Robot-Assisted Minimally Invasive Transforaminal Lumbar Interbody Fusion in the Treatment of Lumbar Spondylolisthesis
Disclosure: This work was supported by the Youth Science Foundation of the National Natural Science Foundation of China (81201433), The National High Technology Research and Development Program of China (2015AA043201), the National Key Development Program (2016YFC0105800), and the Beijing Natural Science Foundation (Z170001).
Abstract
Objective
To compare the clinical efficacy between robot-assisted minimally invasive transforaminal lumbar interbody fusion (robot-assisted MIS-TLIF) and traditional open TLIF surgery in the treatment of lumbar spondylolisthesis.
Methods
According to the inclusion and exclusion criteria, 48 cases with lumbar spondylolisthesis who received surgical treatment from June 2016 to December 2017 in the spinal surgery department of Beijing Jishuitan Hospital were analyzed in this study, including 23 patients who received robot-assisted MIS-TLIF and 25 patients who received traditional open TLIF surgery. The two groups were compared in terms of pedicle screw accuracy evaluated by Gertzbein-Robbins classification on postoperative computed tomography (CT), operation time, blood loss, postoperative drainage, hospitalization, time to independent ambulation, low back pain evaluated by visual analog scale (VAS), lumbar function evaluated by Oswestry Disability Index (ODI), paraspinal muscles atrophy on magnetic resonance imaging (MRI), and complications.
Results
Postoperative CT showed that the rate of Grade A screws in the robot-assisted MIS-TLIF group was significantly more than that in the open surgery group (χ2 = 4.698, P = 0.025). Compared with the open surgery group, the robot-assisted MIS-TLIF group had significantly less intraoperative blood loss, less postoperative drainage, shorter hospitalization, shorter time to independent ambulation, and lower VAS at 3 days post-operation (P < 0.05). However, the duration of surgery was longer. The VAS of the robot-assisted MIS-TLIF group decreased from 6.9 ± 1.8 at pre-operation to 2.1 ± 0.8 at post-operation, 1.8 ± 0.7 at 6-month follow-up and 1.6 ± 0.5 at 2-year follow-up. The VAS of the open surgery group decreased from 6.5 ± 1.7 at pre-operation to 3.7 ± 2.1 at post-operation, 2.1 ± 0.6 at 6-month follow-up and 1.9 ± 0.5 at 2-year follow-up. The ODI of the robot-assisted MIS-TLIF group decreased from 57.8% ± 8.9% at pre-operation to 18.6% ± 4.7% at post-operation, 15.7% ± 3.9% at 6-month follow-up and 14.6% ± 3.7% at 2-year follow-up. The ODI of the open surgery group decreased from 56.9% ± 8.8% at pre-operation to 20.8% ± 5.1% at post-operation, 17.3% ± 4.2% at 6-month follow-up and 16.5% ± 3.8% at 2-year follow-up. Paraspinal muscle cross-sectional area in 2-year follow-up in patients of the open surgery group decreased significantly compared to patients of robotic-assisted MIS-TLIF group (P = 0.016).
Conclusion
In the treatment of lumbar spondylolisthesis, robot-assisted MIS-TLIF may lead to more precise pedicle screw placement, less intraoperative blood loss, less postoperative drainage, less postoperative pain, quicker recovery, and less paraspinal muscle atrophy than traditional open surgery.
Introduction
Spondylolisthesis is defined as a disorder that causes the slip of one vertebral body over the one below. It includes degenerative spondylolisthesis and isthmic spondylolisthesis. Lumbar spondylolisthesis occur in 4%–6% of the general population1, 2. It commonly occurs at the fourth and fifth lumbar vertebrae and accounts for more than 95% of the total cases of lumbar spondylolisthesis. Lumbar spondylolisthesis is a major cause of spinal canal stenosis and is related to low back pain and leg pain. Most people with lumbar spondylolisthesis do not have any symptoms, only approximately 10% of these people have clinical symptoms that require treatment. However, once symptoms occur, more than 50% of the patients complain of considerable pain and dysfunction and, in severe cases, cauda equina syndrome3. Studies have demonstrated that once patients fail a 6-week trial of standardized nonsurgical treatment that includes physical therapy, medications, and spinal injections, surgical treatment is superior4.
