation and implants; the company had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; nor in the decision to submit the article for publication. Internal funds were used to acquire the cadaveric specimens and cover all other associated costs.
ABSTRACT
Objective
In total hip arthroplasty (THA), intraoperative periprosthetic femoral fracture (IOPFF) is a significant concern, often occurring during femoral canal instrumentation and stem implantation due to proximal femur strain. However, the impact of different stem designs on this strain remains unclear. This study conducted a biomechanical analysis comparing strain patterns on the proximal femur during the implantation of three stem types: single taper, double taper, and collared stems. This study aims to explore if there is a difference in strain patterns placed on the proximal femur during the implantation of three different stem types: single taper, double taper, and collared stems?
Methods
There were 24 cadaveric femurs randomly assigned to three groups based on implant geometry: Smith and Nephew anthology (single taper), synergy (double taper), and polar (collared) stems. Strain gauges were placed on the proximal femur to measure strain during implantation in both horizontal and vertical directions. Peak strain, the difference between maximum strain at final impaction and baseline, was recorded. The Kruskal–Wallis test compared peak strain between stem designs.
Results
At the medial proximal femur, collared stems produced compressive strain (−276) in the horizontal vector, differing significantly from the tensile strain generated by single (41, p = 0.009) and double taper stems (218.5, p = 0.003). No significant strain difference existed between single and double taper stems at the medial proximal femur. At the lateral proximal femur, double taper stem impaction resulted in compressive strain (−69), significantly differing from the tensile strain produced by single taper (221, p = 0.024) and collared stem impaction (462, p = 0.009). No strain differences were observed in other tested areas.
Conclusion
This study highlights distinct strain patterns at the medial and lateral proximal femur depending on the stem type. Collared stems induce compressive strain at the medial proximal femur, while double taper stems result in compressive strain at the lateral proximal femur. Understanding these differences may help reduce IOPFF risk in THA procedures. Based on these findings, the use of collard stems would be preferable over single or double taper stems in elderly patients with suboptimal bone quality, as it reduces strain on the medial cortex and improves immediate stability.
1 Introduction
Total hip arthroplasty (THA) continues to be a highly successful operation with excellent clinical outcomes [1]. Complications are rare but can be associated with diminished patient-reported outcomes and surgical satisfaction. One such preventable complication is intraoperative periprosthetic femoral fracture (IOPFF), occurring in 1%–5% of primary THA [2, 3]. These most often occur during instrumentation of the femoral canal and stem implantation, when the proximal femur encounters the greatest circumferential strain [2, 4]. The risk of IOPFF is further increased by the use of cementless femoral implants that achieve stability through press-fit fixation, which remains ubiquitous in clinical practice, with recent American Joint Replacement Registry data reporting over 95% of elective primary THAs utilizing cementless metaphyseal fixation [2, 5, 6]. IOPFF has been correlated to an increased risk of postoperative periprosthetic femur fracture and increased risk of revision THA [7-9]. Furthermore, even with properly treated IOPFF, typical primary cementless implants may have reduced survivorship following intraoperative fracture secondary to failed or fibrous ingrowth, or postoperative stem subsidence [2-9].
Mitigating the risk of IOPFF through an understanding of the modifiable and nonmodifiable risk factors associated with intraoperative fracture may reduce patient morbidity and improve implant survival. Female sex, increasing age, poor bone quality, and abnormal proximal femur morphology have been identified as nonmodifiable risk factors [2, 7, 8, 10]. Modifiable risk factors implicated in increased risk of IOPFF include surgical approach (direct anterior and direct lateral) and cementless stem fixation [7, 11]. The single taper, double taper, and collared stems areamong the most commonly used stem designs in primary cementless THA. However, there remains a paucity of literature investigating the IOPFF risk associated with these three common stem geometries. As such, the purpose of this study was to (i) compare proximal femoral strain patterns during implantation of three commonly used uncemented THA stems—single taper, double taper, and collared designs—using a standardized cadaveric biomechanical model. The goal was to determine if stem geometry influences strain distribution and correlates with the risk of IOPFF, (ii) furthermore, another goal of this study was to evaluate the horizontal and vertical strain placed at specific anatomic locations of the proximal femur to identify key regions that may be prone to IOPFF, and (iii) lastly, a purpose of this study was to elucidate a biomechanical rational for implant design selection based on the strain placed on the proximal femur during implant impaction. These results may help guide future clinical studies and promote design specific implants and guidelines to minimize IOPFF and improve outcomes of primary uncemented THA.
