Introduction and An Analysis of Inter- and Intra-observer Validity to the Classification of Hoffa-Like Tibial Plateau Fractures
Zhongzheng Wang, Yanwei Wang, and Yuchuan Wang are Co-first author.
Abstract
Objective
The posterior coronal shearing fractures of the tibial plateau are rare and can be easily missed or ignored. Our team defined these fractures as Hoffa-like fracture of the tibial plateau and conducted a series of studies. The aim of this study is to introduce the characteristics of the Hoffa-like fracture of the tibial plateau, propose a new classification system and evaluate its validity.
Methods
Sixty-one patients with Hoffa-like fractures of the tibial plateau were treated in five trauma centers (I–III) from 2017 to 2020. A new classification system was developed based on the morphological fracture patterns in CT and radiographic of the first 30 cases. Ten cases of suspected tibial plateau Hoffa-like fractures were supplemented additionally to the 61 cases to increase the accuracy. CT and radiographic images of the 71 cases were reviewed independently by four reviewers on two separate occasions and classified according to the new classification system. Cohen's kappa coefficient (κ) was used to analyze the reliability on separate observers at the same time and to analyze the classification made by same observer at different times (intra-observer), which measures inter-observer and intra-observer agreements.
Results
Out of the 61 patients, 46 (75.4%) isolated coronal fractures involving the medial condyle of tibial plateaus and 53 (86.9%) combined with intercondylar spine fractures. The κ-values were calculated for the new classification system (mean κ = 0.74 inter-observer, mean κ = 0.79 intra-observer, indicating substantial agreement).
Conclusion
The novel classification lends insight into fracture morphology of the tibial plateau Hoffa-like fractures, has good inter- and intra-observer validity, and it aids in treatment.
Introduction
Isolated posterior coronal shearing fracture of the tibial plateau is an uncommon and unstable intra-articular fracture which extends through either the medial or lateral condyle.1 Like the distal femoral Hoffa fracture, the posterior coronal shearing fracture of the tibial plateau is also considered to be the result of high-speed and high-energy trauma. Some authors suggest that the direct impact of knee flexion is the injury mechanism, while others attribute the fracture to simultaneous vertical shear and torsion.2, 3 It is known that an isolated split fracture of the posteromedial condylar was first described in 1869 by Busch4 and noted that these injuries be considered as fracture-dislocations.5, 6 Based upon the basic concept of action and reaction force and the finding of Barei et al.7 the Hoffa-like fracture of the tibial plateau, isolated posterior shearing or splitting coronal fracture involving the medial/lateral or bicondylar, was proposed by our team.
Literature reports on the Hoffa-like fractures of the tibial plateau have been addressed very sporadically. Our clinical observations showed that such injuries mainly occurred in the medial condyle of the tibial plateau and rarely found in the lateral condyle because of fibula protection. This injury can be easily overlooked with conventional radiographs imaging, especially if nondisplaced or when present in association with an intercondylar proximal tibia.8 Ignoring this type of injury may cause distal displacement of the fracture fragments, leading to posterior subluxation, instability of the femoral-tibial articulation, stiffness, and arthritis of the knee.9
Various classification schemes are used to describe tibial plateau fractures, but few included this Hoffa-like fracture of the tibial plateau. The Schatzker,10 AO/OTA,11 Duparc and Ficat,12 Hohl and Luck,13 and three-column classifications14 of the tibial plateau fracture are the more popular classification methods, but none of them can accurately reflect this type of fracture. More recently the three-column system of Luo et al. has been developed, this tool is effective in describing any posterior fracture location but its' inability to distinguish between split and depression type fractures means the use of an accompanying classification is necessary.15 The Hoffa-like fracture of the tibial plateau, was classified as type I (simple posterior-medial plateau condyle fracture) by Moore,16 classified as a P-type (coronal split fractures of the posterior tibial fractures with a medial or lateral coronal split) by Khan et al.4 However, these two classifications did not describe the extent of fracture involvement and displacement, and had limited therapeutic significance. In addition, these classification systems were both developed using antero-posterior X-ray to define fracture patterns, so their ability to adequately describe all fracture patterns is somewhat limited.17 Therefore, the new naming and classification will facilitate scholars' memory and communication, and provide help for subsequent treatment.
We proposed a CT-based classification system for the Hoffa-like fracture of the tibial plateau. The purpose of this study is to introduce the novel classification for Hoffa-like fracture of the tibial plateau, develop corresponding treatment strategies and evaluate its inter- and intra-observer validity.