Several spinal fusion techniques have been used in the surgical treatment of lumbar spondylolisthesis, their purpose is to decompress the neural elements and stabilize the spinal segment through arthrodesis with pedicular instrumentation. transforaminal lumbar interbody fusion (TLIF) is associated with shorter operation time, requires less neural retraction, decreases the complications of neurological injury, and has less adjacent segment degeneration compared with posterior lumbar interbody fusion (PLIF)5, 6. Extreme lateral interbody fusion (XLIF) enabled foramen decompression and increased central canal diameter but with a risk of interbody implant impaction, correction loss, and recurrent root pain. Furthermore, TLIF is less technically demanding than anterior lumbar interbody fusion (ALIF), while also avoiding various risks to abdominal organ, vessel, nerve, and retrograde ejaculation. However, traditional open TLIF surgery still results in fairly extensive damage to the muscle, spinous process, and even sometimes the facet joints. Moreover, the postoperative healing of the surgical wound in the back muscles could have negative effects on its short-term and long-term clinical efficacy7. Therefore, MIS-TLIF has been widely applied with the advantages of less blood loss, quicker recovery, and lower incidence of adjacent segment degeneration.
In a meta-analysis which compared the accuracy of robot-assisted and free-hand pedicle screws insertion, the results showed that the robot-assisted technique is more accurate than the free-hand technique after analyzing the incidence of “perfect” and “clinically acceptable” pedicle screw insertions8. Several orthopaedic robots have been applied in spinal operation, including TianJi Robot, SpineAssist, Renaissance, Mazor, and da Vinci Robotic System. The TianJi Robot is an orthopaedic surgical robot developed in China with completely independent intellectual property, and it has been applied in the surgery of all spinal segments9, 10. A high level of accuracy for pedicle screw insertion and a reliable, safe process were showed in the clinical application of the TianJi Robot11, 12. In our current study, we used the TianJi Robot system to assist the pedicle screw insertion in the MIS-TLIF procedure and help to identify the decompressed site.
Progress has been made in minimally invasive surgical instruments, surgical navigation systems, and surgical robots, while the surgical techniques of physicians have also improved. Therefore, it is now possible to perform precise robot-assisted MIS-TLIF in the treatment of lumbar spondylolisthesis. In this study, we compared the clinical outcomes of robot-assisted MIS-TLIF and traditional open surgery in the treatment of patients with lumbar spondylolisthesis. The purpose of our preliminary study included the following: (i) whether robot-assisted MIS-TLIF is feasible and safe in the treatment of patients with lumbar spondylolisthesis; (ii) compared to traditional open surgery, does robot-assisted MIS-TLIF result in a more stable fixation, less surgical trauma, and early postoperative recovery in the treatment of patients with lumbar spondylolisthesis; (iii) what kinds of complications are associated with robot-assisted MIS-TLIF and traditional open surgery in the treatment of patients with lumbar spondylolisthesis.
Materials and Methods
Study Popualtion
Inclusion and Exclusion Criteria
Inclusion criteria followed the participant, intervention, comparison, outcome (PICO) model: (i) patients with single-segment, Meyerding Grade I or II lumbar spondylolisthesis, persistent lower back pain for more than 6 months, VAS > 5, systemic conservative management was ineffective; (ii) robot-assisted minimally invasive pedicle insertion and transforaminal lumbar interbody fusion; (iii) freehand fluoroscopy assisted pedicle screw insertion and traditional open transforaminal lumbar interbody fusion; (iv) accuracy of screw placement, operative time, blood loss, postoperative drainage, length of hospitalization, time to independent ambulation, lower back pain evaluated using visual analog scale (VAS), lumbar function evaluated using the Oswestry disability index (ODI), paraspinal muscle atrophy and complications.
Exclusion criteria were: (i) patients who had received previous lumbar spinal surgery; (ii) patients with lumbar spinal infection, tumor, and adjacent lumbar segmental instability; (iii) patients with scoliosis.
The percentage of lumbar vertebral slippage was calculated based on Taillard index13, that is, percentage of slippage = relative forward displacement distance of upper vertebral body on the lower vertebral body/ length of upper vertebral body × 100%. A score of 0%–25% was considered as Meyerding Grade I, and 25%–50% was considered as Meyerding Grade II.