2 Materials and Methods
2.1 Specimen Characteristics
A total of 24 fresh-frozen human cadaveric femurs were procured. Specimens were excluded if they had evidence of trauma or a prior surgical procedure, which was inferred by direct inspection of the osseous specimens for deformity or implants. Dual X-ray absorptiometry (DEXA) scans measured the bone mineral density (BMD) of each femur at the greater trochanter and lesser trochanter. Femurs were then randomly assigned to three groups of stem geometry utilizing computer randomization: single (medial-to-lateral) taper, double taper (fit-and-fill), or collared stem.
2.2 Stem Characteristics
Broaches and implants were provided by Smith and Nephew (London, UK). Group 1 was randomized to the“Anthology” (Smith and Nephew, London UK) stem, serving as a proxy for Mont Type 1, single medial to lateral taper with proximal porous coating (Figure 1A) [12, 13]. Group 2 was randomized to the “Synergy” (Smith and Nephew, London UK) stem, representing typical double taper Mont Type 2 stems (Figure 1B) [14]. Finally, Group 3 was randomized to a collared stem, representing Mont Type 3C, for which the “Polar” (Smith and Nephew, London UK) stem was utilized (Figure 1C) [10, 15].
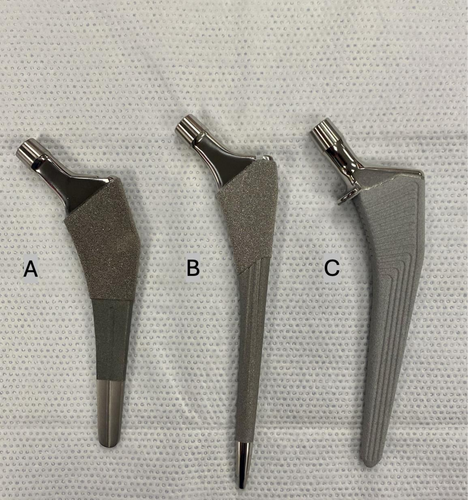
The three different monolithic femoral implants tested in this study are widely used in the field of arthroplasty. The “Anthology” stem used in Group 1 has demonstrated satisfactory clinical outcomes, with a reported stem survival rate of 99% over a follow-up period exceeding 20 years [12, 13] (Figure 1A). The “Synergy” stem used in Group 2, representing typical Mont Type 2 stems, is proximally porous coated with medial-to-lateral and anterior-to-posterior taper geometry [14] (Figure 1B). This design aims to achieve fixation by contacting the medial and lateral metaphyseal cortex, as well as the anterior and posterior metaphyseal cortex. In comparison to the Type 1 stem, it has a relatively thicker profile in the anterior–posterior plane and fills a larger surface area of the femoral metaphysis, giving rise to its “fit-and-fill” name. Clinical reports have indicated a Type 2 stem survival rate of approximately 95%–100% over a follow-up period of 15–20 years [12]. Lastly, Group 3 had the “Polar” stem implanted, which is a collared stem, representing a Mont Type 3C stem [10]. The Polar collared stem is fully titanium and hydroxyapatite coated with a proximal collar (Figure 1C). These stems have a rectangular cross-section that provides robust rotational stability with all four corners press-fitting into endosteal bone. As they extend distally, both the anterior–posterior and mediolateral planes taper in a wedge shape. The fixation of these Type 3C stems primarily occurs at the junction between the femoral metaphysis and diaphysis, as well as at the proximal part of the diaphysis, enabling three-point fixation in the sagittal plane. This type of stem has demonstrated satisfactory clinical outcomes with a stem survival rate of greater than 95% over a follow-up period exceeding 20 years [12, 15].
2.3 ImplantTemplating and Selection
All stems were implanted under the guidance of the senior author (O.S.), a fellowship-trained arthroplasty surgeon. X-rays of the femurs were obtained to digitally template the stems with OrthoView (Jacksonville, Florida, USA) software. All remaining soft tissue was removed from the femurs prior to instrumentation. The femoral neck cuts were performed 10 mm above the lesser trochanter and carried to the saddle of the greater trochanter with the assistance of the appropriate osteotomy guide. The femurs were then instrumented with implant-specific instrumentation sets. The decision of final broach size was made with a combination of the digitally templated stem sizes and clinical judgment. No fractures occurred during instrumentation or stem implantation.