Materials and Methods
Patient Selection
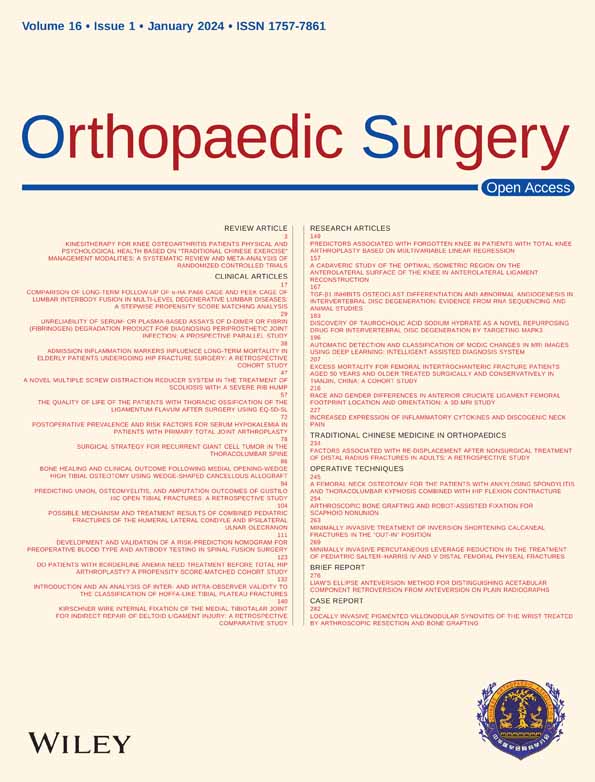
Using five maintained orthopedic databases at large level I to III trauma centers, we conducted a retrospective search for the radiograph and CT imaging data of 5560 patients with a diagnosis of the tibial plateau fracture between August 2017 and September 2020. All imaging data were collectively reviewed by three senior observers (two surgeons and one radiologist) with more than 10 years of experience in orthopedic trauma. Disagreement was resolved by consensus. Based upon the finding of Barei et al.,7 we defined the isolated coronal-plane split fracture in which the primary fracture line lying within −45° to 30 of posterior medial/lateral or bicondylar axis as a Hoffa-like fracture of the tibial plateau (Figure 1).
Finally, a total of 61 cases of Hoffa-like fractures of the tibial plateau were included in this study. Inclusion criteria were: (i) skeletally mature; (ii) patients were diagnosed isolated Hoffa-like fracture of the tibial plateau; (iii) closed fractures presenting within 2 weeks; (iv) completed preoperative radiographic (anteroposterior and lateral views) and CT images; and (v) time of postoperative follow-up of at least 1 year. Exclusion criteria: (i) fracture associated with ipsilateral sagittal-plan plateau fracture; (ii) same leg distal femur fracture or comminuted fracture; and (iii) open injuries of the knee were excluded.
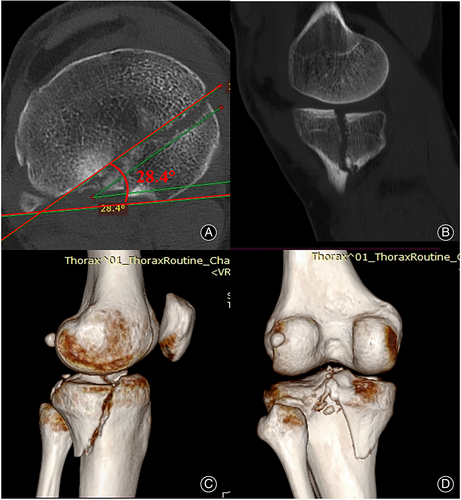
Description of the Classification
The development of the new classification is based on our initial pilot study details and abundant clinical experience obtained at the five trauma centers. In our experience, the lack of identifying of the size and displacement of the posterior fracture fragments will not achieve reduction and good alignment of the articular, which may lead to poor prognosis. In the CT scans and plain radiographs of the first 30 cases, the Hoffa-like fractures of the tibial plateau are classified into three types and nine subtypes based on position of the primary fracture line involving articular surface and the degree of fracture displacement. The primary fracture line involving the sagittal plane <1/4 of the posterior tibial plateau condyle (medial/lateral) were designated Type I. Primary fracture line involving the sagittal plane ≥1/4 and ≤1/2 of the posterior tibial plateau condyle (medial/lateral) were named Type II. Type III were those primary fracture line involving the sagittal plane >1/2 of the posterior tibial plateau condyle (medial/lateral). Those not having displacement being Subtype A, those having minimal articular step (<2 mm) being Subtype B and those having obvious articular step (≥2 mm) named Subtype C (Figure 2).