Groups of Patients
In total, 48 patients with spondylolisthesis were included in this study, they were randomly divided into two groups. All patients were chosen consecutively according to random number table: when one patient corresponded to an odd number, the patient would be in robot-assisted MIS-TLIF group, and when one patient corresponded to an even number, the patient would be in open surgery group. Robot-assisted MIS-TLIF group included 23 cases: four male and 19 females, aged 35–71 years, mean age 51.3 years. Three smokers and six cases presented with osteoporosis. Thirteen cases presented with slippage at segment L4-5 and 10 cases at L5S1. Seven cases accompanied with spondylolysis. Five cases complained of back pain and 18 cases complained of back pain accompanied with lower limb pain and numbness. Based on the Meyerding classification, 12 cases showed Grade I slippage and 11 cases showed Grade II slippage.
Open surgery group included 25 cases: six males and 19 females, aged 39–72 years, mean age 54.1 years. Six smokers and seven cases presented with osteoporosis. Fifteen cases presented with slippage at segment L4-5 and 10 cases at L5S1. Nine cases were accompanied with spondylolysis. Seven cases complained of back pain and 18 cases complained of back pain accompanied with lower limb pain and numbness. Based on the Meyerding classification, 14 cases showed Grade I slippage and 11 cases showed Grade II slippage.
The patients received the operation from June 2016 to December 2017 in the spinal surgery department of Beijing Jishuitan Hospital. The two groups of patients were comparable in terms of gender, age, the percentage of smokers, the percentage of osteoporosis, the percentage of spondylolysis, segment of slippage, severity of slippage, preoperative VAS, and preoperative Oswestry disability index (ODI). The differences were not statistically significant (P > 0.05, Tables 1 and 2).
| Groups | No. of cases | Gender | Age (years, x̅ ± s) | Smoker | Osteoporosis | Spondylolysis | Slippage segment | Slippage severity | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | L4-5 | L5S1 | Grade I | Grade II | ||||||
| Robot-assisted MIS-TILF group | 23 | 4 | 19 | 51.3 ± 9.8 | 3 | 6 | 7 | 13 | 10 | 12 | 11 |
| Open surgery group | 25 | 6 | 19 | 54.1 ± 10.2 | 6 | 7 | 9 | 15 | 10 | 14 | 11 |
| Test statistics | — | 0.317 | 0.593 | 0.944 | 0.022 | 0.167 | 0.060 | 0.071 | |||
| P value | — | 0.419 | 0.561 | 0.276 | 0.570 | 0.460 | 0.519 | 0.509 | |||
| Characteristic | Robot-assisted MIS-TILF | Open TLIF | P-value |
|---|---|---|---|
| Duration of surgery (min) | 135.1 ± 11.2 | 102.2 ± 7.1 | 0.002 |
| Intraoperative blood loss (mL) | 173.6 ± 17.9 | 332.1 ± 23.5 | 0.005 |
| Postoperative drainage (mL) | 97.5 ± 13.8 | 261.3 ± 19.8 | 0.000 |
| Hospitalization (day) | 7.3 ± 1.8 | 10.0 ± 1.6 | 0.018 |
| Time to independent ambulation (day) | 1.5 ± 0.8 | 2.9 ± 1.3 | 0.006 |
| Visual analog scale (VAS) of low back pain | |||
| Preoperative | 6.9 ± 1.8 | 6.5 ± 1.7 | 0.687 |
| Postoperative | 2.1 ± 0.8 | 3.7 ± 2.1 | 0.004 |
| 6-month follow-up | 1.8 ± 0.7 | 2.1 ± 0.6 | 0.762 |
| 2-year follow-up | 1.6 ± 0.5 | 1.9 ± 0.5 | 0.861 |
| Oswestry Disability Index (ODI) | |||
| Preoperative | 57.8% ± 8.9% | 56.9% ± 8.8% | 0.916 |
| Postoperative | 18.6% ± 4.7% | 20.8% ± 5.1% | 0.825 |
| 6-month follow-up | 15.7% ± 3.9% | 17.3% ± 4.2% | 0.765 |
| 2-year follow-up | 14.6% ± 3.7% | 16.5% ± 3.8% | 0.718 |
| Accurate number/total screw number | 87/92 | 85/100 | 0.025 |
| Intraoperative revision, no. of screws | 0 | 5 | |
Surgical Equipment
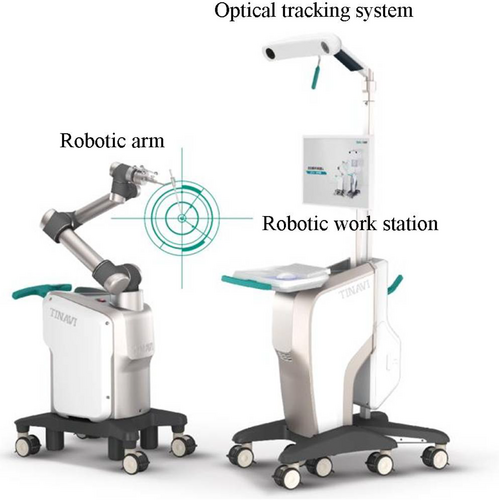