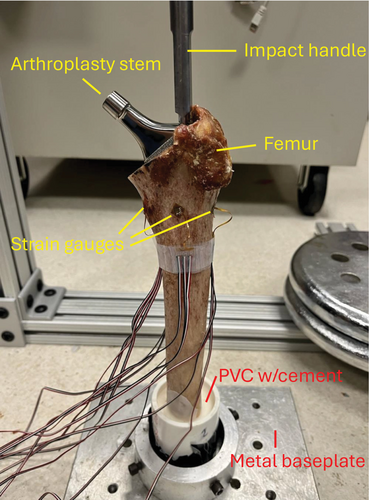
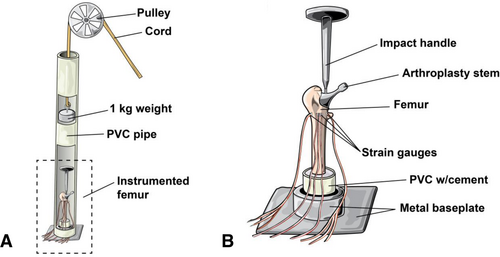
2.4 Experimental Setup
The femurs were potted with polymethyl methacrylate (PMMA) into 3-in. diameter polyvinylchloride (PVC) tubes so that the tip of the greater trochanter was 12 in. above the base of the PVC tube for all test subjects (Figure 2). The testing apparatus was assembled to reproducibly create an impaction force upon the insertion handle similar to that in previous biomechanical literature [16]. After manually broaching to the correct size, guided by digital templating and clinical judgment, theone of the three matching stem designs (Figure 1) was hand-inserted until the top of its ingrowth surface stood 5 mm above the neck cut. A 48-in. polyvinylchloride tube housed a 1-kg weight attached to a pulley that was dropped from height of 1 meterto produce the final stem impaction force (Figures 2 and 3). To maintain a consistent 1-m drop height for all tests, the weight's drop height was adjusted based on slight variations in the length of the inserter handles for each stem type. Strain gauges (rosette 350 Ohm strain gauges (Vishay, Raleigh, NC)) were affixed to the anterior, medial, posterior, and lateral proximal femur to measure the strain generated byfinal stem impaction in the horizontal and vertical directions (Figure 2). Strain was recorded with data acquisition software. The measurement of strain is unitless. In our experimental setup, a positive value indicated a tensile strain while a negative value indicated a compressive strain. Immediately prior to testing, the potted femurs with attached strain gaugeswere allowed to come to room temperature and then placed into a base and affixed with bolts to ensure a secure fit.
2.5 Data Analyses
Baseline demographic characteristics, including age, sex, race, and BMD, were compared between stem groups using the Kruskal–Wallis and chi-square tests, where appropriate. Peak strain, calculated as the difference between maximum strain at final impaction and baseline strain, was compared between stem designs for each vector orientation (anterior, posterior, medial, and lateral) utilizingthe Kruskal–Wallis test. For significant differences identified from global testing with Kruskal–Wallis, wethen conducted pairwise comparisonsusing the Deans–Steel–Critchlow–Fligner test. p-values < 0.05 were considered statistically significant. Data management and analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC).
3 Results
3.1 Demographics
Of the 24 fresh-frozen human cadaveric femurs used in this study, the mean donor age was 63 years, with a standard deviation of ±10 years, and ages ranged from 45 to 80 years. There were 14 specimens from men and 10 from women. There were 18 Caucasian specimens, and six were African American. There were no differences in age, sex, and race between the three groups. There were no differences between groups in BMD (Table 1).
| Demographics | ||||
|---|---|---|---|---|
| Single taper | Double taper | Collared | p | |
| Age (median) | 58.25 | 65.75 | 64.5 | 0.289 |
| Sex (n, %) | 0.805 | |||
| Men | 6 (75) | 5 (63) | 3 (37) | |
| Women | 2 (25) | 3 (37) | 5 (63) | |
| Race (n, %) | 0.401 | |||
| Caucasian | 7 (88) | 5 (63) | 6 (75) | |
| African American | 1 (12) | 3 (37) | 2 (25) | |
| BMD (median, IQR)a | ||||
| Lesser trochanter | 1.30 (1.11–1.77) | 1.49 (1.42–1.69) | 1.50 (1.34–1.79) | 0.385 |
| Greater trochanter | 0.51 (0.45–0.61) | 0.51 (0.31–0.70) | 0.59 (0.47–0.78) | 0.677 |
- a BMD, bone mineral density in g/cm2; IQR, interquartile range.
