Arthroscopic Bone Grafting and Robot-assisted Fixation for Scaphoid Nonunion
Abstract
Objectives
Scaphoid nonunion remains a challenging problem to manage with no general consensus on its treatment recommendations. We propose a novel minimally invasive (MIS) technique of arthroscopic bone grafting (ABG) with robot-assisted fixation for the treatment of scaphoid nonunions.
Methods
Patients with radiographically proven scaphoid nonunion treated by this novel surgical technique were included. Following arthroscopic debridement and iliac crest bone grafting, the scaphoid was fixed percutaneously using either multiple Kirschner (K)-wires or a headless compression screw using a robotic navigation system.
Results
Six male patients with an average age of 29.2 years were enrolled. Four patients had scaphoid waist fractures, and the other two were proximal pole fractures. During wrist arthroscopy, punctate bleeding of the proximal scaphoid fragment was observed in four out of the six patients. Half of the patients were fixed using a headless compression screw and the other half using multiple K-wires. All the guidewires were placed with a single-attempt using the robotic navigation system. Postoperatively, all the scaphoid fractures had complete radiographic union by 16 weeks. At a mean follow-up of 18.3 months, there were significant improvements in wrist range of motion, grip strength, and patient-rated outcomes. No intraoperative or early postoperative complications were encountered in any of our patients.
Conclusion
Arthroscopic bone grafting with robot-assisted fixation is a feasible and promising therapeutic option for scaphoid nonunions, regardless of the vascularity of the proximal pole fragment. This novel technique allows for anatomic restoration of the scaphoid alignment and accurate, targeted placement of implants into the scaphoid nonunion site within a single-attempt using a robotic navigation system.
Introduction
The scaphoid is the most commonly fractured carpal bone, with a 2–7% incidence rate of all fractures.1, 2 Approximately 10–15% of acute scaphoid fractures eventually progress to fracture nonunion due to the fracture instability,3 tenuous blood supply,4 high rates of missed diagnosis,5 and delayed presentation.3, 5, 6 Nonunions can occur even if there was timely intervention with cast immobilization.5, 7, 8
There have been various surgical techniques reported in the literature,9-14 but the consensus for optimal treatment recommendation for scaphoid nonunions remains debatable. Non-vascularized bone grafts with internal fixation are reported to have an 88% union rate for scaphoid nonunion,15 however open surgery theoretically does additional damage to important structures such as the joint capsule, ligaments, and potentially threatens the already tenuous blood supply.16, 17 Arthroscopic bone grafting (ABG) allows for a minimally invasive (MIS) surgical approach and also achieves satisfactory clinical outcomes for scaphoid nonunion.18, 19 Another issue to highlight is that accurate fixation of scaphoid fractures can be technically demanding under fluoroscopy,20 and suboptimal placement of implants can occur even for experienced hand surgeons. Repeated attempts of guidewire insertion weaken the structural integrity of the scaphoid, and the resultant bone loss coupled with suboptimal implant placement may lead to further complications.21 Excessive radiation exposure from repeated fluoroscopy during the traditional freehand implant placement for scaphoid fracture is also an issue of concern for both the surgeons and the patients.22-24 With the advent of robotic navigation systems in hand surgery, the overall accuracy, efficacy, and safety of percutaneous fixation of scaphoid fractures have greatly improved.9, 25-28
As such, we propose a novel MIS surgical technique of ABG combined with robot-assisted fixation for the treatment of scaphoid non-unions. With the use of three-dimensional (3D) intraoperative real-time image navigation, percutaneous scaphoid fixation becomes precise and easy to perform.
This study comprises six male patients with scaphoid nonunions who were treated by this novel MIS surgical technique. The goals of this study are to: (i) describe the surgical workflow; and (ii) report the preliminary clinical and radiographic outcomes in our case series.
Methods
This was a retrospective case series that was approved by the local hospital ethics committee (K2022-111-01). Informed consent was obtained from all the patients prior to the start of the study.