The TianJi Robot (Beijing Tinavi Medical Technology, Beijing, China) is composed of a robotic surgical planning and operation station and an infrared positioning camera which work as an optical tracking system and a 6 degree-of-freedom (DOF) robotic arm (Fig. 1). The computer of the surgical planning station can use intraoperative digital imaging data to perform three-dimensional (3D) reconstruction. The surgeon determines the entry point, direction, length, and diameter of the pedicle screw and the decompression site to perform the corresponding preoperative planning and surgical simulation. Space mapping between the patient position and 6-DOF robotic arm is performed using the optical tracking system. This enables the unification of the coordinate systems between the medical imaging space and the robotic arm. During the operation, the robotic work station can be used to control the 6-DOF robotic arm to perform intraoperative positioning and operations.
Surgical Procedure
Robot-assisted Surgery
Anesthesia and position. After general anesthesia the patient was placed in a prone position. Fluoroscopy was used to determine the spinous process of the vertebra above the slipped vertebra.
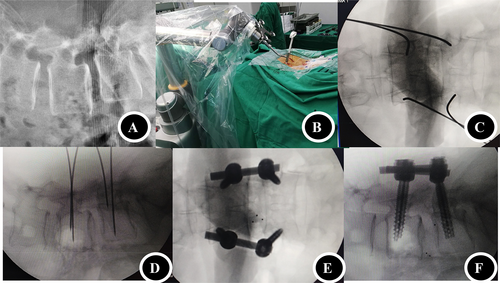
Approach and exposure guided by the robot. the patient tracer was fixed to the spinous process of the vertebra above the slipped vertebra. A C-arm (ARCADIS Orbic 3D C-arm, Simens) automatically performed a continuous rotation of 190° to acquire a set of digital images which were transferred to the work station of TianJi Robot. The robot surgical planning and operation station was then used to confirm the entry point, direction, diameter, and length of the pedicle screws. Then, corresponding transverse incisions were made for intermuscular blunt separation.
Pedicle screw insertion and decompression guided by the robot. The robot was used to determine the entry pathway of the pedicle screw and guide pins were placed. The robot was also used to locate the position of the intervertebral disc which caused symptoms, and the multifidus gap was separated until the facet joint. Then, a stepwise expansion sleeve was placed along the guide pins, followed by MAST Quadrant retractor. The robot surgical planning and operation station was then used to determine the decompression site. Part of the lamina, ligament flava, inferior articular process, and the superior articular process were removed. The nerve root canal and nerve roots were examined.
Interbody fusion and closure. The intervertebral disc was removed and the endplate was prepared. The bone graft was placed in the intervertebral space, and an intervertebral fusion cage was inserted. Pedicle screws were then inserted along the guide pins, connecting rods were installed, and spinal alignment was restored (Fig. 2). The drainage tube was placed, and the incision was sutured layer by layer.
Traditional Open Surgery
Anesthesia and position. After general anesthesia, the patient was placed in the prone position. Fluoroscopy was used to determine the pedicle of the slipped vertebra and below the slipped vertebra.
Approach and exposure. A posterior midline incision was made. A high frequency electric knife was used to dissect the paraspinal muscles along the spinous process. Blunt separation of the paraspinal muscles was performed. After bipolar electrocoagulation for hemostasis, the muscle was cut to expose the lateral edge of the facet joint.
Pedicle screw insertion and decompression. Routes for pedicle screws were prepared by analyzing the anatomic mark and the mark pins were placed. After confirmation by fluoroscopy, the pedicle screws were placed. The lower half of the lamina, unilateral inferior articular process of the slipped vertebra, and the corresponding superior articular process of the lower vertebra were removed. The nerve root canal and nerve roots were examined.