Management and Follow-up
All 61 patients diagnosed with Hoffa-like fracture of the tibial plateau received symptomatic treatment at our five trauma centers. Among them, we found that the common treatment strategies included conservative treatment (immobilization of the affected limb, plaster or brace fixation), external fixation, Kirschner or screw fixation, plates and screws fixation.18 Anterolateral approach, lateral approach, medial approach, posteromedial approach and bilateral (medial and lateral) approach were the popular surgical approaches.1, 14 Demographic characteristics, mechanism of injury, combined fractures, treatment strategies, the time of follow-up and fracture healing were recorded. At the final follow-up, the Hospital for Special Surgery (HSS) score was used to evaluate the function outcome of the knee and the visual analogue scale (VAS) score (0, no pain; 10, maximal imaginable pain) was used to assess the pain of the knee.19-21
Assessment of Inter- and Intra-observer Validity
Four additional observers (one trauma-trained resident [A], two senior orthopedic surgeons [B and D], and one radiologist specializing in musculoskeletal radiology [C]) were recruited to classify the images of the tibial plateau Hoffa-like fractures, all of whom were not in charge of patient selection. Before reviewing the images, the four reviewers were trained in using the new classification and showed examples of each type. There were ten cases of suspected tibial plateau Hoffa-like fractures, inclusion criteria were imaging diagnosis of simple depressed tibial plateau fractures, split combined with depressed tibial plateau fractures, sagittal split fractures of the tibial plateau, and comminuted tibial fractures, were supplemented additionally to the 61 cases to increase the sample size, break the inherent thinking of observers and increase the accuracy of the study. Then, the four reviewers independently reviewed the 71 CT and radiographic images on two occasions (8 weeks apart). The 71 cases were randomly arranged and marked with numbers. The observers' first choices were not available for the second reviewing, and they received no feedback after the first reviewing. The cases need to be shuffled before being reviewed a second time by the same reviewer. When recording the classification results, the nine categories were marked from 1 to 9 successively, and the cases that could not be included were marked with “NO.” Non-participants recorded the classification results of each time.
Statistical Analysis
All statistic data were performed using IBM Statistical Package for Social Sciences (SPSS) version 26.0 (IBM, Armonk, NY, USA). Cohen's kappa coefficient (κ) was used to analyze the reliability on separate observers on same time and to analyze the of the classification made by same observer in different time (intra-observer), which measures inter-observer and intra-observer agreements.22 The level of κ values was interpreted according to the guidelines of Landis and Koch.23 κ (0–0.20) as slight agreement, 0.21–0.40 as fair agreement, 0.41–0.60 as moderate, 0.61–0.80 as substantial agreement, and 0.81–1 as perfect agreement. Continuous data is expressed as the mean and range. Categorical variables are presented as numbers and percentages.
Results
Participants and Classification
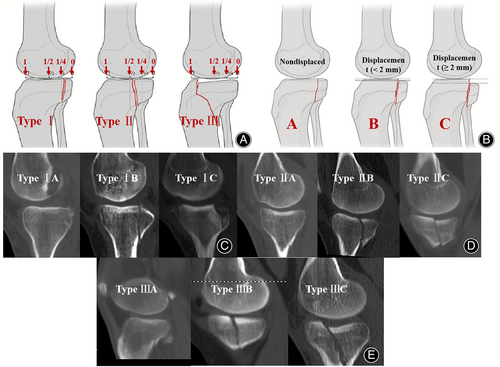
A total of 61 patients (41 males and 20 females, mean age was 44.5 years, range 26–74) with Hoffa-like fractures of the tibial plateau out of the 5560 tibial plateau fractures were included in the retrospective study. The tibial plateau Hoffa-like fractures accounted for about 1.1% (61/5560) of the tibial fractures. Among the 61 cases, 32 (52.5%) were caused by road traffic accidents, 19 (31.1%) caused by falling from height. Eleven cases of the tibial plateau Hoffa-like fracture combined with fibula head fracture, which mainly occurred in the lateral condyle of tibia. Forty-six cases (46/61, 75.4%) of primary fracture line involved the medial condyle of the tibial plateau. Fifty-three (53/61, 86.9%) cases of the tibial plateau Hoffa-like fracture combined with intercondylar spine fracture, which mainly occurred in the medial and dual condyle of the tibia (Figure 3A,B). Fifty-seven cases (57/61, 93.4%) whose primary fracture line entered along the medial condyle of the tibial plateau and gradually extended to the posterior condyle or the lateral condyle. There were only four cases (4/61, 6.6%) whose primary fracture line entered along the lateral condyle and gradually extended to the posterior condyle (Figure 3C). Among the 61 cases, 21 received conservative treatment, eight received Kirschner wire or screws fixation, and 33 received plate and screw fixation. The authors found that the novel classification scheme generally correlated with treatment strategies and developed corresponding treatment plans accordingly. The fracture types and recommended treatments are summarized in Table 1. Also, the 61 patients completed at least 1 year of follow-up (mean 27.5 months, range 12.0–48.0 months). The mean fracture healing time was 4.9 months (range 3–9 months). At the final follow-up, the mean HSS score was 83.4 (range 57.0–98.0) and the mean VAS score was 1.8 (range 0–5.0) (Table 2).