The inclusion criteria include: (i) patients with radiographically proven scaphoid nonunions (X-ray or CT); (ii) more than 6 months from injury to initial surgery; and (iii) minimum of at least a 1-year follow-up.
The exclusion criteria include: (i) degenerative wrist arthritis, for example, scaphoid nonunion advanced collapse (SNAC) wrist; (ii) injuries to the contralateral upper limb; and (iii) incomplete or loss to follow-up data.
Surgical Technique
Anesthesia and Position
All patients were positioned supine and given a brachial plexus block as regional anesthesia. An arm tourniquet was placed over the injured limb and the limb was hung using a wrist traction tower.
Arthroscopic Bone Grafting
The 3–4 portal was created and used to evaluate the wrist ligament and status of the joint cartilage. Arthroscopic debridement of wrist synovitis was performed using an arthroscopic shaver. The midcarpal radial (MCR) and midcarpal ulnar (MCU) portals were created to evaluate the cartilage of the midcarpal region as well as the scaphoid nonunion site. A probe was then introduced via the MCR portal to examine the stability of the nonunion site with the MCU portal used for direct visualization. A headless compression screw (Mini Acutrak, Acumed, Hillsboro, OR, USA) was used to percutaneously fix fracture fragments that were large enough,19 and for fracture fragments deemed too small for screw placement, three 1.1 mm Kirschner (K)-wires were inserted instead.19 The nonunion site was meticulously debrided using an arthroscopic shaver, arthroscopic burr, and curette through midcarpal portals. Vascularity of the proximal pole of the scaphoid was determined after debridement by checking for punctate bleeding (Figure 1A). One or two K-wires were drilled into the distal scaphoid via the scaphoid tubercle as joysticks without crossing the nonunion site. Under arthroscopic guidance, reduction of two nonunion fragments was achieved by manipulating the joysticks and an added probe. Once satisfactory alignment was achieved, the pre-inserted guidewires were then drilled into the proximal scaphoid fragment through the fracture line for temporary fixation.27, 29, 30

A 2-cm incision was made over the contralateral iliac crest for bone graft harvest. The amount of autologous cancellous bone graft required to be harvested was approximately three to five times that of the nonunion defect size. The bone graft was then morselized using a rongeur and delivered via a 4.0 mm cannula to the nonunion site through the MCR portal (Figure 1B). Under direct visualization using the MCU portal, the bone graft was packed firmly into the fracture site using a depressor (Figure 1C).
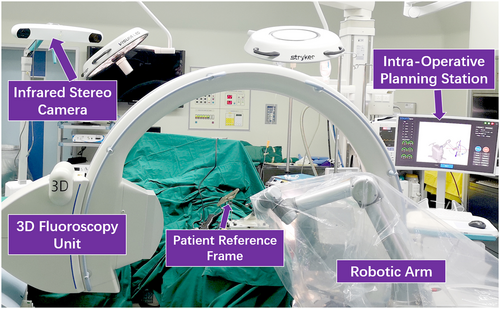
Robot-assisted Percutaneous Fixation
After bone graft insertion, the wrist traction tower was removed and the injured wrist was then fully extended and firmly fixed onto a radiolucent, reusable wrist positioning jig.25 The jig has a patient reference frame attached and the 3D-fluoroscopy unit (ISO-C3D, Siemens, Erlangen, Germany) was used for intraoperative 3D image capturing. The TiRobot (TINAVI Medical Technologies, Beijing, China), a commercially available robotic navigation system (Figure 2), was utilized for guidewire placement and implant trajectory planning.25 The surgeons can adjust the position, angle, and length of the screw or guidewire placement in the coronal, sagittal, and axial planes in the robotic software workstation (Figure 3D, see also Figure 5D). A wire aiming guide that was part of the robotic arm was automatically introduced through the gripper of the robotic arm to the planned implant insertion site. For scaphoid nonunion fragments that were large enough, a 1.1 mm K-wire was first introduced into the central axis of the scaphoid under the constraint of the wire aiming guide (Figure 3E), and a cannulated drill was used to drill over the K-wire before insertion of the headless compression screw (Figure 3F). For scaphoid nonunion fragments that were too small to accommodate screw placement, three 1.0-mm K-wires were inserted using the robotic arm after the ideal positions were determined in the navigation system (Figure 5E, F). Satisfactory reduction of the scaphoid fragments and position of the implant placement was confirmed by fluoroscopy. If K-wires were used, they were cut and buried beneath the skin for later removal. The wrist traction tower was set up again for a final check of the scaphoid nonunion site, ensuring that the bone graft remains tightly packed.