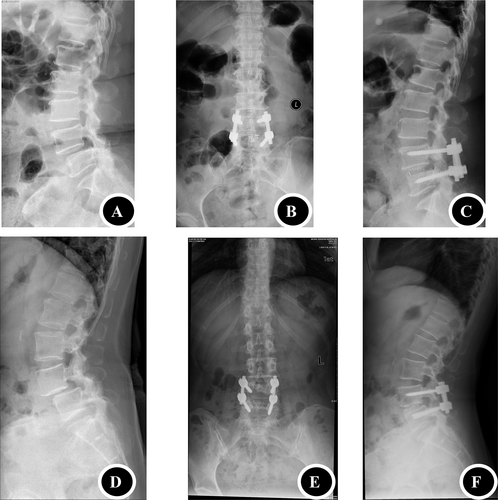
Interbody fusion and closure. The intervertebral disc was removed and the endplate was prepared. The bone graft was placed in the intervertebral space, and an intervertebral fusion cage was inserted. Connecting rod was installed and spinal alignment was restored (Fig. 3). The drainage tube was placed, and the incision was sutured layer by layer.
Outcome Measures
Accuracy of Pedicle Screw Placement
Accuracy of pedicle screw placement was assessed on postoperative thin-cut CT scan by a blinded, independent radiologist based on Gertzbein–Robbins classification: Grade A: perfect intrapedicular localization without breach of the cortical layer of the pedicle; Grade B, <2-mm pedicle breach; Grade C, <4-mm pedicle breach; Grade D, <6-mm pedicle breach; and Grade E, a ≥ 6-mm deviation from the pedicle cortex14. Graded A pedicle screws were considered to be perfect intrapedicular localization, while graded B–E pedicle screws were considered to be poor trajectory15.
All data were recorded and evaluated by a blinded, independent clinician.
Duration of Surgery
Duration of surgery was defined as the time to perform all procedures after anesthesia, including positioning the patient, exposing the operative area, pedicle screw insertion, decompression, interbody fusion, wound suture, and changing the patient's position.
Intraoperative Blood Loss
Intraoperative blood loss was defined as the volume of blood lost during surgery, which was measured by the sum of the blood in the suction bottle and the amount of blood in the gauze.
Postoperative Drainage
Postoperative drainage was defined as the volume of blood lost after surgery, which was measured by the volume of the fluid in the drainage bottle.
Length of Hospitalization
Length of hospitalization was defined as the days the patient stayed in the hospital, which was calculated from the date the patient was admitted to the hospital to the date of discharge.
Time to Independent Ambulation
Time to independent ambulation was defined as the date from the day after surgery to date when the patient could walk independently by themselves.
Lower Back Pain
VAS was used to evaluate lower back pain. Using a VAS ruler, the score was determined by the patient's mark on the 10-cm line, a range of scores from 0 to 10, which extend from “no pain” to the most severe pain. A higher score means greater pain intensity.
Lumbar Function
Lumbar function was evaluated using the ODI. The ODI includes 10 sections: pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, and traveling. Each section comprises six statements that are scored from 0 to 5. Intervening statements are scored according to rank. If more than one box is marked in each section, the highest score is used. If all 10 sections are completed, the score is calculated as follows: total scored out of total possible score × 100. If one section is missed (or not applicable), the score is calculated: (total score / (5 × number of questions answered)) × 100%. Here, 0%–20% is considered mild dysfunction, 21%–40% is considered moderate dysfunction, 41%–60% is considered severe dysfunction, 61%–80% is considered disability, and 81%–100% considers patient as either long-term bedridden or exaggerating the impact of pain on their life.
Paraspinal Muscles Atrophy
Cross-sectional area of paraspinal muscles measured on preoperative and 2-year follow-up axial MRI image was used to evaluate the paraspinal muscles atrophy.
Evaluation of Intraoperative and Postoperative Complication
The intraoperative and postoperative complications in follow-up were recorded. The intraoperative complications include screw misplacement, dural damage, nerve root damage, etc. Postoperative complications include neurological compromise, such as radiating pain, numbness, decreased muscle strength, infection, cerebrospinal fluid leakage, screw loosening, etc.
Statistical Analysis
SPSS 19.0 (Chicago, IL, USA) was employed for statistical analysis. Continuous variables including age, duration of surgery, intraoperative blood loss, postoperative drainage, length of hospitalization, VAS, and ODI, and are reported as mean ± standard deviation. Between-group comparisons were made with the independent-sample t-test. Categorical variables including number of patients, and number of screws are reported as a frequency or percentage. Between-group comparisons were made with chi-square test. Differences were considered statistically significant when P < 0.05.