| Types | Description | Recommended treatment | Case (n, %) |
|---|---|---|---|
| I | Primary fracture line involved the coronal plane <1/4 of the posterior tibial plateau condyle (medial/lateral) | 6, (9.8%) | |
| Subtype IA | The articular step –nondisplaced | Conservative treatment | 1, (16.7%) |
| Subtype IB | The articular step–minimally displaced (<2 mm) | Conservative treatment | 1, (16.7%) |
| Subtype IC | The articular step–obviously displaced (≥2 mm) | Plate and screws | 4, (66.6%) |
| II | Primary fracture line involved the coronal plane the ≥1/4 and ≤1/2 of the posterior tibial plateau condyle (medial/lateral) | 25, (41.0%) | |
| Subtype IIA | The articular step–nondisplaced | Kirschner wire/screw/plate | 11, (44.0%) |
| Subtype IIB | The articular step–minimally displaced (<2 mm) | Kirschner wire/screw/plate | 6, (24.0%) |
| Subtype IIC | The articular step–obviously displaced (≥2 mm) | Plate and screws | 8, (32.0%) |
| III | Primary fracture line involved the coronal plane >1/2 of the posterior tibial plateau condyle (medial/lateral) | 30, (49.2%) | |
| Subtype IIIA | The articular step–nondisplaced | Plate and screws | 9, (30.0%) |
| Subtype IIIB | The articular step–minimally displaced (<2 mm) | Plate and screws | 4, (13.3%) |
| Subtype IIIC | The articular step–obviously displaced (≥2 mm) | Plate and screws | 17, (56.7) |
- Note: See Figure 1.
| Characteristic | Hoffa-like fracture of the tibial plateau, n = 61 | Characteristic | Hoffa-like fracture of the tibial plateau, n = 61 |
|---|---|---|---|
| Age, years | 44.5 (26–74) | Intercondylar spine Fracture, yes | 53 (86.9%) |
| Sex, male | 41 (67.2%) | Follow-up time, months | 27.5 (12.0–48.0) |
| BMI, Kg/m2 | 25.4 (18.8–40.09) | Time to bone union, months | 4.9 (3.0–8.0) |
| Mechanism of Injury | Fracture line | ||
| Vehicle | 32 (52.5%) | Medial condyle | 46 (75.4%) |
| Falling | 19 (31.1%) | Lateral condyle | 4 (6.6%) |
| Others | 10 (16.4%) | Dual condyle | 11 (18.0%) |
| Affected side, right | 24 (39.3%) | HSS points* | 83.4 (57.0–98.0) |
| Fibula head fracture, yes | 11 (18%) | VAS score* | 1.8 (0.0–5.0) |
- Notes: Data presented as mean (range), or n patient prevalence.
- Abbreviation: BMI, body mass index.
- * Represents the score were evaluated at the final follow-up.