Postoperative Management
Postoperatively, all patients were immobilized with a thermoplastic scaphoid splint that included the interphalangeal joint of the thumb. Supervised rehabilitation with an occupational therapist was commenced at week 8 postoperatively.
Follow-up Assessment
All the patients were followed up at regular intervals with serial radiographic imaging to confirm bony union. Standard scaphoid X-rays were taken at 4-week intervals to monitor the progress of graft incorporation and fracture union19 and eventual bony union was confirmed by CT imaging. At the final follow-up, the bilateral wrists' range of motion (ROM) and grip strength were measured. The visual analogue scale (VAS) pain score, the Mayo wrist score (MWS), the quick disabilities of arm, shoulder, and hand score (QuickDASH), and the patient-rated wrist evaluation (PRWE) were also evaluated.
Statistical Analysis
SPSS v. 25.0 software (IBM, Armonk, NY, USA) was used for statistical analysis. The paired data were presented as medians and interquartile range and assessed with the Wilcoxon signed rank test. Two-tailed tests were used throughout and significance was defined at p value <0.05.
Results
From January 2021 to June 2022, six male patients with an average age of 27.2 (range: 16–47) years were enrolled. The basic information of the six male patients is presented in Table 1. Four out of six patients were scaphoid waist nonunions, and the remaining two were proximal pole scaphoid nonunions. Only one patient was a smoker. None of the patients had humpback deformity or other significant scaphoid malalignment, which were evaluated by preoperative CT imaging.
| Case | Age | Occupation | Side affected | Mechanism of injury | Smoker | Scaphoid nonunion site | Prior visit and intervention | Injury to surgery interval/ (month) | Type of implant | Operation duration/(minute) | Union time/(week) | Follow-up interval/(month) | Return-to-work |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 21 | Worker | R, Dominant | Motor vehicle accident | No | Waist | Delayed presentation, no treatment | 6 | Screw | 120 | 12 | 29 | Same job |
| 2* | 47 | Clerk | R, Dominant | Fall from heights | Yes | Waist | Timely visit and missed diagnosis, surgery | 312 | Screw | 180 | 16 | 20 | Same job |
| 3 | 19 | Athlete | R, Dominant | Sports | No | Waist | Timely visit and missed diagnosis, no treatment | 7 | Screw | 165 | 12 | 19 | Retraining |
| 4 | 32 | Engineer | R, Dominant | Sports | No | Proximal pole | Delayed presentation, no treatment | 24 | K-wires (3) | 180 | 15 | 17 | Same job |
| 5 | 28 | Designer | L, Non-dominant | Sports | No | Waist | Timely visit and correct diagnosis, cast immobilization | 6 | K-wires (3) | 255 | 12 | 13 | Same job |
| 6 | 16 | Student | R, Dominant | Sports | No | Proximal pole | Timely visit and missed diagnosis, no treatment | 8 | K-wires (3) | 105 | 12 | 12 | Same job |
- * This was a redo case of scaphoid nonunion as the initial surgery of arthroscopic bone graft and percutaneous screw fixation at another local hospital was performed close to a year ago.
Punctate bleeding of the proximal scaphoid fragment was observed in four out of six patients during intraoperative wrist arthroscopic visualization. Contralateral iliac crest cancellous autograft was harvested for all six of our patients. All the patients underwent single-attempt guidewire insertion using the 3D navigation system and half of them were fixed using a headless compression screw and the other half using multiple K-wires. The mean operative time was 167.5 (range: 105–255) minutes. All the scaphoids united at a mean follow-up of 13 (range: 12–16) weeks, as confirmed by CT imaging.