Ethical Approval
This study was approved by the ethics committee of the Beijing Jishuitan Hospital (Beijing Jishuitan Hospital ethical approval No.: 20150504), and all patients provided written informed consent.
Results
Baseline Characteristics of Study Paticipants
This study included 48 patients (robot-assisted MIS-TILF group: 23 patients; open surgery group: 25 patients; male: 23 patients; female: 25 patients). Mean age of the patients was 52.7 (range, 35 to 72 years), difference of age of the two groups was not significant (P > 0.05, Table 1). There were three smokers in robot-assisted MIS-TILF group and six in open surgery group, difference of the two groups was not significant (P > 0.05, Table 1). There were six patients with osteoporosis in robot-assisted MIS-TILF group and seven in open surgery group, difference of the two groups was not significant (P > 0.05, Table 1). There were seven patients with spondylolysis in robot-assisted MIS-TILF group and nine in open surgery group, difference of the two groups was not significant (P > 0.05, Table 1). There were 13 L4/5 segments and 10 L5/S1 segments in robot-assisted MIS-TILF group and 13 L4/5 segments and 10 L5/S1 segments in open surgery group, difference of the two groups was not significant (P > 0.05, Table 1). There were 12 grade I and 11 Grade II cases of spondylolisthesis in robot-assisted MIS-TILF group and 14 grade I and 11 Grade II cases of spondylolisthesis in open surgery group, difference of the two groups was not significant (P > 0.05, Table 1).
Accuracy of Screw Placement
Among the 92 pedicle screws in the robot-assisted MIS-TLIF group, 87 were Grade A and five were Grade B. Among the 100 pedicle screws in the open surgery group, 85 were Grade A and 15 were Grade B. Both groups did not have Grade C, D, or E pedicle screws. Grade A screws in the robot-assisted MIS-TLIF group was significantly more than that of the open surgery group (χ2 = 4.698, P = 0.025, Table 2).
Duration of Surgery
Duration of surgery was significantly longer for patients in robot-assisted MIS-TILF group (135.1 ± 11.2 min) compared to open surgery group (102.2 ± 7.1 min) (P < 0.05, Table 2).
Intraoperative Blood Loss
Intraoperative blood loss was significantly less for patients in robot-assisted MIS-TILF group (173.6 ± 17.9 mL) compared to open surgery group (332.1 ± 23.5 mL) (P < 0.05, Table 2).
Postoperative Drainage
Postoperative drainage was significantly less for patients in robot-assisted MIS-TILF group (97.5 ± 13.8 mL) compared to open surgery group (261.3 ± 19.8 ml) (P < 0.05, Table 2).
Length of Hospitalization
Length of hospitalization was significantly less for patients in robot-assisted MIS-TILF group (7.3 ± 1.8 days) compared to open surgery group (10.0 ± 1.6 days) (P < 0.05, Table 2).
Time to Independent Ambulation
Time to independent ambulation was significantly less for patients in robot-assisted MIS-TILF group (1.5 ± 0.8 days) compared to open surgery group (2.9 ± 1.3 days) (P < 0.05, Table 2).
Lower Back Pain
The preoperative VAS score for lower back pain was not significantly different for robot-assisted MIS-TLIF group (6.9 ± 1.8) compared to open surgery group (6.5 ± 1.7). The VAS of the robot-assisted MIS-TLIF group decreased from 6.9 ± 1.8 at pre-operation to 2.1 ± 0.8 at post-operation, 1.8 ± 0.7 at 6-month follow-up and 1.6 ± 0.5 at 2-year follow-up. The VAS of the open surgery group decreased from 6.5 ± 1.7 at pre-operation to 3.7 ± 2.1 at post-operation, 2.1 ± 0.6 at 6-month follow-up and 1.9 ± 0.5 at 2-year follow-up. Postoperative VAS of robot-assisted MIS-TLIF group was lower than that of the open surgery group in all follow-up stages but only the difference of 3-day post-operation was significant (P < 0.05, Table 2). The postoperative VAS of both groups at all stages were significantly smaller compared to the preoperative VAS (P < 0.05).