Inter-observer Reliability
The mean κ value for inter-observer reliability between different observers using the new classification twice was 0.74 (range 0.61–0.87), indicating “substantial agreement.” The lowest mean κ-value for inter-observer reliability was 0.65 (range 0.63–0.67) occurred among the resident and radiologist (A and D). The two senior orthopedic surgeons showed highest agreement level with mean κ value of 0.82 (range 0.77–0.87) (Table 3).
| Observers | Inter-observer (1st time) | Inter-observer (2nd time) | Mean | ||
|---|---|---|---|---|---|
| k Statistic | Agreement | k Statistic | Agreement | ||
| A-B | 0.77 | Substantial | 0.75 | Substantial | 0.76 |
| A-C | 0.63 | Substantial | 0.67 | Substantial | 0.65 |
| A-D | 0.75 | Substantial | 0.79 | Perfect | 0.77 |
| B-C | 0.71 | Substantial | 0.84 | Perfect | 0.78 |
| B-D | 0.87 | Perfect | 0.77 | Substantial | 0.82 |
| C-D | 0.61 | Substantial | 0.75 | Substantial | 0.68 |
| Mean | 0.72 | Substantial | 0.76 | Substantial | 0.74 |
- Note: k-value: (0–0.20) as slight agreement, 0.21–0.40 as fair agreement, 0.41–0.60 as moderate, 0.61–0.80 as substantial agreement, and 0.81–1 as perfect agreement.18
Intra-observer Reproducibility
Using the new CT-based classification, the mean κ-value for intra-observer reproducibility was 0.79 (range 0.64–0.93), again indicating “substantial agreement” (Table 4).
| Observers | Intra-observer | |
|---|---|---|
| k Statistic | Agreement | |
| A | 0.93 | Perfect |
| B | 0.82 | Perfect |
| C | 0.64 | Substantial |
| D | 0.75 | Substantial |
| Mean | 0.79 | Substantial |
Discussion
In this study, a new CT-based classification system for the tibial plateau Hoffa-like fracture was proposed according to the location of primary fracture line and the degree of fracture fragment displacement. And specific treatment strategies for each type were recommended. Additionally, Kappa (κ) statistics showed that the new classification has a high agreement level of inter- and intra-observer.
Characteristics of Hoffa-like Tibial plateau fractures
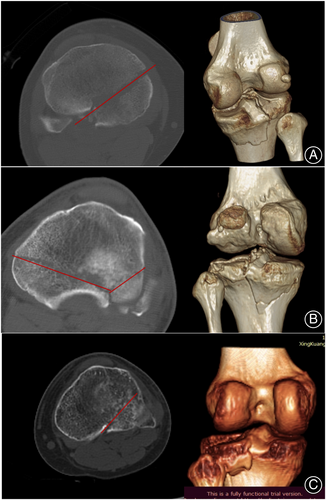
In recent years, the posterior coronal shearing fractures of the tibial plateau, facing the distal femoral, have been gradually recognized by orthopedic surgeons.24 The isolated posterior coronal shearing fracture of the tibial plateau, known as Hoffa-like fracture of the tibial plateau, is a rare injury and appears confusing on initial radiographs.2, 24, 25 However, with the widespread use of CT scans, we found that this type of fracture has been underappreciated previously.1 On the axial plan of CT scans, the Hoffa-like fracture line of the tibial plateau usually extends posterolateral from medial side of the medial condyle, or extends posteromedial from lateral side of the lateral condyle. Although occasionally bicondylar, the Hoffa-like fractures of the tibial plateau are commonly unicondylar and usually originate from the medial condyle.18, 26
Injury Mechanism of Hoffa-like Tibial plateau fractures
The mechanism of injury implied that Hoffa-like fracture of the tibial plateau was mainly caused by the direct impact with the knee in a flexed position, and followed by the vertical shear and twisting forces with the knee in a hyperextension position. In our recent study of lower extremity specimens, the mechanisms of injury in two scenarios (falling from height and motor vehicle crash) were simulated and this type of fracture was successfully reproduced in 6/10 specimens. In both settings, the axial or anter-posterior force from the femoral condyle was concentrated on the posterior half of the tibial plateau, resulting in an isolate shearing fracture with no depression.27, 28 In addition, we found that the clinical outcomes of previously treated patients with Hoffa-like fractures of the tibial plateau were not satisfactory. The mean knee HSS function score was 83.4 and the mean VAS pain score was 1.8 at our follow-up of at least 1 year. Therefore, orthopedic surgeons should pay more attention to these injuries.