The functional results are presented in Table 2. At a mean follow-up of 18.3 months, there were significant improvements in grip strength, wrist ROM, VAS, QuickDASH, MWS, and PRWE scores. Five patients returned to their original occupations and one patient who was a professional basketball player was undergoing retraining. No intraoperative or early postoperative complications were encountered.
| Variables | Pre-operative | Last FU | z-value | p-value* |
|---|---|---|---|---|
| Grip strength (%)† | 77.5 (65–86) | 95 (84–100) | −2.214 | 0.027 |
| Wrist ROM arc (%)† | 75 (50–85) | 92.5 (80–100) | −2.041 | 0.041 |
| VAS (point) | 2.5 (2–5) | 0.5 (0–2) | −2.214 | 0.027 |
| MWS (point) | 65 (55–76) | 80 (74–100) | −2.060 | 0.039 |
| QuickDASH (point) | 21.6 (12.5–30.1) | 4.6 (1.7–10.2) | −2.207 | 0.027 |
| PRWE (point) | 21.5 (17.3–28.9) | 9.5 (4.5–15.6) | −2.207 | 0.027 |
- Note: Wrist range of motion (ROM) includes flexion-extension and radial-ulnar deviation. Grip strength and wrist range of motion are presented as percentage of the contralateral wrist. All the data were presented as medians and interquartile range.
- * p-values were calculated using the Wilcoxon signed rank test.
- † Presented as percentage of the contralateral wrist.
- Abbreviations: FU, Follow-up; MWS, Mayo Wrist Score; PRWE, Patient-Rated Wrist Evaluation; QuickDASH, the Quick Disabilities of the Arm, Shoulder, and Hand score; VAS, visual analogue scale.
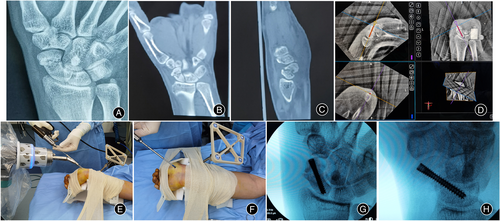
Illustration of Case 1
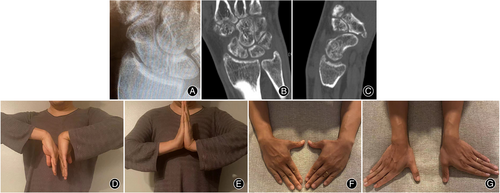
A 21-year-old male patient sustained a scaphoid waist fracture after falling off his bike. He did not seek medical attention until 6 months post injury due to persistent pain. Preoperative X-ray and CT images revealed a scaphoid waist nonunion (Figure 3A–C). He was treated with ABG and TiRobot-assisted fixation using a percutaneous headless compression screw (Figure 3D–F). Intraoperative fluoroscopy confirmed satisfactory screw placement (Figure 3G,H). X-ray and CT images taken 12 weeks after surgery showed union of the fracture site (Figure 4A–C). The final follow-up assessment at 29 months showed excellent functional recovery (Figure 4D–G).

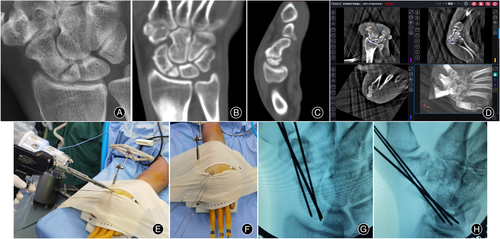
Illustration of Case 4
A 32-year-old male patient sustained a wrist injury while playing soccer. He had a delayed presentation a year after the injury and was diagnosed then with proximal pole scaphoid nonunion. However, he took another year to decide to proceed with surgery. Preoperative X-ray and CT imaging at 2 years post injury re-confirmed the proximal pole scaphoid nonunion (Figure 5A–C). He was treated with ABG and TiRobot-assisted percutaneous fixation using three K-wires (Figure 5D–F). Intraoperative fluoroscopy confirmed satisfactory positioning of the K-wires (Figure 5G, H), which were removed 2 months after surgery. X-rays and CT image performed 15 weeks after surgery confirmed fracture union (Figure 6A–C). At his final follow-up assessment at 17 months, he demonstrated excellent and painless functional recovery of his injured wrist (Figure 6D–G).