Lumbar Function
The ODI of the robot-assisted MIS-TLIF group decreased from 57.8% ± 8.9% at pre-operation to 18.6% ± 4.7% at post-operation, 15.7% ± 3.9% at 6-month follow-up and 14.6% ± 3.7% at 2-year follow-up. The ODI of the open surgery group decreased from 56.9% ± 8.8% at pre-operation to 20.8% ± 5.1% at post-operation, 17.3% ± 4.2% at 6-month follow-up and 16.5% ± 3.8% at 2-year follow-up. Compared to open surgery group, ODI of robot-assisted MIS-TLIF group was not significantly different for all stages (P > 0.05, Table 2). The postoperative ODI of both groups at all postoperative stages were significantly smaller compared to that of the preoperative ODI (P < 0.05).
Paraspinal Muscles Atrophy
Paraspinal muscle cross-sectional area at 2-year follow-up decreased by an average of 14.5% (SD = 8.9%; range, −28.1% to −2.7%) in patients of the open surgery group and decreased by an average of 3.9% (SD = 8.1%; range, −13.8% to +11.2%) in patients of MIS-TLIF group (P = 0.016).
Complications
During surgery, no pedicle screws in robot-assisted MIS-TLIF group required intraoperative revision. While in the open surgery group, five pedicle screws required intraoperative revision (Table 2). Both groups did not show dural damage, nerve root damage, decreased muscle strength, infection, cerebrospinal fluid leakage. One patient in the robot-assisted MIS-TLIF group and one patient in the open surgery group presented with transient numbness in the lateral foot dorsum. After neurotrophic treatment, the numbness disappeared at the postoperative 6-month follow-up. One patient in the open surgery group (whose pedicle screw was revised during operation) complained of low back pain at 6-month follow-up and the X-ray film show the upper pedicle screw loosening, accompanied by the development of spondylolishthesis. She received another revision operation using bone cement intensification of the pedicle screw route.
Discussion
The advantages of using a robot for surgery include fatigue resistance and high precision. Therefore, the application of robot-assisted surgery has been gradually increasing in general surgery, neurosurgery, cardiac surgery, urology, and orthopaedics, and has yielded good clinical efficacy16, 17. Current applications in orthopaedics mainly involve the TianJi Robot, SpineAssist, Mazor, Israeli Renaissance, and US da Vinci Robotic System. The system used in this study was the TianJi Robot System, which can conduct surgery on all spinal segments, pelvis, and limb fractures. This robot system is able to use intraoperative 3D imaging to achieve accurate positioning, conduct precise placement of pedicle screws and facilitate the accurate decompression of the spinal canal. It has already been successfully applied in challenging upper cervical spine surgery9, 10.
Robot Assistance Makes Operations Less Invasive
During the exposure process in traditional open TLIF surgery, the paraspinal muscles are separated from the spinal processes and lamina. The lateral part of facet joint is also exposed. Therefore, retractor was required to pull strongly the paraspinal muscles laterally during screw placement and decompression, which can result in more severe muscular damage and greater postoperative pain. The substitution of paraspinal muscles by scar tissue can be observed in the patients who receive a second operation. In contrast, minimally invasive distractor was used in MIS-TLIF to separate and expose the muscular space. Therefore, in the treatment of lumbar spondylolisthesis, it will result in less intraoperative blood loss, less postoperative pain, and regain more quickly. In conventional MIS-TLIF, the exposure of anatomical markers was also required to ensure accurate pedicle screw placement and decompression. Therefore, it can still cause a certain extent of dissection and damage to the muscle and ligament. Robot-assisted MIS-TLIF uses robots for accurate positioning based on intraoperative imaging data. It does not require the exposure of anatomical markers to determine the entry point, direction, and length of pedicle screws and it alleviates the damage to the muscle. Furthermore, the path of the longest and thickest pedicle screw can be determined, which will ensure maximum pullout strength of the pedicle screws. This will prevent the pedicle screws from loosening or dislocating while restoring the alignment of vertebral slippage.