3.2 Horizontal Strain on Medial Proximal Femur
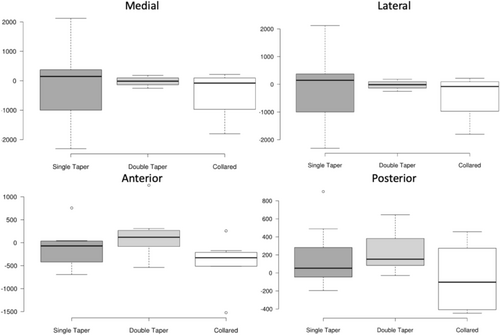
At the medial proximal femur, the collared stem produced compressive strain (−276) in the horizontal vector at final impaction, differing significantly from the tensile strain generated by the single (41, p = 0.009) and double taper stems (218.5, p = 0.003) (Figure 4). No significant difference in strain existed between the single and double taper stems at the medial proximal femur in the horizontal vector (41 vs. 218.5, p = 0.545).

3.3 Horizontal Strain on Lateral Proximal Femur
At the lateral proximal femur, double taper stem impaction resulted in compressive strain (−69), significantly differing from the tensile strain produced by single taper (221, p = 0.024) and collared stem impaction (462, p = 0.009). There was no difference in strain observed between the collared and singletaper stems at the lateral proximal femur in the horizontal vector (462 vs. 221, p = 0.859).
3.4 Anterior and Posterior Horizontal Strain and Vertical Strain
There was no difference in proximal femur strain generated by the three stems in the horizontal vector at either the anterior or posterior femur (Figure 4). Additionally, there were no differences in strain between the three stems in the vertical vector at any of the 4 locations evaluated in this study (Figure 5).
4 Discussion
4.1 Main Findings
Collared stems generated a compressive strain at the medial proximal femur in the horizontal plane, which was significantly different from the tensile strain produced by single and double taper stems. At the lateral proximal femur in the horizontal plane, a compressive strain was produced by the double tapered stems, while the collared and single taper stems produced a tensile strain. There was no significant difference between stems at the anterior and posterior cortex in the horizontal vector and in any area in the vertical vector.
4.2 Study Purpose and Stem Design Overview
This study aimed to investigate the strain on the proximal femur during implantation of different types of primary cementless THA stems and its potential association with the risk of intraoperative periprosthetic femoral fracture (IOPFF). IOPFF during THA is a major contributing factor to reducing overall survivorship of uncemented stems and increasing overall morbidity and mortality [2, 3, 17, 18]. These findings provide insights into the biomechanical behavior and associated relative fracture risk of the three stem geometries examined: single (medial-to-lateral) taper, double taper, and collared stems.
4.3 Collard Stem Design and Medial Proximal Femoral Strain
In this biomechanical model of skeletally mature specimens with a range of bone densities, the impaction of a collared stem produced significantly less strain in the horizontal vector at the medial proximal femur compared to the strain produced from the impaction of single taper and double taper implants. This finding suggests that the design of the stem may play a critical role in modulating strain distribution in the proximal femur. The use of a collared stem may shield the medial proximal femur from circumferential strain as the collar of the device contacts the relatively strong calcar bone during implantation [19, 20]. Furthermore, no difference in strain was observed between the single taper and double taper stems at the medial cortex, challenging the often-remarked adage that the single (medial-to-lateral) taper stem may have a greater propensity for IOPFF than its metaphyseal filling counterpart. These findings are particularly relevant as the cortex of the medial proximal femur is a common location for intraoperative fracture, and increased strain in this region has been associated with a higher risk of IOPFF in previous studies [21, 22].
4.4 Evidence Supporting Collard Stems as Protective Against Periprosthetic Fracture
Indeed, other studies have touted that collared stems are protective against periprosthetic femoral fractures (PFF). In their paired cadaver biomechanical study, Lamb et al. concluded that the addition of a collar to an uncemented stem increases the torque required to cause periprosthetic femur fracture [19]. The authors postulate that the collar mitigates the rotation of the femoral stem with respect to the endosteal geometry, thereby decreasing the risk of fracture [20]. Similarly, Demey et al. demonstrated in their biomechanical model that collared uncemented stems have significantly greater immediate stability compared to collarless stems, enabling them to withstand greater forces before subsidence and fracture [23]. Furthermore, in a multicenter, retrospective study of 3433 primary cementless THAs performed from 2014 to 2021, Calkins et al. reported that compaction-collared stems had a significantly lower risk of postoperative PFF requiring operative treatment than single-taper and double-taper stems [24].
4.5 Implant Selection Based on Bone Density
For such reasons, some authors have advised selecting the appropriate implant design based on the bone density observed in preoperative radiographs. Carli et al. conducted a systematic review of 34 out of 596 initially identified articles and found that cementless implants, particularly single taper and double taper types, were linked to a significantly higher number of PFF when compared to anatomical, fully coated, and tapered/rounded stems [25]. The authors proposed reducing the utilization of single taper and double taper uncemented stems in older patients who have osteoporotic bone [25].