Discussion
Current Therapeutic Insights in Scaphoid Nonunion
The treatment of scaphoid nonunions remains a challenging and controversial problem. Delayed treatment of this condition leads to progressive degenerative wrist osteoarthritis,31 otherwise known as SNAC wrist. Sequelae to developing SNAC wrist can exist even with timely surgical intervention.15 Patients may sustain debilitating wrist pain and stiffness without valid therapeutic strategies.32
There is a lack of high-quality studies in the current literature on the merits of arthroscopic management of scaphoid nonunions. However, it can be extrapolated that this MIS procedure is surgically less traumatic, has good arthroscopic magnification for better carpal visualization, and allows for early rehabilitation postoperatively.16, 18 A comparative study of patients managed with arthroscopic or open bone graft and internal fixation revealed high union rate in both techniques (96.4% and 97.1% respectively).11 Although the open technique restored carpal alignment more satisfactory based on imaging, both groups remained comparable at the minimum 2-year follow-up.
Another method of treating scaphoid nonunions is using vascularized bone grafting, but this procedure has a steep learning curve with high technical demands with a potential for donor site morbidities.18 These difficulties have prompted surgeons to re-explore the option of non-vascularized grafting and wrist arthroscopy in treating scaphoid nonunions instead.12, 13, 16, 18, 19, 32, 33 A recent systematic review suggested that ABG can be equally efficacious in achieving union compared with vascularized bone grafting in treating scaphoid nonunion.15 In a retrospective study by Ramamurthy et al.,33 the union rate for scaphoid nonunions treated by open non-vascularized grafting and fixation was reported at 71%. Wong and Ho18 reported an overall 90.3% union rate in arthroscopic management of scaphoid nonunion, which was comparable to Wu et al.19 who demonstrated a 100% union rate using arthroscopic bone grafting and fixation in 20 patients with proximal pole scaphoid nonunion, with satisfactory functional recovery at a mean follow-up of 31 months. Our current case series also showed satisfactory clinical outcomes with a 100% scaphoid union rate using ABG and robot-assisted fixation, regardless of the implant used.
Preliminary Outcome
In this study, we used a novel MIS technique of ABG with robot-assisted percutaneous fixation for the treatment of either waist or proximal pole scaphoid nonunion in six patients. Normal alignment of the scaphoids was restored in all patients after the packing of the non-vascularized iliac crest bone graft into the nonunion site under arthroscopic guidance. A robot-assisted single-attempt guidewire insertion was performed in all patients. Our short-term follow-up demonstrated satisfactory functional recovery with a 100% union rate.
In comparison to previous studies, the mean surgical time of this dual ABG and robot-assisted fixation is 167.5 (range: 105–255) minutes, which is comparable to the ABG and conventional freehand percutaneous fixation technique of an average of 118 min in Wu et al.,19 182.5 min in Lee et al.,34 and 213 min in the Wong and Ho18 studies, respectively. A lengthy set-up time (about 20–30 min) is required for the robotic system.25, 28 There is a learning curve to the correct positioning of the wrist, jig, trackers, and the alignment of the robot navigation system to effectively receive the signals. A designated robotic surgery operating room with trained medical staff will also help in reducing the setting up time.