Multifidus mainly participates in back flexion, rotation of the spine and maintaining lumbar lordosis. They are important for maintaining dynamic spinal stability, and their function cannot be replaced by other muscles after damage. Robot-assisted MIS-TLIF alleviates the interference with spinal stability by protecting the multifidus and other paraspinal tissues. It can reduce the incidence of adjacent segment degeneration, and also create the conditions for early postoperative activity. Postoperative MRI indicated that the patients of the robot-assisted MIS-TLIF group did not show significant paraspinal muscle atrophy compared to pre-operation, whereas the open surgery group showed significant muscle atrophy. After surgery, patients of the robot-assisted MIS-TLIF group were ambulatory significantly earlier than that of the open surgery group, which may have reduced the incidence of complications related to bed rest. The postoperative pain and ODI in both groups showed improvements compared to preoperative values. The VAS of the robot-assisted MIS-TLIF group on the third day after surgery was significantly lower than that of the open surgery group. These suggest the benefits of minimal surgical trauma, mild pain, and rapid recovery of robot-assisted MIS-TLIF. Due to the limited exposure and field of vision in MIS-TLIF, one of its disadvantages is insufficient decompression. A proportion of nerve compression might not be detected during surgery, which could lead to insufficient decompression. The robot system can display the real-time positions of 3D bone structure, and help the surgeon to locate the specific positions that need decompression. If necessary, another intraoperative scan can be performed before wound closure to determine whether the decompression was sufficient and whether the position of pedicle screws was accurate.
Robot-Assisted Precise Pedicle Screw Placement
Consistent with other research results, the rate of pedicle screw misplacement of the robot-assisted group is lower than that of free-hand group18-20. Furthermore, robot-assisted systems can ensure precise pedicle screw once for all, which can prevent the reduction of pullout strength caused by changing of pedicle screw routes. This is one of the main reasons for the development of robot systems in spinal surgery. The percentage of Grade A pedicle screw placement using the TianJi Robot system was 94.6%, which was significantly higher than the 85% using free-hand placement in the open surgery group. This is also higher than the 89.3% reported in the literature using the SpineAssist robot-assisted system21 and 87.8% using the O–arm navigation22. While using the O–arm navigation or other kinds of navigation to prepare the pedicle screw route, we must push the probe, and this may cause the image shifting and lead to an error in the route. During operation in the prone position under general anesthesia, respiratory movement may cause motion of the vertebral body, particularly in the lower thoracic and lumbar spine23. These displacements may cause inaccurate robot operations. The TianJi Robot can perform real-time measurements of the error. When large errors are detected, the ventilator can be disconnected for a short period of time to avoid respiratory movements. The ventilator is restarted after errors decrease and the robot finishes its work accurately.
Learning Curve of the Robot-Assisted MIS-TLIF
Relevant research findings have shown that after the da Vinci robot system was used to perform 10 consecutive surgeries, the surgical team showed better coordination. As the number of surgical cases increased, shorter time was needed to create the operating space and to establish access using the robotic arm24. Our experience indicates that in the treatment of lumbar spondylolisthesis using robot-assisted minimally invasive TLIF, 10 cases of surgery was sufficient to complete the learning curve. After that, the time required for robot-assisted screw placement and decompression was greatly reduced. Due to the relatively narrow operating space in minimally invasive surgeries, the nerves may not be clearly exposed during operation. Therefore, less experienced surgeons are more likely to cause nerve irritation symptoms. In this study, one patient in the robot-assisted MIS-TLIF group and one patient in the open surgery group showed transient numbness on the dorsum of the foot. As we considered that it may be related to nerve irritation, the numbness relieved after neurotrophic treatment. As robot-assisted surgeries do not require the exposure of anatomical markers, the learning curve is much shorter than general minimally invasive surgeries. Therefore, robots are helpful in minimally invasive surgeries. Although the duration of surgery was slightly longer, this technique combined the precise positioning of robot systems with minimal tissue damage and could achieve less pain and less adjacent segment degeneration. These features will enable less bleeding, quicker recovery, more accurate screw placement, less damage to paraspinal soft tissue, less surgical scar, and higher clinical satisfaction. As all new techniques will have a learning curve, the coordination between the surgeons and robots will take some time. After mastering this technique, the duration of surgery of robot-assisted MIS-TLIF might be similar to traditional open surgery, or even shorter.
Limitations of this Study
Limitations of this study included a small sample size and that subgroup analyses exploring the effect of patients' baseline demographic and clinical variables on the outcomes were not performed. These analyses are important and need to be included in future further research.
Conclusion
In the treatment of lumbar spondylolisthesis, robot-assisted MIS-TLIF may lead to more precise screw placement, less intraoperative blood loss, less postoperative pain, quicker recovery, and less paraspinal muscle atrophy than traditional open surgery.