4.6 Double Taper Stem Design and Lateral Proximal Femur Strain
The present study, however, found that impaction of the double taper stem resulted in lower strain in the horizontal vector at the lateral proximal femur compared to the single taper and collared stems. Compared to the single taper and collared stems used in this study, the double taper stem has a relatively thicker profile in the anterior–posterior plane and fills a significant portion of the femoral metaphysis, giving rise to its “fit-and-fill” name. The metaphyseal-filling design with greater fixation in the meta-diaphysis may explain the decreased strain observed at the lateral proximal femur during impaction of the double taper stem compared to the single taper and collared designs.
4.7 Considerations for Cemented and Dual-Modular Stems
It has been suggested that surgeons should consider returning tocementing femoral stems as a solution to address the risk of IOPFF [26, 27]. However, it should be noted that simply transitioning to a cemented stem does not necessarily guarantee a low rate of periprosthetic fractures. Several studies have indicated that smooth, polished, tapered cemented femoral stems (which do not have a collar)actually have a relatively high incidence of fractures following the surgery [28, 29]. Despite these findings, cementation of femoral THA stems should remain within the contemporary arthroplasty surgeon's armamentarium for patients who have Dorr C bone, poor bone quality, and those with femoral neck fractures [26]. Lastly, dual-modular stems have largely fallen out of use during primary THA due to complications such as higher rates of fretting corrosion and fatigue failure at the modular neck-stem junction, associated adverse local tissue reactions, and need for revision surgery [30]. Despite these complications, dual-modular stems still have unique applicability in specific cases to address hip dysplasia and deformities and may be useful on a case-by-case basis [30].
4.7.1 Limitations and Strengths
The present study is not without its limitations. Our biomechanical model utilized cadaveric specimens, which may not fully replicate the in vivo conditions encountered during surgery. Therefore, caution should be exercised when extrapolating these findings to clinical practice. Future research using in vivo models or clinical data would provide a more robust understanding of the biomechanical factors contributing to IOPFF. In addition, although most manufacturers produce a single taper, double taper, and collared stem that is similar in design characteristics to those used in this study, the results of this study may not be transferable to other manufacturers' femoral stem designs. Furthermore, we used all uncemented monolithic stems in this study, limiting analysis of the possible differences in the strain produced on the proximal femur using modular stems and cemented implants.
This study has several notable strengths. We used a controlled biomechanical model of cadaveric femurs with a range of bone densities, which allowed for realistic simulation of clinical variability in patient bone quality. A standardized loading protocol ensured consistency across all stem implantations. Directly comparing three widely used stem designs highlights the biomechanical effects of stem geometry on the proximal femur. Strain was measured using standardized gauges placed at four critical regions of the proximal femur, and it was analyzed in both horizontal and vertical vectors to provide a comprehensive understanding of load distribution during implantation. Importantly, the study provides insight into intraoperative periprosthetic femoral fractures (IOPFF), a clinically significant complication in cementless THA, enhancing the practical relevance of the findings.
5 Conclusions
In this biomechanical evaluation of stem impaction strain, single (medial-to-lateral) and double(fit-and-fill) taper stem geometries were found to produce a tensile strain on the proximal femur medial cortex that differed significantly from the compressive strain generated by the collared design. No difference in strain was observed between the single and double taper stems at the medial proximal femur. Double taper stem designs exhibited a compressive strain at the lateral cortex of the proximal femur that differed significantly from the compressive strain generated by their single taper and collared counterparts. Since bone is more prone to fracturing under tensile loads, these findings may help arthroplasty surgeons optimize stem selection to mitigate the risk of IOPPF in patients undergoing THA.
Author Contributions
Barrett Bruno Torre: writing – original draft, writing – review and editing, conceptualization, methodology, investigation, formal analysis, supervision. Jordan Andre Bauer: writing – review and editing, conceptualization, formal analysis. Ian Wellington: writing – review and editing, methodology, investigation. Tannaz Sedghi: writing – review and editing, formal analysis. Dillon Neumann: writing – review and editing, investigation. Adam Lindsay: writing – review and editing, supervision. Olga Solovyova: writing – review and editing, supervision.
Ethics Statement
This study was conducted using human cadaveric specimens. All specimens were de-identified prior to use. In accordance with institutional policy and applicable national regulations, this study did not involve living human subjects and was therefore deemed by our Ethics Committee to be exempt from Institutional Review Board (IRB) oversight under Title 45, Code of Federal Regulations, Part 46. This research complied with all ethical standards regarding the respectful and appropriate use of human cadaveric material.
Conflicts of Interest
The authors declare no conflicts of interest.