The Correlation of Avascular Necrosis with Rate of Bony Union
Some studies have demonstrated the tenuous blood supply of the proximal pole of scaphoid using micro-computed tomography imaging.4, 17 At arthroscopy, punctate bleeding of the proximal scaphoid fragment was not seen in two out of the six patients, but both these patients had complete bony healing within 16 weeks after surgery. Wong and Ho18 defined the lack of punctate bleeding of the proximal scaphoid fragment as avascular necrosis but they were still able to achieve 81.8% union rate in such patients. Similarly, this finding was also supported by other reports in the literature,19, 35-37 and presence of scaphoid proximal pole avascularity did not appear to correlate with fracture healing potential.35, 38
Surgical Tips and Tricks of this MIS Technique
The accurate placement of K-wires into the scaphoid bone under conventional fluoroscopy control can be challenging, even for experienced hand surgeons. The robot-assisted technique provides a precise and quick method for optimal implant placement in both nondisplaced and displaced scaphoid fractures within a single-attempt.25, 27 Of note, the relevant training to the surgeons on how to use the 3D navigation system is necessary.
One of our male patients (case 2) was a redo case as the scaphoid remained ununited after the initial surgery of ABG and percutaneous screw fixation at another local hospital. Specific to this patient, a chronic heavy smoking history may be one of the reasons the fracture remained ununited.37 We repeated the arthroscopic bone grafting and used the 3D navigation system to place the screw in the central axis of the scaphoid. Coupled with smoking cessation therapy, the patient went on to achieve bony union of the scaphoid at 16 weeks postoperatively.
Economic Evaluation of the Robotic Surgery
The TiRobot system is more costly as compared with traditional percutaneous scaphoid surgery but apart from being able to use this robotic system in scaphoid surgeries, the TiRobot system can also be used in other sub-specialties like spine surgeries. Just in the first half of 2023, the TINAVA company's annual report for the TiRobot system surpassed 10,000 cases.39 We believe that the further popularization of robots will help to spread the upfront and running costs in larger specialist units through joint purchasing and usage agreements.25
Limitations of this Study
There are some limitations to our study. This is a technical feasibility report with a relatively small sample size of only six patients enrolled. Although the short-term follow-up results have been promising, a longer surveillance to track their long-term functional recovery is necessary. More comparative studies between arthroscopic bone grafting using the conventional freehand technique versus robot-assisted fixation are required to better assess the reliability of this novel technique and whether it indeed leads to better clinical outcomes in the long run for the treatment of scaphoid nonunions.
Conclusion
Arthroscopic bone grafting and robot-assisted percutaneous fixation for scaphoid nonunions is a feasible and promising surgical method with satisfactory short-term clinical results, regardless of the vascularity of the proximal pole fragment. This novel technique allows for anatomic restoration of the scaphoid alignment and accurate, targeted placement of implants into the scaphoid nonunion site within a single-attempt using a robotic navigation system.
Author Contributions
All authors had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Conceptualization, B.L.; methodology, Z.Y., R.Q.R.L., and J.Z.; investigation, Z.Y. and R.Q.R.L.; formal analysis, Z.Y. and R.Q.R.L.; resources, S.C. and B.L.; writing—original draft, Z.Y.; Writing—review and editing, Z.Y., R.Q.R.L., J.Z., S.L.C., and B.L.; visualization, B.L.; supervision, S.L.C. and B.L.; funding acquisition, B.L.
Acknowledgments
We would like to thank Professor Pak-Cheong Ho of Prince of Wales Hospital, Hong Kong, for inspiring us to adopt wrist arthroscopy in the treatment of scaphoid pathology. We would also like to thank Mrs. Jie Shen of Beijing Jishuitan Hospital, China for her assistance in this research.
Funding Information
This study was supported by Beijing Municipal Science and Technology Project (code: Z201100005520094). Beijing Natural Science Foundation-Joint funds of Haidian Original innovation Project (code: L202030). National Natural Science Foundation of China (code: 82272581). Yunnan Provincial Science and Technology Talents and Platform Project (code: 202105AF150050).
Conflict of Interest
The authors declare that they have no potential conflict of interest.
Ethics statement
Informed consent was obtained from all participants included in this study. This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Beijing Jishuitan Hospital (No. K2022-111-00).