Treatment Strategies of Hoffa-Like Tibial plateau fractures
As we all know, an ideal fracture classification system should not only be easy to understand and remember, but also to guide treatment selection, indicate prognoses, and show low validity among users.29 The most common tools utilized today have been developed based on coronal plane radiographs alone and fail to recognize those characteristics witnessed using CT scans in conjunction with three-dimensional reconstructions.15, 17 On the basis of fully understanding the anatomical structure and fracture characteristics of the isolated posterior coronal shearing tibial plateau fractures, the authors proposed a simple yet comprehensive CT classification. The new classification can accurately describe the location of primary fracture line(s) along with the degree of articular surface involvement and the degree of fracture fragment displacement. Furthermore, we have formulated specific recommended treatment planning for each subtype of fracture, which may improve the development of fixation concepts relative to the Hoffa-like fractures of the tibial plateau. For fractures of type IA and IB, conservative treatment can be selected. For fractures of two subtypes of IIA and IIB, screw fixation is recommended, and plates and screws can also be used if necessary. For all type C, type IIIA and IIIB fractures, plates and screws are recommended for firm fixation. It should be noted that the fracture lines of type IIIA and IIIB are long oblique, and the fracture piece is prone to sliding relative to the diaphysis, which has a high risk of secondary displacement. Therefore, plate and screw fixation must be carried out to prevent postoperative secondary reduction loss, which has been confirmed in previous studies.18, 26, 30
Validity to the Classification of Hoffa-Like Tibial Plateau Fractures
Kappa (κ) statistics are the common method used to calculate changes of inter- and intra-observer variations.3 In general, the reliability of simpler classification systems is higher, such as the three-column classification which is usually high, but the disadvantage is that it provides less information about fracture patterns and morphology.31 According to our statistical results, we found that the new classification system had high reliability and repeatability. More importantly, our new classification is based on fracture line progression and collapse degree. The mean κ value for inter-observer reliability was 0.72 (range 0.61–0.87) at the first viewing and 0.76 (range 0.67–0.84) at the second viewing, indicating “substantial agreement.” And with the increase of proficiency in the new classification system, the consistency between observers tends to be stable. Besides, the mean κ-value for intra-observer reproducibility was 0.79 (range 0.64–0.93), indicating “substantial agreement.” Therefore, we believe that the new classification system will have wide application prospects.
Strengths and Limitations
To the best of our knowledge, this was first time the novel Hoffa-like tibial plateau fracture classification system and to verify the inter- and intra-observer validity has been presented. Moreover, 10 suspected cases were included in the analysis process to improve the accuracy of the study to a certain extent. Despite the relative strengths of this study, certain limitations must be acknowledged. First, this research was retrospective, which was susceptible to various inducement factors, leading to data bias. Second, the small sample size and short-term follow-up were insufficient to assess postoperative traumatic arthritis. Third, the recommended treatment strategies were based on our previous clinical results rather than true prognosis outcomes.
Prospects of Clinical Application
In the future, prospective, multi centre randomized controlled, and long-term follow-up studies using our proposed CT-based classification system and treatment planning will help to further strengthen the reliability of classification and obtain better clinical results. We believe that the novel classification system will be an important prerequisite for future preoperative planning of Hoffa-like tibial plateau fractures.
Conclusions
Hoffa-like fractures of the tibial plateau are uncommon, challenging intra-articular fractures that demand careful diagnosis and specific treatment planning. This novel CT-based classification shows higher inter- and intra-observer consistency and aids in treatment. Therefore, the new classification for Hoffa-like fractures of the tibial plateau is effective and may have a wide application prospect.
Acknowledgments
I would like to thank all co-authors for their contributions to data collection and collation, writing, and language formatting and proofreading.
Funding Information
This study was supported by the National Natural Science Foundation of China (grant number: 82102551) and Non-profit Central Research Institute Fund of the Chinese Academy of Medical Sciences (grant number: 2019PT320001).
Conflict of Interest Statement
The authors declare that there is no conflict of interest regarding the publication of this paper.
Ethics Statement
This study was registered as a ClinicalTrials.gov PRS (NCT04807062) and approved by the Clinical Trial Ethics Committee of our hospital. These methods were carried out in according with the guidelines of Helsinki Declaration. All data were retrospectively collected and analyzed. The need for informed consent was waived by the Ethics Committee of Hebei Medical University (No. 2021-024-1).
Author Contributions
Zhongzheng Wang, Yanwei Wang and Yuchuan Wang: collecting and analyzing the data, interpreting data, writing and editing the manuscript. Pengyu Ye and Yanbin Zhu: analyzing and interpreting the data, revising the manuscript. Wei Chen and Zhiyong Hou: designing the study, revising the manuscript. Zhiyong Hou and Yingze Zhang: designing and supervising the study, revising the final manuscript.
Open Research
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.